EM Cases Main Episodes are round table in-depth discussions with 2 or more EM Cases guest experts, inherently peer reviewed, and edited for a podcast.
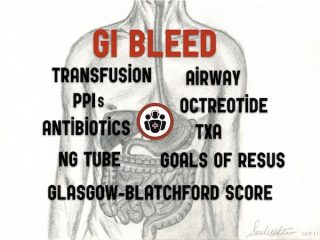
Episode 101 GI Bleed Emergencies Part 1
In this Part 1 of our two part podcast on GI bleed emergencies we answer questions such as: How do you distinguish between an upper vs lower GI bleed when it's not so obvious clinically? What alterations to airway management are necessary for the GI bleed patient? What do we need to know about the value of fecal occult blood in determining whether or not a patient has a GI bleed? Which patients require red cell transfusions? Massive transfusion? Why is it important to get a fibrinogen level in the sick GI bleed patient? What are the goals of resuscitation in a massive GI bleed? What's the evidence for using an NG tube for diagnosis and management of upper GI bleeds? In which patients should we give tranexamic acid and which patients should we avoid it in? How are the indications for massive transfusion in GI bleed different to the trauma patient? What are your options if the bleeding can't be stopped on endoscopy? and many more...