In this episode on Pediatric Syncope & Adult Syncope, Dr. Eric Letovksy & Dr. Anna Jarvis run through the key clinical pearls of the history, the physical, interpretation of the ECG and the value of clinical decision rules such as the ROSE rule and the San Francisco Syncope Rule in working up these patients. We discuss how to differentiate syncope from seizure, cardiac causes of syncope such as Arrhthmogenic Right Ventricular Cardiomyopthy & Prolonged QT Syndrome, and the indications for Holter monitoring, Echocardiograms and stress testing in patients with Syncope.
Dr. Letvosky & Dr. Jarvis answer such questions as: How can we diagnose Hypertrophic Cardiomyopathy in the ED? What is the value of Troponin and BNP in the work-up of syncope? In what ways are patients with Down Syndrome at high risk for serious causes of syncope? In what ways are patients with alcohol dependence at risk for serious causes of syncope? Why is ‘Benign’ early repolarization not a benign condition in patients with syncope? Which children with syncope should be admitted? and many more….
Written Summary and blog post by Claire Heslop, edited by Anton Helman, July 2012
Cite this podcast as: Letovsky, E, Jarvis, A, Helman, A. Pediatric Syncope and Adult Syncope. Emergency Medicine Cases. July, 2012. https://emergencymedicinecases.com/episode-25-pediatric-adult-syncope/. Accessed [date].
APPROACH TO PEDIATRIC SYNCOPE & ADULT SYNCOPE
Key questions:
- Is it truly syncope? (or could it be something else, i.e. seizure?)
- Is the underlying cause serious, or life-threatening? (i.e. cardiac dysrhythmia, MI, GI bleed, PE, SAH, ectopic pregnancy …)Is the patient at high risk for a cardiovascular event, or death?
Major categories of syncope
- Vasovagal: prodrome of nausea, presyncope & sweating; triggered by pain, anxiety, distress, or by prolonged standing or kneeling in a warm and/or crowded place
- Situational: occurs with micturition, cough, defecation; or by carotid sinus pressure (i.e. turning head, shaving), or subclavian steal (i.e. during arm exercises)
- Orthostatic: triggered by BP meds, dehydration, alcohol, & autonomic dysfunction CNS: rarely the cause of syncope as the only symptom
- Cardiovascular: dysrhythmia, structural heart disease or ischemia; clues are family history of sudden/unexplained death, exertional syncope and no prodrome
What are the key clues for serious causes of syncope in a child?
- Family History of sudden cardiac or unexplained death is worrisome. Ask about deafness or pacemaker implantation in younger family members, or inherited metabolic disorders which may indicate a familial cardiac cause.
- Triggers: emotional upset may trigger a benign breath holding spell, while a loud, startling noise may cause syncope in a child with congenital long QT syndrome.
- Always assess children for evidence of non-accidental trauma (abuse), and interview the older child about substance use.
How to differentiate syncope from a seizure
- If there are soft tissue injuries at multiple sites, or if posturing or a rigid (tonic) phase was observed before rhythmic activity (clonus), it more likely a seizure. Both syncope and seizure can cause urinary incontinence, but unlike seizure, patients with syncope return quickly to alertness.
Physical Exam Pearls
- Look for injuries: serious head injuries are possible. Also look for evidence of seizure (bitten tongue, cheeks, multiple bruises).
- Measure orthostatic vitals
- They have higher yield for older pts (1) who may have orthostatic syncope, however, abnormal findings do not rule out other causes of syncope.
- Do a careful cardiac exam
- auscultate for valvular murmurs (i.e. mitral or aortic valve disease).
- **Any outflow murmur that increases with valsalva in syncope is hypertrophic cardiomyopathy (HCM) until proven otherwise!**
- Do a rectal exam for occult blood if a GI bleed is suspected based on history, Hb or hematocrit.
- Other investigations?
- Always do an ECG. Laboratory testing has low yield, so investigate strategically, based on the history and physical. Consider BhCG (ectopic), Hb (anemia), lytes (hypoK, hypoCa, hypoMg),Trop (very low yield in pts with syncope as their only symptom).
- Who needs a head CT?
- Only in adult patients where history or physical suggest SAH,TIA/stroke, or first onset of seizure disorder.
- ED Ultrasound: Syncope preceding or accompanying abdominal pain could be due to an ectopic pregnancy, or a leaking AAA.
