In Emergency Physician Speed How Fast is Fast Enough – Part I, Dr. David Petrie addressed the issue of physician productivity (patients per hour, or PPH), the many factors that influence how quickly emergency physicians can process patients, and some of the tradeoffs between speed and quality. He also discussed the processing rate of the entire ED and introduced the concepts of surge capacity and the effect of crowding on safety if the ED can’t keep up. In this follow-up blog, Dr. Petrie expands on the departmental aspects of throughput and safety, and calls on policy-makers to recognize the need to include surge capacity in planning efforts. He also makes some powerful arguments about the related issues of so-called ‘inappropriate visits’ and the changing role of the ED. In this post – Emergency Physician Speed Part 2 – Solutions to Physician Productivity , he also brilliantly dismantles some common myths about ED visits — and drivers of costs.
Dr. Petrie remarks in several places on CTAS levels; in Canada we use a five-level triage system known as the Canadian Triage and Acuity Scale. Level I is the highest acuity (life-threatening presentations needing immediate attention). Many people, including policy-makers, confuse triage level with appropriateness and consider CTAS IV and V level arrivals to be best seen somewhere else, despite the fact the scale was not designed to measure appropriateness. Most often the CTAS III patient — someone well enough to wait a bit, but too sick to be assessed in a chair — faces the longest wait to be seen, with stretcher availability usually being the bottleneck to flow. Full information on the CTAS scale can be found at: http://caep.ca/resources/ctas.
I hope to address controversies in triage in a future blog. Dr. Petrie also touches on some issues in funding physicians for ED work; if not designed properly, the funding system can create a situation where the financial interests of the physicians are at odds with those of the ED and a safety agenda. I will go into that in more detail in a future entry, as well.
—Dr. Howard Ovens
Finding solutions to the patient-per-hour productivity question in emergency medicine
“How we formulate the problem is far more essential than the solutions.”
– Albert Einstein
As I explained in Part I of this blog, there are patient per hour (PPH) productivity tradeoffs that must be considered in managing the operations of an emergency department. For example, when considering PPH rates for an individual emergency physician (EP), it makes sense to optimize speed in a way that maintains quality and safety for the individual patient, but also ensures that reasonable flow is maintained in the interest of those waiting to be seen. However, though speed should be optimized at the individual level, when considering the problem from the departmental planning level, over a longer period of time, a safety margin should be built into the PPH expectations in order to meet the unpredictable but inevitable surges in patient demand created by the variability in patient arrival patterns. Policy-makers who design systems that are dependent on all EPs seeing new patients all-out, all the time (i.e., 100% utilization) miss this patient safety point.
When this productivity/quality conundrum is seen through a queueing theory lens, the problem becomes clearer — as do solutions. In fact, this is a known but hidden inefficiency problem of Volkswagian proportions (even worse when you consider the immediate patient outcome ramifications) in the operational management of hospitals and EDs.
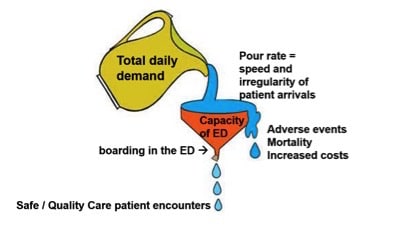
Figure 1 schematically illustrates the fundamental relationship between demand, the variability of arrival and capacity in any ED. If capacity is determined by planning for the average day (see Part I), and that capacity is further reduced by inefficiencies caused mainly by boarding in the ED1,2,3,4 (though many other throughput inefficiencies can contribute, including inadequate EP coverage driven by unrealistically high PPH expectations), then we end up with “poor flow” and all the other complications of demand/capacity mismatch predicted by queueing theory.
