In the first of our series on Highlights from North York General’s Emergency Medicine Update Conference 2015, Dr. Kylie Booth discusses Backboard and Collar Nightmares. The idea that backboards and c-spine collars prevent spinal cord injuries came from level 3 evidence in the 1960’s and there has never been an RCT to prove this theory. In fact a Cochrane review on the topic in 2007 concluded that “the effect of pre-hospital spinal immobilisation on mortality, neurological injury, spinal stability and adverse effects in trauma patients remains uncertain” and that “the possibility that immobilisation may increase mortality and morbidity cannot be excluded”. There have subsequently been several observational studies that describe increased morbidity and mortality associated with backboard and collars in a subset of patients. Dr. Booth argues that the time has long past that a major paradigm shift needs to occur toward a safer more rational use of backboards and collars in our trauma patients.
Written Summary and Blog Post prepared by Dr. Kylie Booth and Anton Helman May 2015
Cite this podcast as: Booth, K, Helman, A. Backboard and Collar Nightmares from Emergency Medicine Update Conference. Emergency Medicine Cases. May, 2015. https://emergencymedicinecases.com/backboard-and-collar-nightmares-emergency-medicine-update-conference/. Accessed [date].
The risks associated with Backboard and Collar
The NUMBERS: In North America – over 1 million patients/year are evaluated for potential spinal injuries.
Approximately 2% actually have injuries and <1% have spinal cord injury.
The THEORY/ The MYTH: If we immobilize our patient, we prevent movement, and thus prevent worsening
neurologic outcomes.
As practitioners we all fear worsening injury, causing harm, being sued. No one wants to be the outlier that isn’t
providing ‘gold standard care’.
However, backboards and collars are not without risk:
1) Time intensive to apply, thus increasing time to definitive care
2) Create ‘difficult airway’ scenarios
3) Have been shown to increase mortality 2 fold in penetrating injuries
4) Quickly (~30minutes) cause pressure ulcers; and while we may consider pressure ulcers as a ‘minor’ injury vs.
the catastrophic (and theoretical) concept of a worsened neurologic outcome – in fact, decubiti are the leading
cause of morbidity and mortality in spinal injured patients.
5) Very uncomfortable, and will alter patient’s physical exam often resulting in unnecessary radiographs, thus
exposing patients to unnecessary radiation and increased length of stays in our departments.
6) Increase intracranial pressure (ICP) by restricting venous flow, thus potentially worsening neurological
outcomes.
Patients who are at high risk for spinal injury are the same patients at risk of traumatic brain injuries. There are two sides to the coin:
A: The biomechanically and neurologically unstable injury may get worse with movement
B: The biomechanically stable but neurologically fragile (TBI) will get worse with delays to resuscitation, and suffer from increased ICP from C-collar
What should we use the backboard and collar for?
A Backboard is:
- an extrication device
- a hard surface for CPR
BUT…it has NEVER been proven to provide spinal protection!
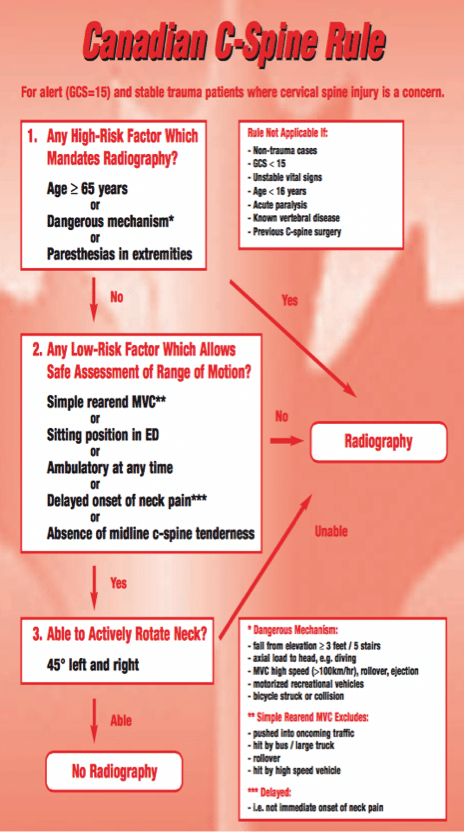
A c-spine collar is useful when applied to those patients who meet the Canadian C-spine Rules. Vaillancourt et al suggest that ~40% of all very low-risk trauma patients could be transported safely WITHOUT C-spine immobilization.
ACEP Guidelines on EMS Management of Patients with Potential Spinal Injury, 2015
“Spinal motion restriction should be considered for patients who meet validated indications such as the NEXUS criteria or Canadian C-Spine rules. Spinal motion restriction should be considered for patients with plausible blunt mechanism of injury and any of the following:”
- Altered level of consciousness or clinical intoxication
- Mid-line spinal pain and/or tenderness
- Focal neurologic signs and/or symptoms (e.g., numbness and/or motor weakness)
- Anatomic deformity of the spine
- Distracting injury
Link to ACEP Guidelines
Note that the concept of ‘Distracting Injuries’ that is present in the NEXUS C-spine decision instrument is subjective and unreliable and some experts believe should be abandoned. In an awake and alert patient, clinical exam is sufficient and will allow reduction in radiographs.
Evidence for selective use of the backboard and collar
Will there ever be an RCT? Likely not; however, we do have some good evidence:
- An international study of 454 patients with blunt spinal injuries compared those transported in the USA with full
immobilization and in Malaysia with no immobilization – there was no difference in neurological outcomes.
