Dr. Clare Atzema, Dr. Nazanin Meshkat and Dr. Bryan Au discuss the presentation, etiology, precipitants, management and disposition of Atrial Fibrillation in the Emergency Department. The pros and cons of rate vs rhythm control are debated, what you need to know about Afib medications, and the value of the Ottawa Aggressive Protocol discussed. The importance of appropriate anticoagulation is detailed, with a review of the CHADS-VASc score and whether to use anticoagulants or ASA for stroke prevention for patients with Atrial Fibrillation. We end off with a discussion on how to recognize and treat Wolff-Parkinson-White syndrome in the setting of Atrial Fibrillation.
Drs. Meshkat, Atzema and Au answer such questions as: What factors should you take into account when deciding whether to use rate control or rhythm control? How is Aflutter treated differently to Atrial Fibrillation in the ED? What are the indications for admission for Atrial Fibrillation and who can be safely sent home? How does the CHADS-VASc score compare to the CHADS2 score for determining who needs anticoagulation for stroke prevention? In which patients is electrical cardioversion contra-indicated? How can we recognize and manage the deadly WPW in the setting of rapid Atrial fibrillation? Why should you consider using an initial energy level of 200J biphasic for all your patients with Afib of Aflutter for electrical cardioversion despite the ACLS guidelines suggesting lower levels? and many many more……
Written Summary and blog post by Claire Heslop, edited by Anton Helman February 2012
Cite this podcast as: Atzema, C, Meshkat, N, Au, B, Helman, A. Atrial Fibrillation. Emergency Medicine Cases. February, 2012. https://emergencymedicinecases.com/episode-20-atrial-fibrillation/. Accessed [date].
ATRIAL FIBRILLATION
The most common dysrrhythmia seen in ED, and incidence increasing with ageing population
Presentation
Common presentations: younger patients often feel palpitations and non-anginal chest discomfort, vs. older patients often present with vague symptoms such as fatigue, lightheadedness and dyspnea
Uncommon presentations: TIA, CHF or ACS
A.fib rarely causes syncope in itself – look for another cause: cardiomyopathy, Brugada syndrome, PE, WPW or vasovagal syncope
A.fib is rarely the sole cause of a patient’s hemodynamic instability, so look for another cause – sepsis, hemorrhagic (GI, AAA), dehydration, etc
Etiology or Precipitants of Atrial Fibrillation
PIRATES – PE, Ischemia, Respiratory disease, Atrial enlargement or myxoma, Thyroid disease (check TSH and free T4 in first-time presenters), Ethanol (“Holiday heart” after binging), Sepsis or Sleep apnea
Others include myocarditis and chronic hypertension
Etiology of Slow A.fib: AV nodal blocking agents (digoxin, beta-blocker or calcium-channel blocker toxicity or at too high doses), sick sinus syndrome and severe hyperkalemia
1/3 are ‘lone Afib’ with no demonstrable cause
In most cases, when the underlying cause is addressed the A.fib resolves
ECG Findings in Atrial Fibrillation
Irregularly irregular narrow-complex tachycardia can be A.fib, A.flutter with irregular conduction, or multifocal atrial tachycardia (MAT) – rate of 100-150/min with 3 different P wave morphologies, variable PR length and poor response to typical medications; find and treat the underlying cause (often COPD)
ST Depressions: common and often due to rate-related ischemia in atheroscletoric coronaries of older patients; should not be investigated further UNLESS patient has anginal chest pain or ACS is likely, or ST segments do not resolve once the patient is not in fast A.fib anymore (after rate control or cardioversion)
Rate Control vs. Rhythm Control in Atrial Fibrillation
AFFIRM trial showed no benefit in rhythm control vs. rate control in terms of morbidity and quality of life, but patients deemed not likely to tolerate being in A.fib were excluded from the study (thereby negating any possible benefit shown in these patients)
The goal for rate control is HR of <110 bpm
Update 2014: Risk of stroke and death in paroxysmal vs persistent Afib full pdf