So, practically, what can we do about this in a way that meets the aims of improving patient outcomes and experiences while also recognizing and balancing the cost implications that may threaten the sustainability of the system? Well, the answer is: It depends. That is, context is everything, and the best way to staff and manage an individual ED likely depends significantly on overall volumes, the degree of variability in the busy-ness of any day, and how large and persistent is the boarding problem in the ED in question. Exactly what works best should be prototyped, mathematically modelled if possible, rapidly iterated, implemented locally, evaluated for value (patient outcomes/cost)5, peer-reviewed, and adapted by similar EDs more generally if it is shown to work.6
Planning for the 75th-percentile day
As discussed in Part I of this blog, planning for the average day in emergency medicine is like pitching your tent at the average tide line, or walking across a river with an average depth of five feet, and wondering why we are in over our heads. As a provocative best guess, I would suggest that in a high-volume, urban teaching hospital ED the more patient-centred (and potentially more cost-sustainable over the long run) operational readiness target (including staffing levels) should be for the 75th-percentile day.
- Potential benefits: The primary and most obvious benefit would be improved patient outcomes. Seventy-fifth-percentile readiness would reduce wait times overall7 and therefore presumably improve patient experience and patient outcomes. Experience would suggest that revving up capacity by 25% in the short term is possible; but beyond this, and especially over longer periods of time, there is a sense of feeling overwhelmed that leads to worse patient outcomes and provider cynicism, disengagement, and burnout.
Seventy-fifth-percentile readiness would also build in more operational flexibility8 within the ED to adapt to the variability that is seen in hour-to-hour demand, including variation between patient arrivals for the resuscitation area versus the undifferentiated Canadian Triage & Acuity Scale (CTAS) III area (which says urgent cases are to be seen within 30 minutes), or the balance between the patient intake versus the reassess/disposition decision functions. Flex shifts could better cover flexible tracks9 and flex to the greatest need10, depending on the day. This includes flexing to adapt to boarding dysfunction and its impact on ambulance offloads11 and dissatisfaction among patients in the waiting room.
The potential secondary benefits may include what can be done during the “slowest” quartile days. That is, rather than treating those slowest quartile days (or shifts, or hours) as down time, they could be seen as an opportunity to do many other things that add value besides assessing and treating the next patient in the intake queue. For example, this time could be used for so called in-situ simulation training, interprofessional education sessions, and team building. Following up on lab and diagnostic imaging reports with patient calls also can be made more timely.
- Potential risks: The primary and most immediate risk would be the increase in costs to the system. These costs would come mostly in the form of staffing costs, though with the non-linearity of the utilization/wait time curve, small decreases in percent utilization can have a big impact on reducing wait times.12 In other words, there could be a relatively big bang for a relatively small buck. And, theoretically, these costs may be more than offset by reducing wait times, as this should reduce adverse events and mortality.
By preparing for the 75th-percentile day, there are also potential savings to be had in reducing overtime or call-back hours; by reducing nursing education hours, which must otherwise occur outside of shift times; and by potentially reducing sick time, burn out, and recruitment/retention costs for all ED health-care providers over a longer period of time. This is speculative, but it may be worth modelling or piloting this operational approach and evaluating it to determine its impact.
The dynamics and pressures on paying EPs to staff a 75th-percentile day would be different in a pure hourly rate system compared with a pure fee-for-service (FFS) context. In an hourly rate ED, the tension would be around determining how many hours/day equals the 75th-percentile and ensuring that all of the non-direct patient-care responsibilities are being delivered. In an FFS environment there would likely be tension around the fact that a 75th-percentile day will actually reduce the per-shift compensation, especially if some of the value-added deliverables discussed above are not incentivized, either in a fee schedule or secondarily through an internal practice plan. Perhaps the Holy Grail in this circumstance would be an ingeniously balanced blended model of payment that assures an hourly rate for the ED readiness provided and incentivizes the right actions within shift time.