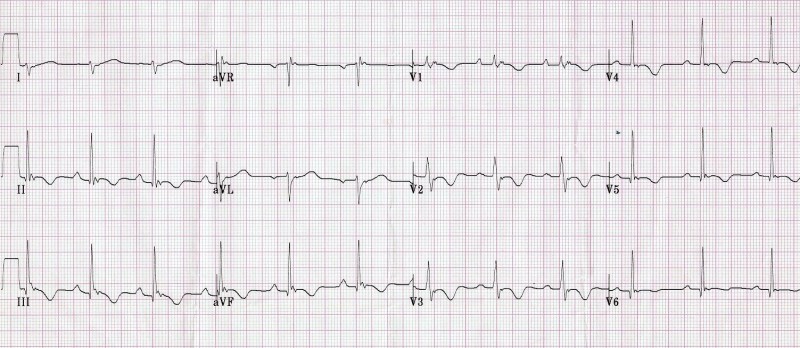
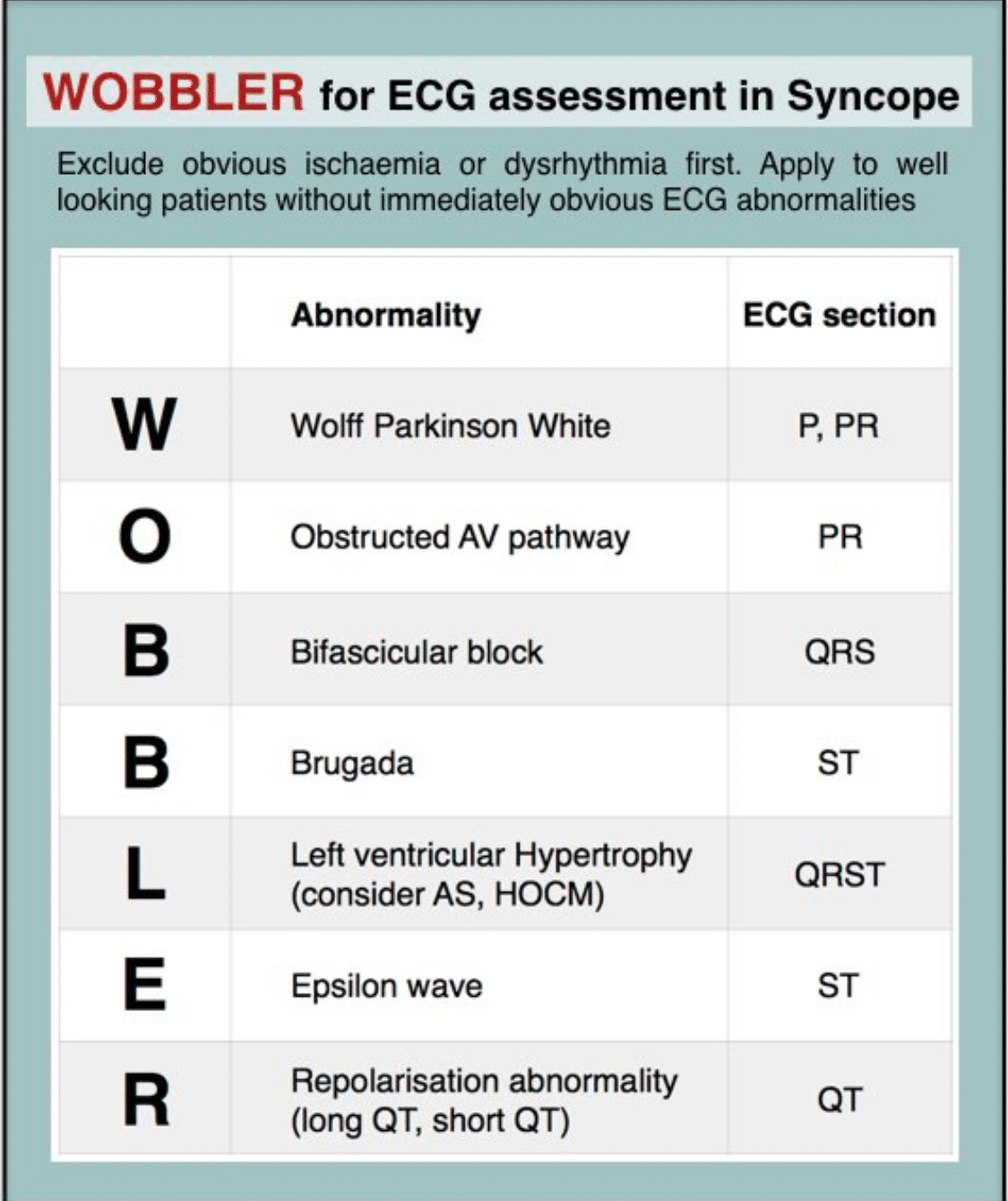
ECG Pearls for Syncope
It’s all about the intervals!
