Kids aren’t little adults. Pediatric sepsis and septic shock usually presents as ‘cold shock’ where as adult septic shock usually presents as ‘warm shock’, for example. In this episode, a continuation of our discussion on Fever from with Ottawa PEM experts, Sarah Reid and Gina Neto, we discuss the pearls and pitfalls in the recognition and management of pediatric sepsis and septic shock. We review the subtle clinical findings that will help you pick up septic shock before it’s too late as well as key maneuvers and algorithms to stabilize these patients. We cover tips for using IO in children, induction agents of choice, timing of intubation, ionotropes of choice, the indications for steroids in septic shock, and much more…..
Written Summary & Blog post Prepared by Michael Kilian & Niran Argintaru, edited by Anton Helman, August 2014
Cite this podcast as: Helman, A, Reid, S, Neto, G. Recognition and Management of Pediatric Sepsis and Septic Shock. Emergency Medicine Cases. August, 2014. https://emergencymedicinecases.com/episode-50-recognition-management-pediatric-sepsis-septic-shock/. Accessed [date].
Pediatric Sepsis
Sepsis in children is a relatively rare emergency department presentation. Although only about 0.35% of pediatric emergency department visits are for sepsis, the mortality rate is as high as 2 to 10% (1,2). Having a sepsis guidelines protocol in the emergency department can decrease mortality from 5% to as low as 1% (2)
Red Flags in the Recognition of Pediatric Sepsis
- Age:
- Of the children <1yr, most will be
- Unexplained tachycardia (after correcting for fever – see below)
- Clinical signs:
- Poor perfusion (long cap refill, lethargy, irritability)
- Conditions that predispose to sepsis: neuromuscular disease, immunocompromised, respiratory conditions, cardiac disease
- Recent surgery
Temperature Corrected Heart Rate and Respiratory Rate
**Recall from podcast 48, rule of thumb – Heart Rate increases by approximately 10 beats/min and Respiratory Rate by 5 breaths/min for every Celsius degree (1.8 degree of Fahrenheit) of fever >38°C
Normal Pediatric Vital Signs
| Age | Heart Rate (beats/min) | Blood Pressure (mm Hg) | Respiratory Rate (breaths/min) |
| Premie | 120-170 | 55-75/35-45 | 40-70 |
| 0-3 mo | 100-150 | 65-85/45-55 | 35-55 |
| 3-6 mo | 90-120 | 70-90/50-65 | 30-45 |
| 6-12 mo | 80-120 | 80-100/55-65 | 25-40 |
| 1-3 yr | 70-110 | 90-105/55-70 | 20-30 |
| 3-6 yr | 65-110 | 95-110/60-75 | 20-25 |
| 6-12 yr | 60-95 | 100-120/60/75 | 14/22 |
| 12 > yr | 55-85 | 110-135/65/85 | 12-18 |
Hypotension is a Late Sign of Pediatric Septic Shock
- Be very cautious in setting of tachycardia and DO NOT WAIT for hypotension to make diagnosis of septic shock.
- A pediatric patient with hypotension and sepsis is a pre-arrest patient.
Investigations in Sepsis
Blood work should include CBC, electrolytes, glucose, kidney function, blood gas, blood cultures, LFTs, and lactate. Urine cultures are commonly done to identify a possible source. Clinical history guides imaging such as chest x-ray.
ABC – DEFG = ABC, DON’T EVER FORGET GLUCOSE
Up to 25% of children with septic shock will have adrenal insufficiency, so always check glucose in septic children. Extremes in blood glucose in sepsis are associated with higher mortality in children (2). Arterial lactate 2 times upper limit of normal indicates organ dysfunction.
Acute Management of Pediatric Sepsis
Fluid Resuscitation in Pediatric Sever Sepsis and Septic Shock
Circulation is of paramount importance in this patient and COMES BEFORE AIRWAY and all other concerns. Thus the approach should be CAB:
1) Circulation, 2) Airway, 3) Breathing.
Establishing IV access in a septic child can be very difficult, especially in the setting of hypotension. If, after 1MINUITE of trying, you cannot establish IV access, move to IO (ideally x2).
Initial fluid goal: 60cc/kg of NS in first hour (3)(2)
- Older children: level 1 infuser
Blood pressure should not be a deciding factor in giving fluids. All septic patients should receive the initial boluses.
Update 2022: A retrospective study from the Improving Pediatric Sepsis Outcomes (IPSO) multicenter quality improvement collaborative including 1204 children with hypotensive septic shock found that there was no 30 day mortality benefit for those who received >30mL/kg fluid resuscitation compared to those who received <30mL/kg within the first hour of ED arrival. Abstract.
Intraosseous Access (IO)
IO access can be used in all ages, even in awake patients. Studies show that the pain from the IO comes more from the actual infusion than the insertion (5). In order to decrease pain, consider infiltrating lidocaine into the bone prior to infusion of fluids. The possibility of pain should not cause hesitation in establishing IO access. (2)
Sites (in this order of preference):
- Proximal tibia
- Distal femur
- Proximal humerus
You can administer the same agents through an IO as an IV (fluids, antibiotics, vasopressors etc.)(2)
Initial Antibiotic Choice: Ceftriaxone 100mg/kg IV push(2)
When to intubate in Pediatric Sepsis and Septic Shock?
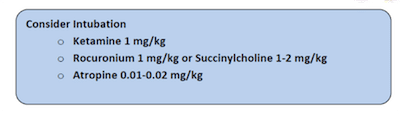
Consider early intubation in fluid refractory septic shock (after 3 boluses of 20ml/kg IV NS) or in any compromised airway.
Infants or neonates with severe sepsis may require early intubation. Intubation and mechanical ventilation increases intrathoracic pressure which reduce venous return and lead to worsening shock. Therefore, fluid resuscitation must be done first.