The acuity/schedule-ability fallacy, and its implications to EM system design and planning
Taking the safe redundancy line of reasoning one step further, it is impossible to consider a 75th-percentile day without a reformulation of the often confused debate around “inappropriate visits” to the ED. Again, this seems to be counter-intuitive to policy-makers and the public. What we do know is that low-acuity patients using the ED have very little to do with wait times and ED access block. This has been demonstrated over and over in the peer-reviewed literature.13,14,15
We also know that low-acuity patients seen in the ED contribute very minimally to overall costs.16 The myth that the ED is “the most expensive place in the system to receive care” likely is due to the misunderstanding of how costs are calculated in ED operations. In a classic NEJM article17 analyzing costs attributable to the ED, it was demonstrated that the fixed costs required to staff and equip a modern ED to meet the acute illness and injury needs of a community (the so-called real emergencies) account for the vast majority of the costs, and the marginal costs of seeing one more low-acuity patient are very, very low —perhaps the cost of a Band-Aid.
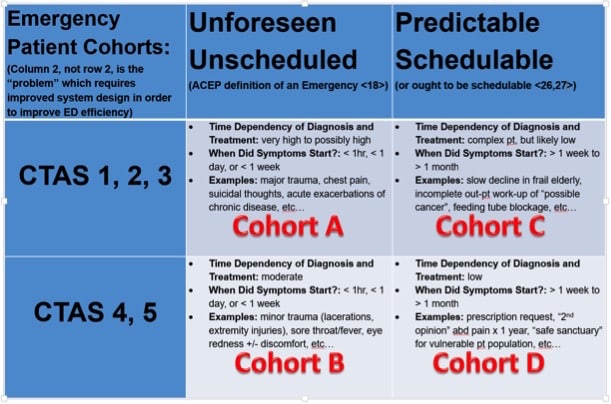
Given this, it is worth considering the 2×2 table in Figure 2, which divides ED patients into four different cohorts and moves away from the counterproductive “real emergency versus shouldn’t be there” false polarity. In the table, the two rows are divided into “high” and “low” acuity, and the two columns are differentiated by the definition of whether a patient visit is considered an emergency or not.18
Figure 2: The Acuity / Schedule-ability fallacy In this reformulation of the “who should be in the ED” debate, Column 1 (cohorts A and B) can reasonably considered appropriate patients for an ED, regardless of their CTAS. Cohort C patients (often triaged on initial quick assessment as a CTAS III because of complexity, not necessarily acuity) are a growing patient population due to an inability to access same day/same week appointments for primary or specialist care. Cohort D patients represent a very small proportion of visits to an ED, and of this small proportion many are from a vulnerable patient population – which is an important safety net role that the ED plays in the system. Unfortunately we have spent millions of dollars in failed attempts19,20 to solve the wrong problem (row 2), and have not adequately designed and integrated our primary care and specialist referral system to handle column 2 patients.21
Risk and patient safety – why some ‘avoidable’ visits are appropriate uses of the ED
This 2×2 table also speaks to the Family Practice Sensitive Conditions (FPSC) methodology that has been used to provide a framework for understanding “potentially avoidable ED visits.”22 The FPSC methodology is based on a documented final diagnosis that theoretically could have been made in a family practice office (if one were available 24/7/365) when the patient was concerned about an unexpected health event. This type of analysis has both merits and limitations. 23,24
Risk is assessed in the moment of decision, looking forward (not backward), often with limited information, and patient perspectives are important. When a parent is awoken by a crying febrile child in the middle of the night, their worry about the risk of serious infection is lost in the FPSC methodology, which classifies the eventual diagnosis of a viral upper respiratory infection as an FPSC — and a visit that potentially should not have gone to the ED. Likewise, if five out of 10 chest pain patients have in retrospect FPSCs such as esophageal reflux, costochondritis, or anxiety, this doesn’t mean the visit and work-up testing in the ED was unnecessary.23,24 I hope the 2×2 table helps to parse out this unreliable “retrospectoscope” phenomenon in the context of emergency medicine system design and planning decisions.
