Disaster medicine is the “universal subspecialty”. Why? Because all physicians could be called upon to help their communities in times of crisis, and because disaster medicine is the ultimate team sport. Emergency Medicine is particularly well suited to take a lead in disaster medicine. We own this.
A medical disaster is the response to an event that by definition is going to outstrip the resources you have. However, what constitutes a disaster may differ depending on hospital resources, the time of day, whether or not the hospital has been damaged by the disaster itself, and whether or not the impact of the disaster is contained or not.
In this EM Cases podcast, with the help of Laurie Mazurik, Daniel Kollek and Joshua Bezanson we will help you become familiar with a general approach to mass casualties, how to handle critical infrastructure disruption in your ED, management of biohazards including airway management, chemical hazards including decontamination and finally evacuation principles in the case of a natural disaster…
Podcast: Play in new window | Download (Duration: 1:32:32 — 84.8MB)
Subscribe: Apple Podcasts
Podcast production by Joshua Beznason & Anton Helman, sound design & editing by Anton Helman
Written Summary and blog post by Anton Helman, edited by Daniel Kollek & Laurie Mazurik Sept, 2017
Cite this podcast as: Helman, A, Mazurik, L, Kollek, D, Bezanson, J. Disaster Medicine. Emergency Medicine Cases. September, 2017. https://emergencymedicinecases.com/disaster-medicine/. Accessed [date].
Initial general approach to mass casualties in disaster medicine
1. Confirm that there are emergency casualties and get an estimate of the number of casualties.
2. Team huddle: Share the information that you have with your team.
3. Notified the hospital administrator on-call who will activate a hospital wide disaster plan (in Canada, a code Orange) so that all departments can halt all non-essential services, conserve resources, and prepare for the surge.
4. Deactivate nonessential and non-emergency services in order to create capacity.
TDAD SAD mnemonic for disaster medicine preparedness
When the surge arrives in your ED:
Triage & Treat: Triage only CTAS (in Canada) or SALT (see below) 1 (red) and 2 (yellow) patients into the ED. Divert CTAS 3-5 or SALT Green to a non-ED area for assessment; preferably a family practice unit or urgent care unit. See the SALT categories and algorithm below.
Discharge: Make an immediate determination about which patients are safe to be discharged from the ED either home or to another part of the hospital. This starts before people arrive and continues throughout the surge. Keep your discharge review cycle short e.g. round q1-4hrs to identify those ready for discharge.
Admit: Any patients requiring admission in the ED go expeditiously to hospital floors and if necessary become their “hall” patients if no beds are available. All hospital floors should have a plan for surge capacity and open areas or increase the number of patients per room etc. in order to alleviate pressure on the ED.
Demand: Demand that the rest of the hospital become involved. All departments need to open their plans for active participation in the disaster code.
SAD:
Spend less time per patient.
Ask for less things to be done. Know who should get what. Be a minimalist and be extremely selective when ordering tests and blood products so as not to overwhelm the lab, blood bank and radiology departments and to expedite patient care as efficiently as possible.
Don’t do anything. Know when not to investigate or treat because the patient is either very unlikely to survive and/or they do not need emergency treatment.
This is an adaptive process that requires flexibility and a staged cascade of events rather than a rigid all-or-none situation. TADAD SAD fits best with a mass trauma event, but can also be applied to chemical, biological or radiological-nuclear events.
The 4 phases of the disaster medicine cycle
- Planning and mitigation – a formal risk assessment needs to take place before a disaster hits to assess those disasters that have either a high probability of happening or have a high impact if they occur.
- Preparedness – practice disaster scenarios with simulation exercises.
- Response phase – execute the plan and adapt it to the particular disaster.
- Recovery phase – restore your previous functionality and review what happened and how to do it better for the next disaster.
Factors that predispose the health system to the vulnerabilities of a medical disaster situation: The disaster comorbidities
Think of the health care system like a person and the effects of a disaster like a stroke.
The co-morbidities that predispose the health care system to a stroke: First, overcapacity is a chronic problem not only in most EDs but also ICUs, medical and surgical units. The more overcrowding in these units prior to a disaster, the more vulnerable your system is. Next, is the notion of tunnel vision, which occurs when a clinical team focuses ONLY on their patient(s) and advocates so hard for them that they consume resources that should be used for others who have better chance of survival. Tunnel vision can affect the patient outcomes across a health system and cause greater morbidity and mortality.
When the disaster (stroke) occurs, dysarthria or aphasia is often the first sign. This is the inability to communicate situational awareness to both medical staff and the public when a critical incident begins to unfold. Second is asymmetric weakness: There will always be a hospital or region that will be crippled first and fail.
The impact of these factors can be catastrophic, but not impossible to address. The only clot buster we have is money/resources and that does not always work. Addressing overcrowding and tunnel vision (my patient before others) is an ongoing day-to-day struggle. The low hanging fruit, is learning to be more health system aware, understanding how tunnel vision and overcapacity is detrimental and practicing interprofessional communication skills.