Update 2014: Time to Cardioversion for Acute Atrial Fibrillation and Thromboembolic Complications paper from JAMA showing that significant stroke risk may occur with cardioversion as early as 12hrs after symptoms start Abstract
Update 2020: A randomized blinded study involving 2789 patients in 135 European hospitals demonstrated that rhythm control is associated with a lower risk of adverse cardiovascular outcomes in patients with early atrial fibrillation (<1 year) and co-morbid cardiovascular conditions Abstract
Link to The Stiell Sessions Part 2: Update in Atrial Fibrillation – The New Guidelines 2014
Medications for Rate Control in Atrial Fibrillation
Beta-blocker (works in 70% of patients): metoprolol 5mg IV q20min up to 15mg, followed by 25-50mg PO – consider using if patient has HTN, CAD, diabetes, prior MI or hyperthyroidism, but do NOT use in asthmatics or patients in acute heart failure
Calcium-channel blocker (works in 54% of patients): diltiazem 10-20mg IV, followed by PO
Update 2018: After an initial IV loading dose of diltiazem in patients with afib with rapid ventricular response (RVR), a single-centre retrospective review of 111 patients showed an associated lower failure rate at 4 hours using PO diltiazem, compared to IV diltiazem infusion. Given these findings, the route of post-loading dose administration can influence disposition for those with afib and RVR. Abstract
Digoxin: should NOT be used as ineffective for rate control, takes a long time to act, and is poor at controlling rate in exercise or anxiety (works through vagal stimulation), therefore does not prevent tachycardia- mediated cardiomyopathy
Amiodarone: consider using in A.fib patient with acute heart failure, esp. If BP is tenuous
In all cases, maximize first agent and avoid going to second agent – re-visit the diagnosis or consider consulting a consultant for admission in these cases
Update 2018: Magnesium Sulfate – A double-blind, randomized controlled trial (The LOMAGHI study) demonstrated IV MgSO4 dosed at either 4.5g or 9g, when combined with other AV nodal blockers, had a synergistic effect on improving rate control of rapid atrial fibrillation in the emergency department. Of note, the 9mg dose had more side effects, and most patients were on digoxin as opposed to other rate control agents (e.g. beta-blockers, calcium channel blockers). Abstract
Cardioversion for Atrial Fibrillation
40-70% of patients will spontaneously convert back to NSR at 24hrs, with shorter episodes more likely to predict conversion (66% if A.fib 24hrs); also less likely to convert if due to underlying cause or enlarged atrium (more likely permanent A.fib)
After discussion with patient, may elect to return next day for assessment; but most patients who present to ED want something done to improve their condition
Patients may be educated to wait 6-8hrs at home the next time they have an episode, EXCEPT if worrisome symptoms are present (chest pain, dyspnea, lighthheadedness)
Update 2019: In a prospective, randomized non-inferiority trial of 427 hemodynamically stable patients with recent onset of atrial fibrillation (<36hours), a wait-and-see approach was non-inferior to early cardioversion with respect to achieving a return to sinus rhythm at 4 weeks. Abstract
Chemical Cardioversion for Atrial Fibrillation
Successful in 60% of cases, but carries higher risk of arrhythmias and hypotension, and longer length of stay in ED
CLASS I medications: flecainide (2mg/kg IV over 10min – most effective), ibutelide (1mg over 10min, repeat at 20min PRN; monitor QT prolongation and consider pre-treatment with MgSO4), and propafenone (“pill in pocket” used by patients when they feel onset of palpitations – must be used in conjunction with beta-blocker to prevent fast dysrhythmias)
Next line agents: procainamide (used in Aggressive Ottawa Protocol by Stiell et al.: 18-20mg/kg at 20- 30mg/min and stop if convert to NSR, QT increase to 2 times duration, or hypotension), and amiodarone in cases of structural heart disease (monitor for bradycardia and hypotension; not very effective but consider using in pulmonary edema)