The implications to ED operations of this 2×2 table are the following. It can be argued that if we appropriately staffed the ED to see all cohort A patients in a timely manner, as per queueing theory principles (in fact, perhaps it is appropriate to prepare for the 90th-percentile cohort A day) then this would leave the department with some surge capacity (inaccurately referred to as “down time”), which can then be used to see the less urgent, but unforeseen, cohort B patients. So, seeing these unexpected but low-acuity EM patients actually makes the overall operation more cost effective, not less. And as part of the safety net role of the ED, there should also be some safety margin built into our operational readiness that allows the ED to fulfill its important societal obligations to a large proportion of cohort D patients as a “safe refuge and modern-day secular sanctuary” — as described in a recent blog on this website.25
Cohort C, on the other hand, is an interesting and growing patient population that is increasing the demands on, and changing the role of, modern EDs. This quote from a patient, excerpted from a recent federal report on innovation in health care21, perhaps best illustrates the problem: “When you have a serious chronic illness like I do, you have to see specialists in isolation. They never seem to have the full picture and as a result I feel responsible for keeping my own record to carry to each of these appointments. They don’t trust the documents that I carry but currently I am working with a family doctor, a rheumatologist, a respirologist, a gastroenterologist, and a cardiologist. Yet, when I think I am getting into trouble and end up in the Emergency Department, they always want to know why I did not go and see my own doctor. . . . You can’t win as a patient.”
While this quote exposes big problems with the lack of integration in our system, it also highlights the “go-to-the-emerg-if-you-have-problems” default instructions that many primary-care and specialist physicians give, and which many patients understand (and in fact, trust).
Matching resources to the expected role of the ED
The “if-you-have-problems” instructions are absolutely appropriate if there is an acute exacerbation of a chronic problem. However, in this day and age it is often the complexity of a potentially schedulable problem, and not necessarily the acuity, that steers a patient toward the ED. While this may be reasonable in some settings, if that is an expected role of the ED then appropriately matched resources must be made available.
In smaller rural EDs, for example, if it has been determined by geography or a minimum community size threshold that an ED is necessary (but commonly the volumes are low), then having cohort B, C, and D patients seen in that ED might be very cost effective for the system. That is, take advantage of the latent capacity and do not agonize over “inappropriate” visits. But in urban areas where the system may want to invest in reducing potentially avoidable visits to the ED, we should support and integrate available alternatives for cohort C and some cohort D patients. One alternative here would be to redirect cohort C and D patients from the ED triage to same-day, next-day appointments with their own GPs (if the patients have one, and their office is mandated to be managed with advanced access scheduling26,27 to assure same day/next day patient appointments), or a nurse practitioner general practice/system navigation clinic (if they don’t), or on to a specialist day clinic if there is already an ongoing patient care plan in place.
Counter-intuitive planning in complex systems
A recent editorial commentary titled “ED care: available, competent, affordable”16 describes that beyond the most acute resuscitation/stabilization mission of emergency medicine, the evolving health-care ecosystem requires a location for expedited, patient-centred, high-quality diagnostic and therapeutic decision-making while at the same time avoiding hospital admissions whenever possible – and the ED has evolved to fill that niche. The commentary also suggests “it is time to reframe the ED visit, too often viewed as a failure of the Health Care system, as the opposite.”
Ultimately, determining the optimal staffing and PPH approach in an individual ED will depend on policy-makers and clinician decision-makers understanding the value of including surge capacity in their plans; defining the ED’s specific role in the broader health-care ecosystem; rethinking “inappropriate” ED patient visits; and modelling and testing what works best for particular EDs.
Perhaps systems engineer Paul Plsek, the Chair for Innovation at the Virginia Mason Medical Center in Seattle, summarized it best in his plenary address to the Institute of Healthcare Improvement annual forum, titled “Little Hope: How Common Sense Thinking can Lead to a Mess.”28 In his speech, he highlighted the need for a better understanding of how complex inter-dependent systems such as health care behave, and how they often have counterintuitive properties.29,30 His clarion call at that time was that we need a “new common sense.” Emergency physicians can lead the way in what most EM practitioner decision-makers (and likely Einstein) would suggest is a better formulation of the problems.