Triaging mass casualties in disaster medicine: SALT
The SALT triage framework stands for Sort, Assess, Lifesaving maneuvers, Treat
SALT Triage Categories

SALT triage categories
SALT Algorithm for triaging mass casualties at the scene
While the goal of triage for mass casualties in the field is to prioritise evacuation, the goal of triage in the ED is to prioritize treatment and user resources.
Surge Capacity in Disaster Medicine
Surge capacity is the ratio of patients to medical beds, staff and consumable resources. Scale up your ED’s capacity in the following ways:
- Be selective in which patients require medical beds and treatment.
- Be selective in which tests are required and how much blood product is ordered.
- Call in additional staff in tiered shifts with specific pre-assigned roles.
- Stockpile consumable resources beforehand.
- Consider where to expand by adding extra beds, who will staff them and where to get supplies.
Learn more about surge capacity strategies in Episode 138 COVID-19 Part 2- ED Surge Capacity Strategies in the COVID-19 Pandemic
Biohazards and Bioterrorism Disaster Medicine
When to suspect a potential biohazard or bioterrorism event
One of the more difficult and essential aspects of biohazard disasters is recognizing them in the first place. The factors indicative of a biohazard include:
- Multiple simultaneous patients with similar clinical syndrome (as in a household of people exposed to carbon monoxide)
- Severe unexplained illnesses, especially among the young and otherwise healthy
- Predominantly respiratory symptoms
- Unusual (non-endemic) organisms
- Unusual antibiotics resistance
- Atypical clinical presentation of disease
- Unusual patterns of disease such as geographic co-location of victims
- Intelligent information – tips from law enforcement, discovery of delivery devices, etc.
- Reports of sick or dead animals or plants
General approach to safety in a biohazard disaster
STEP 1 Protect yourself and others
Distance. Immediately step back at least 2 meters and don an N95 mask, gown, gloves and face/eye protection. Do not touch the patient. Without touching them, give them a surgical mask to wear and ask them to clean their hands with hand sanitizer. Explain why your are taking these precautions. Tell them to wait where they are provided they are isolated from others.
STEP 2 Call for help
Not overhead or by shouting. You don’t want people coming to you. You want them to stay away from the biohazard.
Call the RN/MD on duty. Explain what the situation is and ask them to prepare a room to isolate the patient in as well as a path to get them to the room without exposing others.
Call for Infection Control and ID. If you don’t have Infection Control or ID where you are, go through your local expert link system to reach them. If you have people trained in advanced PPE Training and Equipment e.g. a Powered Air Purifying Respirator (PAPR), call them.
If the patient does not need immediate intervention let them wait while you get the support you need and feel confident that you are safe.
STEP 3 Isolate the patient
Biohazard patients need to be in a room with a solid door that can be closed, preferably with negative pressure. If it has it’s own bathroom that is best as you don’t want this patient leaving the room. Put up the signs on the door for people not to enter.
Do’s and Don’ts of airway management in the biohazard patient
Do’s in biohazard airway management
- Only you (inutbator) and assistant (RT preferably) in the room.
- Wear the most advanced PPE you have.
- Have all your difficult airway tools ready.
- Paralyze the patient. If they can’t cough on you, your risk is lower.
- When you doff PPE have a trained observer watch you do it so if you accidentally contaminate yourself they will see it and tell you. Go shower and put on new greens.
- Once intubated put a filter on the ETT.
- Consider yourself quarantined until the biohazard has been definitively identified.
Don’ts in biohazard airway management
- Don’t bag the patient. Put on nasal prongs at flush and NRB.
- Don’t use nebulizers.
- Don’t expose others until biohazard has been definitively identified.
Listen to Dr. Mazurik’s Best Case Ever Biohazard Preparedness: The Protected Code Blue
Decontamination in suspected chemical threat disasters
Expect a 5:1 of unaffected:affected casualties.
After you have isolated the patient(s) without touching them you can direct them through the decontamination process:
Step 1: 3 D’s.
Disrobe: Removing contaminated clothing if there was an aerosol, liquid or particulate exposure will remove up to 80% of it. Have the patient put contaminated clothing in a plastic biohazard bag and label the bag with the patient’s name and contact information.
Dry decontamination: Provide towels for dry decontamination. With liquids and solids the patient should “blot” off the contaminant rather than rub as rubbing may further push it into the skin.
Don a clean gown or coverall and wait for wet decontamination.
Less commonly available material that adsorb skin contaminants are Fuller’s earth or products that neutralize selective skin contaminants such as Reactive Skin Decontamination Lotion which often reserved for CBRN (Chemical, Biological, Radiological and Nuclear) Teams. If there is a powder exposure, consider vacuuming.
Step 2. Wet Decontamination.
The solution to pollution is dilution!
This is simply showering for 5 minutes with a mild soap and then donning clean clothing afterward.
Most facilities are limited in their showering capacity, which is why the 3 D’s (which remove most of the contaminant) are so critical.
Chemically exposed patients who need physical assistance pose a high risk.