- short PR: WPW
- long PR: AV conduction block
- narrow, deep QRS: HCM
- wide QRS + Epsilon waves: arrhythmogenic RV hypertrophy wide QRS: Vtach,WPW, BBB
- QT interval: long QT syndrome, (also short QT)
Also, look for Brugada, ACS, myocarditis, and PE changes on ECG
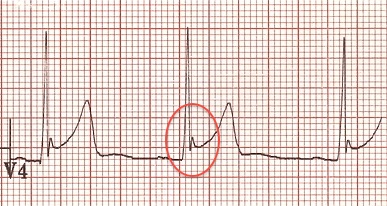
Arrhythmogenic right ventricular cardiomyopathy:
- Genetic disorder leading to fibro-fatty changes, which may result in sudden cardiac death in young people (6).
- Classic ECG findings:
- Inverted T waves in right precordial leads (V1,V2,V3)
- QRS in Lead 1 > 110 msec
- Epsilon waves (low amplitude notches after QRS and before T wave) in right precordial leads (V1- V3)
Benign Early Repolarization:
- Common in young, healthy patients, BER shows a j-point elevation with notching in the anterior leads.
- However, BER pattern in inferolateral leads has been associated with risk for Vfib (7).
- Consider referring these patients to cardiology if they present with syncope.
2016 Update: 10 things to know about the AHA Statement on Benign Early Repolarization
Differential Diagnosis for Syncope
Wolff-Parkinson-White:
- ventricular pre-excitation from accessory conduction, with a short PR and delta wave, susceptible to paroxysmal SVT,Afib,Aflutter, and (rarely) Vfib.
- Avoid nodal blockers!
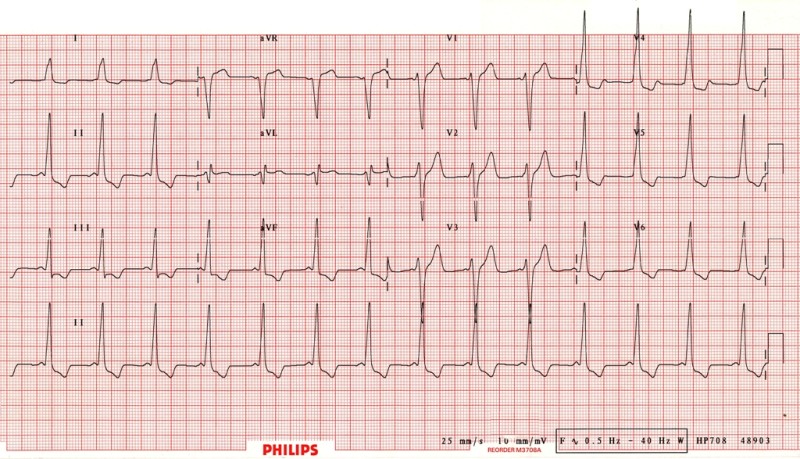
Hypertrophic Cardiomyopathy:
- Genetic disorder of cardiac hypertrophy which can progress to block the LV outflow track.
- ECG findings include increased QRS complex width and voltage, and ST-segment and T-wave signs of LV hypertrophy.
- HCM is the most common cause of sudden death during exercise in young adults and children!
- In young patients, ECG may show Q-waves in leads II, III, aVF,V5,V6.
Prolonged QT Syndrome
- A QTc interval >500 is worrisome (>450 in kids) for high risk for Torsade de Pointes, and sudden death.
Congenital Long QT
- inherited, often with deafness; syncope can be triggered by sudden loud noises or startling events, or spontaneously.
Acquired Causes: (& examples)
- Antiarrhythmics (amiodarone, sotolol)
- Antibiotics (macrolides)
- Antidepressants (TCAs, citalopram)
- Antipsychotics (haldol, seroquel)
- Antihistamines (loratidine, benadryl)
- **Numerous other medications, as well as low K+, Ca+, and Mg+ (due to alcohol abuse, diuretics, malnutrition), myocarditis, hypothermia, methadone, and carbon monoxide, can lengthen the QT segment.**
Short QT Syndrome
- QT≤ 300 ms that does not significantly change with heart rate, tall and peaked T waves, with a structurally normal heart.