—Dr. David Petrie
Dr. David Petrie is an emergency physician and trauma team leader at the QEII Health Sciences Centre in Halifax, Nova Scotia. He is the Professor and Head of the Dalhousie Dept. EM, and Chief of the Central Zone EDs in the Nova Scotia Health Authority. David’s primary academic interest includes the teaching and assessment of critical thinking in medical education and the application of complexity science to Health System Design.
References
Affleck, Andrew and Paul Parks, Alan Drummond, Brian Rowe, Howard J. Ovens. Emergency department overcrowding and access block. CJEM. 2013;15(6):359-370
Rabin, Elaine and Keith Kocher, Mark McClelland, Jesse Pines, Ula Hwang, Niels Rathlev, Brent Asplin, N. Seth Truegar, Ellen Weber. Solutions to Emergency Department ‘Boarding’ and Crowding are Underused and May Need to be Legislated. Health Affairs 2012,31(8):1757-1766
Asplin, Brent R. and David J. Magid. If You Want to Fix Crowding, Start by Fixing Your Hospital. Ann Emerg Med. 2007;49:273-274
Innes, G. Sorry-we’re full! Access block and accountability failure in the health care system. CJEM. 2015;17(2):171-179
Porter, Michael E. and Elizabeth Olmsted Teisberg. Redefining Health Care: Creating Value-Based Competition on Results. Harvard Business School Press; May 25,2006: ISBN 978-1-59139-778-6
Brown, Tim and Roger Martin. Design for Action. Harvard Business Review 2015(9):56-64
Vertesi, L. Dynamic model for physician staffing. Presented to the School of Industrial Engineering; 2008 Oct; Toronto.
Ward, Michael J. and Yann B. Ferrand, Lauren F. Laker, Craig M. Froehle, Timothy J. Vogus, Robert S. Dittus, Sunil Kripalani, Jesse M. Pines. The Nature and Necessity of Operational Flexibility in the Emergency Department. Ann Emerg Med 2015;65(2):156-161
Laker, Lauren F. and Craig M. Froehle, Christopher J. Lindsell, Michael J. Ward. The Flex Track: Flexible Partitioning between Low- and High-Acuity Areas of an Emergency Department. Ann Emerg Med 2014;64(6):591-603
Saghafian, Soroush and Wallace J. Hopp, Mark P. Van Oyen, Jeffrey S. Desmond, Steven L. Kronick. Complexity-Augmented Triage: A Tool for Improving Patient Safety and Operational Efficiency. Manufacturing & Service Operations Management 2014;16(3):329-345
Schwartz, Brian. Transfer of care and offload delay: continued resistance or integrative thinking? CJEM 2015;17(6):679-684 Article author query
- schwartz b [PubMed] [Google Scholar]
Sanford, David. How Queueing Theory Can Influence Wait Times. Health Council Canada Video 7
Schull, Michael J. and Alex Kiss, John-Paul Szalai. The Effect of Low-Complexity Patients on Emergency Department Waiting Times. Ann Emerg Med 2007;49(3):257-264
Foley, Matthew and Eric Legome, Maria Raven. Reducing Emergency Department Utilization: Is This the Answer?. Acad Emerg Med 2013;20(10):1062-1063
Myth: Emergency Room Overcrowding is Caused by Non-Urgent Cases. Canadian Health Services Research Foundation 2009
Bernstein, Steven L. ED Care: Available, Competent, Affordable. Acad Emerg Med 2014;21(1):73-75
Williams, Robert M. The Costs of Visits to Emergency Departments. NEJM 1996; 334(10):642-646
Definition of Emergency Medicine. ACEP Board of Directors June 2015.