(Hauswald, 1998) - In 2005, a large prospective cohort study looked at selective immobilization by paramedics in 13,357 patients, 415 (3%) of which had cervical spine injuries. Thirty-three of the 415 patients with spine injuries were not immobilized, none of which sustained a spinal cord lesion (Domeier, 2005)
- In a retrospective review of 861 records of patients transported to a trauma centre in California after application
of a selective immobilization strategy, and subsequently discharged with the diagnosis of cervical spine injury.
Five injuries were missed by their C-spine clearance protocol, one of which resulted in an adverse outcome.
They concluded: immobilization protocol is 99% (95% CI, 97.7% to 99.7%) sensitive in identifying patients with cervical injuries for immobilization. Those patients not identified were at extremes of age. These results
suggest that selective immobilization may be safely applied in the out-of-hospital setting but should be used with
caution at extremes of age. (Stroh, 2001) - In Canada, the Canadian C-Spine Rule (CCR) was validated for paramedic use in a study by Vaillancourt et al in
2009. The formal safety evaluation study publication is expected soon. EMS in the city of Calgary and the
province of Nova Scotia are currently using the CCR. Most other Canadian EMS are awaiting further safety
evaluation studies before implementing such a program.
A call to change the ‘backboard and collar for all’ paradigm
Prehospital and hospital based practices (including EMS, BLS, ACLS, ATLS) must change.
Encourage the Ministry of Health, local EMS/base hospital and physician providers to change standard protocols
that require all to be immobilized.
Educate colleagues re: evidence (or lack there of!) and use validated Canadian C-spine Rules to guide practice.
The ED should be a NO-BB zone! The backboard is an extrication device only! Encourage EMS to transport on
their cots, and if they do arrive with BB, ask EMS to safely transfer patient from the backboard to stretcher on a
slider, minimizing movement and have EMS take the BB with them!
Draft ILCOR Cervical Collar Guidelines February 2015, Full PDF
Quote of the Month
One of the first duties of the physician is to educate the masses not to take medicine
– William Osler
References
- Stone, M. et al. The Effect of Rigid Cervical Collars on Internal Jugular Vein Dimensions. Acad Emerg Med. 2010;17:100-102.
- Ham, W. et al. Pressure ulcers from spinal immobilization in trauma patients: A systematic review. J Trauma Acute Care Surg. 2014;76: 1131Y1141.
- Kwan, I et al. Spinal immobilisation for trauma patients. Cochrane Database Syst Rev. 2001;(2):CD002803.
- Engsberg, J. et al. Cervical spine motion during extrication. J Emerg Med. 2013,Vol 44, No.1; 122-127.
- Domeier RM, Frederiksen SM, Welch K: Prospective performance assessment of an out-of-hospital protocol for
selective spine immobilization using clinical spine clearance criteria. Ann Emerg Med 2005, 46:123-131. - Hauswald, M. A reconceptualisation of acute spinal care. Emerg. Med. J. 20. 720-723, 2012. Full PDF
- Hauswald, M. Out-of-hospital spinal immobilization: its effect on neurologic injury. Acad Emerg Med. Mar, 1998;
5(3):214-9. Abstract - Haut, ER. Spine immobilization in penetrating trauma: more harm than good? J Trauma. Jan, 2010; 68(1):
115-20. - Shafer, JS, et al. Cervical spine motion during extrication: a pilot study. West J Emerg Med. 2009,10(2): 74-78.
- Stroh G, Braude D: Can an out-of-hospital cervical spine clearance protocol identify all patients with injuries? An
argument for selective immobilization. Ann Emerg Med 2001, 37:609-615. - Sundstrom, T et al. Prehospital Use of Cervical Collars in Trauma Patients: A Critical Review. J.
- Neurotrauma. 2014, 31: 531-540.
- Vaillancourt, C et al. The out-of-hospital validation of the Canadian C-Spine Rule by paramedics. Ann
Emerg Med 2009. 54:663-71. Full PDF - Vaillancourt, C et al. Evaluation of the safety of C-spine clearance by paramedics: design and methodology.
BMC Emerg. Med. 2011, 11, 1. Full PDF - National Association of EMS Physicians and American College of Surgeons Committee on Trauma. EMS Spinal
Precautions and the Use of the Long Backboard. Prehospital Emergency Care 2013; 17: 392.
More FOAMed on Backboard and Collar Nightmares
EP Monthly’s ‘Ditch the Spine Board’ blogpost
Sancrit.com’s ‘The Curse of the Cervical Collar’ blogpost
PHARM: Prehospital and Retrieval Medicine’s ‘Rational for prehospital soft neck collar use’ blogpost
Dr Helman & Dr. Booth have no conflicts of interest to declare





[…] lecture on the non-utility of backboards and collars via Anton Helman and EM Cases. […]
Great episode! I completely agree with everything that was said! As a Paramedic in Ontario my hands are tied by the MOH BLS Standards. Where I work (Ornge) we will use the Scoop to change pressure points, provide more comfort and make it easy to remove once at the receiving to reduce the time on the device. As an aside, we were referred to as EMS personnel or workers in the episode. We are Paramedics. Primary Care, Advanced Care or Critical Care. Thank you! Looking forward to more talks from the EMU Conference!