Electrical Cardioversion of Atrial Fibrillation
More effective than chemical cardioversion (90%), but patient may prefer not to use given fear or pain Do NOT attempt in patients at high risk of thrombo-embolic events (valvular heart disease, severe mitral
disease, cariomyopathy, prosthetic valve or prior TIA/CVA), or when procedural sedation is contra-indicated
Consider using initial energy level of 150-200J biphasic to increase the success rate and decrease the number of total shocks given
Update 2015: Study suggests that patients with atrial fibrillation or flutter with an acute underlying medical illness may not benefit from rate or rhythm control. Article
Anticoagulation for Atrial Fibrillation
Risk of stroke is EQUAL for paroxysmal and persistent A.fib, so even if patient is in NSR at discharge from ED, he or she STILL needs anticoagulation based on risk stratification at least until follow up
Risk of CVA for non-valvular A.fib is 5% per year (1-2% if <60yo, but 25% if >80yo), and risk reduced to 1% with anticoagulation (risk reduction 70% with NNT 25); risk of CVA with cardioversion is dependent on risk factors and length of A.fib but ranges in 1-5%
Use heparin (UFH or LMWH) if patient has arrhythmia of >48hrs or unknown duration and hemodynamically unstable needing emergent cardioversion, or if
Canadian Cardiovascular Society recommends using CHADS2 score to predict risk of CVA
CHF, HTN, Age≥75, Diabetes, TIA/CVA (2 points) – score ≥1 = dabigatran or warfarin; consider ASA if score of 1 and patient reluctant to anticoagulate, but urge follow up with GP or cardiologist; also consider ASA if score is 0 and patient is not young
European guidelines recommend using CHA2DS2VASc score given that CHADS2 does not include other (but still important) risk factors
CHF, HTN, Age ≥75 (2 points), Diabetes, TIA/CVA (2 points), Vascular diseases (CAD, MI, PVD), Age 65-74, Sex category (female 1 point, male 0 point)
No anticoagulation in younger patients with presumably no structural heart disease and CHA2DS2VASc = 0
Warfarin
- NNT to prevent 1 stroke = 25; NNH to cause 1 intracerebral bleed = 400
- HAS BLED mnemonic for bleeding risk: HTN, Abnormal renal or liver function, Stroke, Bleeding history, Labile INR, Elderly ≥65yo, Drugs that promote bleeding or excess alcohol use – Score ≥3 means higher (3.7%) risk of major bleeding
Dabigatran
- Oral direct thrombin inhibitor with peak effect in 2hrs and no monitoring needed; however, can’t check compliance, there is no reversal in major bleeding (attempt dialysis instead), and contraindicated in renal failure; it is also expensive and not covered
- As effective as warfarin with slightly lower ICH but slightly higher GI bleeds, and may be associated with increased MI
- Dosage: at 110mg PO od, equivalent than warfarin in preventing stroke with significantly lower bleeds; at 150mg PO od, superior than warfarin at preventing stroke with equivalent bleeds
- Consider using it in patients with difficult to manage INR
Update 2015: Study in Annals of Emergency Medicine suggests that patients given a prescription for warfarin in the ED may have better rates of long-term anticoagulation. Abstract
Disposition for Atrial Fibrillation
Most patients can be discharged home – prescribe medications to rate control if this strategy was chosen, ensure follow up (with TSH testing if not done in ED), and consider follow up with cardiologist to perform Holter, echocardiography or ablation, as well as in first-time presenters or patients with associated CAD or CHF
Indications for Admission: A.fib in association with hyperthyroidism, ischemia, pneumonia or CHF (increased mortality), rate difficult to control
Update 2015: A 30-day mortality clinical decision instrument for patients who present to the ED with AFib Abstract
Update 2018: A retrospective review showed nuisance bleeding in atrial fibrillation patients on anti-coagulation (i.e. bleeding not requiring medical attention) is common, and was not associated with increased risk of stroke/systemic embolism or major bleeding. Abstract
Is a Troponin necessary for all acute Atrial Fibrillation patients in the ED?