Bunn, Frances and Geraldine Byrne, Sally Kendall. Telephone consultation and triage: effects on health care use and patient satisfaction. The Cochrane Collaboration 2009;1:1-38
Morgan, Sofie Rahman and Anna Marie Chang, Mahfood Alqatari, Jesse M. Pines. Non-Emergency Department (ED) Interventions to Reduce ED Utilization: A Systematic Review. Acad Emerg Med 2013;20(10):969-985
Naylor, David and Francine Girard, Jack Mintz, Neil Fraser, Toby Jenkins, Christine Power. Unleashing Innovation: Excellent Healthcare for Canada. Report of the Advisory Panel on Healthcare Innovation 2015 July
Sources of Potentially Avoidable Emergency Department Visits. Canadian Institute for Health Information 2014
Kellermann, Arthur L. and Robin M. Weinick. Emergency Departments, Medicaid Costs, and Access to Primary Care – Understanding the Link. NEJM 2012;366:2141-2143
Raven, Maria C. and Robert A. Lowe, Judith Maselli, Renee Y. Hsia. Comparison of Presenting Complaint vs. Discharge Diagnosis for Identifying ”Nonemergency” Emergency Department Visits. JAMA 2013;309(11):1145-1153
Hannam, Paul. Health Equity, Trust and Data Collection in the Emergency Department. Emergency Medicine Cases 2015 Aug
Rose, Katherine and Joseph S. Ross, Lenora I. Horwitz. Advanced access scheduling outcomes: A systematic review. Arch Intern Med 2011 July;171(13):1150-1159
Advanced Access and Efficiency Workbook for Primary Care. Health Quality Ontario (July 2011)
Plsek, Paul. Little Hope: How Common Sense Thinking Can Lead To a Mess. Institute for Healthcare Improvement National Forum 2000
Zimmerman, Brenda and Glouberman, Sholom. Complicated and Complex Systems: What Would Successful Reform of Medicare Look Like? Commission on the Future of Health Care in Canada 2002; Discussion Paper 8
Helbing, Dirk. Globally Networked Risks and How to Respond. Nature 2013;497:51-59





Another interesting article. I am not sure if this analysis truly applies to all EDs however. You make mention of the small, rural ED. I work in one of those and our daily visits are highly weighted toward chronic, elderly pts (your Cohort C), often with acute exacerbations (COPD, CHF, “weak and dizzy”) and then the CTAS 4 and 5 “can’t get in to see my Family doc” pts, many of whom quite frankly would not have come to an ED (or even their GPs) twenty or so yrs ago and would mostly have fared just fine. We have been told that the fixed cost of one pt registering for the ED is in the neighbourhood of $300…not insignificant at all if you add it (if it is in fact correct). This is just admin costs and does not include the salary of the NP or the hourly wage of the physician. Our ED is a one physician ED and we have one NP (only for the last year or so) so the CTAS 4/5’s can back up quite quickly if we get a couple of higher acuity patients, creating disgruntlement among the lower acuity pts who don’t understand (or don’t want to understand) the concept of triage based on acuity. The province sets goals for wait time reduction for those patient as well as the higher acuity patients of course and yet, as I have said above many of these people could actually wait a day or so to see someone else or even get by without seeing a physician. I believe part of our problem in North America is that our culture has become one where having a medical professional solve every health issue, no matter how minor, has become expected. This leads to people seeking more medical care for things many people would have dealt with on their own not so long ago, as I have stated above. I have friends in Europe who would never consider bringing themselves or their children to an ED for many of the things we see here or even to their doctor. Perhaps the burden of these visits is not as great relatively at larger urban hospitals but my opinion, based on some experience at different rural hospitals, is that it represents a large proportion of workload at these smaller hospitals. Of course, there is a perverse incentive to keep these people coming to the rural EDs in Ontario if they are funded by an hourly AFA because we are given money based on total OHIP billable visits, therefore the greater the number of visits, the greater the funding and the more we can pay our physicians, many of whom come from other areas and are at least partly motivated by hourly rates. One of our greatest challenges in attracting physicians is how much we pay compared to how much the other hospitals pay, who often have higher volumes and therefore higher hourly wages.