If patients need physical assistance to decontaminate and/or require active patient care, you should not assist them unless you have appropriate PPE. In an unknown exposure, this means advanced PPE such as a chemical suit and air purifying respirator. If you know the exposure poses no threat to you e.g. gas exposure, you may approach the patient with lower levels of PPE.
Those who need assisted wet decontamination, should have this carried out by those in advanced PPE, trained in technical decontamination. Your hospital should have a technical decontamination plan.
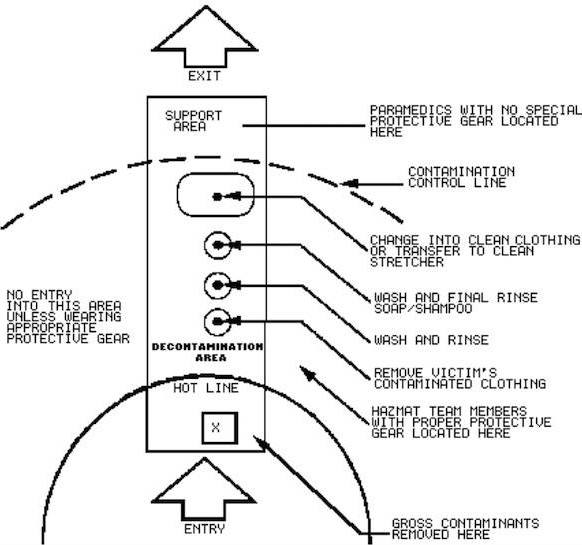
Decontamination set up. Flow is only in one direction; nobody goes against the arrows.
ED evacuation and transport considerations in the natural disaster situation
In the event of a natural disaster such as a hurricane with flooding, ask yourself:
- What is the magnitude of the natural disaster?
- Is it contained?
- How has the natural disaster impacted other hospitals in the region? Consideration should be given to evacuating the most heavily hit hospitals by the natural disasters and having a higher threshold to evacuate the less heavily hit hospitals.
- Who is the patient load? If electricity in your ED is at risk of an outage think of 3 types of patients first: ventilated, paced, those in the midst of a procedure.
- If the ED is evacuated, what is the destination? There should be a pre-determined location in your hospital disaster plan.
- How are the patients going to be transported to the new destination and in what order? The sickest and most resource intensive patients should be evacuated first, however consideration should be given to shelter in place if the risk of transport is anticipated to outweigh the risk of staying.
- What services need to be maintained during transfer and reception? Ventilation, sedation and analgesia are usually first priorities.
- Do you have forensic and/or psychiatric patients that require security staff to be transferred with them?
- How will you ensure that each patient’s medical record will be transferred securely?
Quote of the Month
We don’t rise to the occasion. We fall to the level of our training.
For more on disaster medicine on EM Cases:
Best Case Ever 61 Biohazard Preparedness: The Protected Code Blue
References
Ciottone, G. R. (2016). Ciottone’s Disaster Medicine. Mosby Elsevier.
National Association of Emergency Medical Technicians (2016). All Hazards Disaster Response Course Manual.
Walter, F. G. (2016). Advanced Hazmat Life Support Provider Manual 4th edition (AHLS).
CAEP/CEEP (2013). Position Paper on Healthcare Facility and Agency Disaster Preparedness in Canada. Available online: http://www.ceep.ca/resources/HCF_&_Agency_Preparedness_Position_Paper_-Final.pdf
Kollek, D. (2013). Disaster Preparedness for Healthcare Facilities. Mcgraw-hill.
Richards CF, Burstein JL, Waeckerle JF, Hutson HR. Emergency physicians and biological terrorism. Ann Emerg Med. 1999;34(2):183-90.
Lillibridge SR, Noji EK, Burkle FM. Disaster assessment: the emergency health evaluation of a population affected by a disaster. Ann Emerg Med. 1993;22(11):1715-20.
Trained observers for donning and doffing PPE. CBME collaborative.
Other FOAMed Resources on Disaster Medicine
Emergency Medicine Blog Lecture Slides On Toxic Gases and An Introduction To CBRNE Weapons
Disasters by Sean Rothwell on Life in the Fast Lane
Dr. Mazurik’s Best Case Ever Biohazard Preparedness: The Protected Code Blue
St. Emlyn’s EM Blog How to declare a Major Incident
Drs. Helman, Bezanson, Kollek and Mazurik have no conflicts of interest to declare
Now test your knowledge with a quiz.






Great topic, thanks.
Which speciality do you call for advice with biological or chemical disaster?
For biological call Infection Control and/or ID. For chemical call Tox. For both, also call hospital administrator to activate disaster plan.
Listened to this the day before the Vegas shooting. Let’s hope we never have to use it. Thanks for the good topic. Makes me feel a bit better if that day ever comes.
What is the name of the song at the end? I love it! Also, I loved the podcast! I am premed right now, while working as a Paramedic, and am hoping to specialize in emergency medicine. Listening to all of the information you all have is endlessly interesting. Thank you!