In an unpublished review of charts at the University Health Network, 86% of patients had troponins drawn, 14% were positive and 5% of patients were treated as ACS – most of these had hypotension, signs of heart failure, or ECG changes after conversion or rate control
Ischemia may be the result or the cause of A.fib, so consider doing troponins when there are clinical features of ACS present or risk factors for CAD
Atrial Flutter
Look in leads II, III, aVF to see saw-tooth waves (or turn ECG upside down to see them better), especially if the narrow-complex tachycardia is around 150/min
Pharmacological cardioversion and rate control are both MUCH less effective than with A.fib Unclear if it really takes less energy to cardiovert (50J), so consider using 150-200J initially
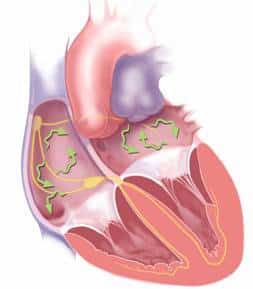
Wolff-Parkinson-White Syndrome (WPW)
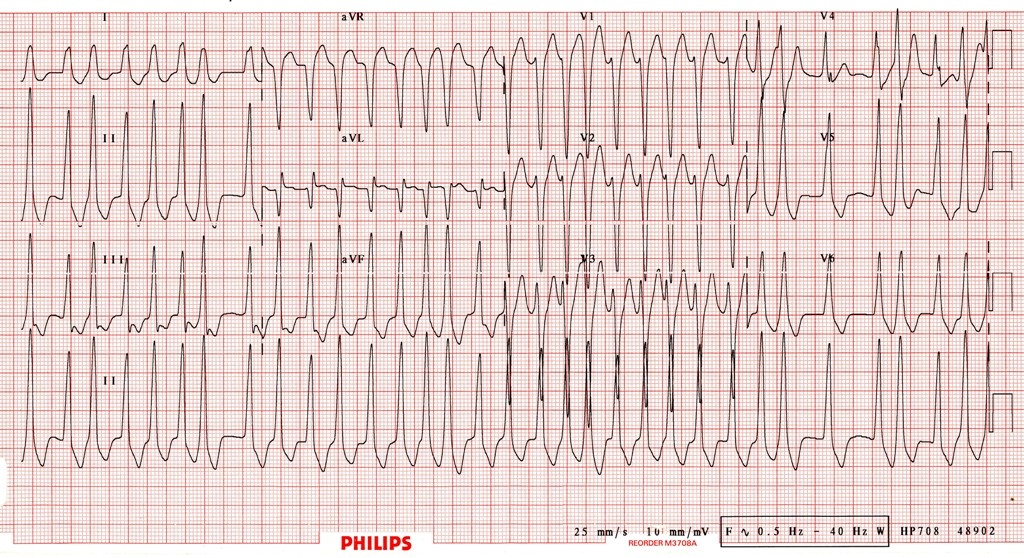
Differential of A.fib with wide QRS: A.fib with aberrancy (RBBB or LBBB – QRS usually has typical morphology), or A.fib with pre-excitation – eg, WPW: esp. when QRS morphology is bizarre, polymorphic and much faster than usual A.fib (sometimes approaching 300)
NEVER give AV nodal blocking agent (beta-blocker, calcium-channel blocker, adenosine, digoxin and even amiodarone) as the AV node will be blocked and impulses sent preferentially down the bypass tract – which doesn’t have any slowing mechanism – and trigger VF
Treatment: electrical cardioversion, or procainamide is the safest medication
ECG of A.fib with WPW:
Link to The Stiell Sessions Part 2: Update in Atrial Fibrillation – The New Guidelines 2014
For more on atrial fibrillation on EM cases:
Episode 57: The Stiell Sessions 2 – Update in Atrial Fibrillation 2014
Best Case Ever 7: Atrial Fibrillation
Dr. Meshkat, Dr. Au and Dr. Atzema have no conflicts of interest to declare.
Key References
Wyse DG, Waldo AL, Dimarco JP, et al. A comparison of rate control and rhythm control in patients with atrial fibrillation. N Engl J Med. 2002;347(23):1825-33.
Camm AJ, Lip GY, De caterina R, et al. 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation–developed with the special contribution of the European Heart Rhythm Association. Europace. 2012;14(10):1385-413.
Pisters R, Lane DA, Nieuwlaat R, et al. A Novel User-Friendly Score (Has-Bled) To Assess 1-Year Risk Of Major Bleeding In Patients With Atrial Fibrillation: The Euro Heart Survey. Chest. 2010;138(5):1093-1100.
Cairns JA, Connolly S, Mcmurtry S, Stephenson M, Talajic M. Canadian Cardiovascular Society atrial fibrillation guidelines 2010: prevention of stroke and systemic thromboembolism in atrial fibrillation and flutter. Can J Cardiol. 2011;27(1):74-90.
Stiell IG, Clement CM, Perry JJ, et al. Association of the Ottawa Aggressive Protocol with rapid discharge of emergency department patients with recent-onset atrial fibrillation or flutter. CJEM. 2010;12(3):181-91.
Now test your knowledge with a quiz.




[…] Episode 20: Atrial Fibrillation, Best Case Ever 7: Atrial Fibrillation, and Episode 57: The Stiell Sessions 2 – Update in Atrial Fibrillation 2014 on Emergency Medicine Cases […]