Choice of medications in intubation
There is no strong data supporting any particular induction agents or paralytic agents in the intubation of a septic child.
| Ketamine | Drug of choice as it is relatively safe in hypotension and tachycardia. However, catecholamine depletion can cause refractory hypotension and result in worsening shock. |
| Propofol | Should not be used for long-term sedation in children younger than 3 years old because of an association with fatal metabolic acidosis. |
| Etomidate | Should be discouraged or used carefully in septic shock as it inhibits the adrenal axis and sympathetic nervous system affecting hemodynamic stability. Etomidate is associated with increased mortality in children with meningococcal sepsis because of adrenal suppression effect. |
Succinylcholine 1 mg/kg (or 2mg/kg in infants) IV or Rocuronium 0.45-0.6 mg/kg IV are both reasonable choices for paralytic agents.
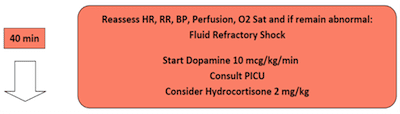
Fluid Refractory Shock
If there are no signs of improvement within 1 hour of aggressive fluid resuscitation (remember goal of 60cc/kg), the initiation of ionotropes is indicated. Consider which agent you will use early (during second bolus of 20cc/kg) so that it can be ready to administer at 60min mark without delay if necessary. (2)
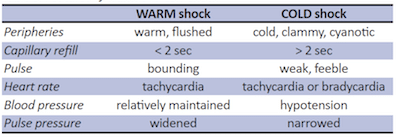
Cold vs. Warm shock
Most children have COLD shock, which is characterized by high SVR and low cardiac output (this differs from adults who usually have low SVR and present with warm shock). Thus, children are poorly perfused, have delayed cap refill with cold extremities and have a temperature differential between their core and their extremities. (5)
Ionotropic Choices in Pediatric Septic Shock
- Cold Shock: Epinephrine 0.05-0.3 mcg/kg/min and titrate to effect
- Warm Shock: Norepinephrine .05-0.3 mcg/kg/min and titrate to effect.
You can safely start these inonotropes through a peripheral IV or IO. The lack of a central line should not delay the initiation of inonotropes at the 60min mark. (2)(5)
Adjunct Treatments in the Management of Pediatric Sepsis and Septic Shock
- Glucose: Remember to check the glucose in all children and treat as necessary. Both hypo and hyperglycemia are associated with worse outcomes. For glucose <6mmol, start D10W 5cc/kg (avoid higher concentration). (2)
- Corticosteroids: The use of hydrocortisone in pediatric septic shock is currently being investigated and its role is unclear. Consider using hydrocortisone 2mg/kg in any child that has fluid and inotropic resistant septic shock or proven adrenal insufficiency (1).
Goals of Resuscitation in Pediatric Septic Shock
Normalization of vital signs is a main goal. Aim for a normal blood pressure, pulse (without differences between central and peripheral pulses).
Clinically, the child should have a normal capillary refill, warm extremities and urine output >1ml/kg/hour indicating improved perfusion. Lactate and mental status should be normalized as well.
Cognitive Decision Aids in The Management of Pediatric Sepsis and Septic Shock
ESTABLISHED PROTOCOLS for pediatric sepsis have been shown to DECREASE MORTALITY. (5)(2) It is helpful to have your room equipped with PALS algorithms (6), broslow tapes, GCS and normal vital sign tables to facilitate timely and accurate decisions. See below for The Children’s Hospital of Eastern Ontario pediatric sepsis algorithm.
Extra-Corporeal Membrane Oxygenation (ECMO)
If all else fails, ECMO can be used in the child who is in cardio-respiratory failure and refractory to all treatment. (2) However, in Canada, this treatment is almost exclusive to the ICU setting given all the resources involved.
Children’s Hospital of Eastern Ontario Algorithm for Septic Shock
Key Take Home Points
- Hypotension is a late sign – do not wait for it to diagnose and aggressively treat pediatric sepsis.
- CAB, not ABCs – fluid 20ml/kg is the first priority even if normal BP. Aim for three boluses over the first hour. Don’t delay using an IO!
- Early goal directed therapy – early antibiotics! (ceftriaxone
20100mg/kg IV) - Don’t forget glucose –a large proportion of septic children have adrenal insufficiency, which is associated with increased mortality.
Now Test Your Knowledge
For more Pediatric EM learning visit one of EM Cases newest collaborators trekk.ca – Translating Emergency Knowledge for Kids (TREKK) is a growing network of researchers, clinicians, health consumers and national organizations who want to accelerate the speed at which the latest knowledge in children’s emergency care is put into practice in general EDs – rural, remote or urban.
 For more information on paediatric shock on EM Cases:
For more information on paediatric shock on EM Cases:
Best Case Ever 27: Pediatric Shock
For more EM Cases content on Paediatric Emergencies visit EM Cases Digest Vol. 2 Pediatric Emergencies here.
Dr. Helman, Dr. Neto and Dr. Reid have no conflicts of interest to declare.
Key References
1) Singhal S, Allen MW, Mcannally JR, Smith KS, Donnelly JP, Wang HE. National estimates of emergency department visits for pediatric severe sepsis in the United States. PeerJ. 2013;1:e79. Full Text
2) Dellinger RP, Levy MM, Rhodes A, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. 2013;41(2):580-637. Full text
3) Kleinman ME, Chameides L, Schexnayder SM, et al. Pediatric advanced life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Pediatrics. 2010;126(5):e1361-99. Full Text
Now test your knowledge with a quiz.







In the Key Take Home Points, I think it should be ceftriaxone 100 mg/kg (not 20 mg/kg).
Thanks for the correction Thomas!