Bit of a long diatribe but I would be interested to know if you have any idea of how ED systems work in places like Europe or perhaps Australia/New Zealand and how their utilization compares with that in North America and how cultural differences might play into the equation. I know in the UK there have been active efforts on the part of the government to educate the public on appropriate uses of A&E, as they call it. I can’t help but think that might be useful here. It might reduce some of the utilization issues and allow us more time to take care of the more acute cases as well as those elderly, frail, chronic patients who we are only going to see more of as the baby boomers (myself included) continue to age a “rust out”.
Thanks for the comment Bruce. Emergency Medicine is very community and culturally sensitive, but overall ED visits are growing internationally and cultural expectations are moving toward expectations of access to sophisticated diagnostics and consultations for assessment and treatment of acute illness and injury. With internet and smart phones and WebMD that trend will be hard to buck. But there is still an opportunity, especially in smaller communities, to ensure alternatives to the ED are well known, well organized and accessible. And to educate patients on where to go when for help. That is hard to do at a system level.
With respect to costs, much of the fixed costs are not recoverable by a few less patients not registering. Most of the ED costs are labour, and you can only reduce by a full person, not a portion. Therefore iff there is a volume decrease of a significant and sustained amount, you can reduce staffing by 1 FTE. So true marginal costs of each additional person are far less than $300, although a program that decreases volumes by a significant amount can recover “real money” as 1 FTE/24 hours will be several hundred thousand dollars/year.
The challenges of aligning physician payments with other incentives and recruitment to low volume practice locations are for another day!
Howard Ovens
In addition to human staff being indivisible, Emergency Departments are indivisible; if a community makes a certain threshold (however defined; population, historical pt volumes, distance from regional centre, etc) that “requires” an ED be there, then, these come in units of one ED (not .68 of an ED, say).
So if the #s justify .68 of an ED/EP and 1 is there, then there might be some “extra” capacity to see pts from column 2 (potentially schedulable) in that 2×2 table. Yes, with short term surges of pts in column 1, these patients may have to wait a little longer but wrt system costs it might be more cost effective to see these patients in the ED (rather than opening up a walk-in across the street). Obviously, the better answer would be to have same day/next day access to primary care / continuity of care if that is possible in any given community.
Re other systems in Europe – I do believe that pts can be referred from ED triage (or even better, book their own appointments on line) if they fall into that second column, directly to primary care clinics integrated with their own primary care “collaborative practice”. Certainly the UK does this, and in Norway.
David I hate the “triage away” concept; least patient-centred thing I can imagine. You have to assess the patient BEFORE you “triage” them away, why not just complete the process – educate the patient, and arrange f/u for another day????
I agree, I hate the triage “away” concept as well… I am thinking more of a triage “into” another stream that is still geo-located within spitting distance from the main ED (or may even just be a virtual space embedded within the same ED). So, if you have large enough volumes (and good enough triage distinguishers between the patient types) then creating a fast track (for quadrant B), a RAZ (for quadrant A, ambulatory 3s), a resusc/monitored bed zone (for quadrant A,1,2, and non-ambulatory 3s) and another zone, or stream, for quadrant C and quadrant D pts. This C/D zone could be managed by NPs with EP (or GP) oversight? Some degree of smoothing could occur between zones depending on the day, and obviously given the uncertainty and undifferentiated nature of many presenting complaints significant vigilance would have to be maintained to avoid the “geography is destiny” cognitive errors.
The “educate the patient, and arrange f/u for another day” part of this is absolutely key to changing the trajectory of care (and costs) for this patient over the next months to years, and EPs don’t do a great job with this if they are feeling overwhelmed by a lack of surge capacity (or are trouble shooting daily flow/boarding issues). My sense is that when the C/D patients get embedded in the other streams, and are “seen” by EPs in a rush, we do a poor job in meeting the patients and the system’s needs. Perhaps this issue is addressed well by discharge planning RNs and GEMs, etc, in some depts., but there may be an opportunity to do it better in some regions of the Country?
We can always do it better! That’s why we have this blog :)