Update 2018: A prospective observational study of patients >60 years of age with syncope, showed serious cardiac arrhythmias (non-sinus rhythm; multiple premature ventricular conductions; short PR interval; first degree atrioventricular block; complete left bundle branch block; and ST, T, and Q-wave abnormalities consistent with acute or chronic ischemia) in 3% of patients, that were not recognized at initial ED assessment. Abstract
RISK STRATIFICATION & DISPOSITION FOR SYNCOPE
Who are the high risk patients for recurrent syncope and sudden death?
- While outcomes after discharge from ED for most patients with syncope are generally benign, patients with high risk features (signs of cardiac disease or arrhythmias) need admission for urgent cardiac assessment (2).
Which patients with syncope need an echo?
- Any suggestion of structural cardiac disease based on history, exam, ECG, or exercise-induced syncope, or family history of death, requires an urgent echocardiogram.
What are the indication for a Holter Monitor in a patient with Syncope?
- Holter have very low yield (1–3%), but in an adult patient with frequent episodes, or features suggesting arrhythmogenic syncope, a Holter is indicated (3).
Which patients with Syncope need a stress test?
- Our experts recommend stress testing in patients suspected of cardiac syncope only after an echocardiogram, and consultation with a cardiologist.
What are the indications for admission in patients with Syncope?
- ACEP guidelines for syncope (4) recommend (B level) that these clinical features warrant admission:
- history of CHF,
- history of ventricular arrhythmias,
- associated symptoms of ACS,
- exam evidence of significant CHF,
- exam evidence of significant valvular disease,
- abnormal ECG (ischemia, arrhythmia, BBB, prolonged QTc)
Is the San Francisco Syncope Rule Useful?
- Validation studies show poor sensitivities so our experts do not recommend it’s use as a sole tool for risk stratification.
Risk Stratification Of Syncope in the ED (ROSE)
- The ROSE rule (5) advises admission of a patient with any one of the following:
- BNP >300, Bradycardia <50, Rectal exam showing blood or suspicion of GI bleed, Anemia (Hb<90), Chest pain with syncope, ECG showing Q waves (except in lead III), or Saturation <94% on room air. (Mnemonic: BBRACES)
Medical Short Stay Units for Syncope
- Our experts have found in their practice that prolonged ED observation alone does not have a role, unless a further test (i.e. a cardiac echo) is planned.
Syncope Discharge Instructions
- For vasovagal: avoid known triggers, such as alcohol and warm environments, and maintain adequate hydration, food and sleep.
- To reduce injury: once syncope prodrome starts, lie down, and avoid driving or high risk activities.
For abstract comparing outcomes of syncope vs presyncope go here.
Update 2021: Prospective study of 8,233 adults (>16 years) with syncope at 11 Canadian ED’s from 2010-2018 using the Canadian Syncope Risk Score (CSRS). Found < 1.0% of very-low and low-risk patients had any serious outcome at 30-days; CSRS suggesting that very-low and low-risk patients may be discharged, with discussion regarding investigations/disposition for medium-risk patients, and high-risk should be hospitalized. Abstract
For more on syncope on EM Cases:
Best Case Ever 10: Pediatric Syncope
Key References
Mendu, M et al. Arch Int Med. 2009;169:1299.
Sheldon, R et al. Can J Cardiol. 2011;27:246.
Moya, A et al. Euro Heart J. 2009;30:2631.
ACEP Clinical Guidelines. Ann Emerg Med. 2001;37:771.
Matthew, J et al. JACC. 2010;55:713.
Hulot, JS et al. Circulation. 2004;110:1879.
Haissaguerre, M et al. NEJM. 2008;358:2016.
Dr. Letovsky, Dr. Helman and Dr. Jarvis have no conflicts of interest to declare
For more EM Cases content on Pediatric Emergencies check out our free interactive eBook,
EM Cases Digest Vol. 2 Pediatric Emergencies here.
For more Pediatric EM learning visit trekk.ca – Translating Emergency Knowledge for Kids (TREKK) is a growing network of researchers, clinicians, health consumers and national organizations who want to accelerate the speed at which the latest knowledge in children’s emergency care is put into practice in general EDs – rural, remote or urban.






Leave A Comment