We rarely discuss medico-legal issues on EM Cases because it misguides us a bit from good patient centered care – which is what emergency medicine is really all about.
Nonetheless, missed orthopedic injuries are the most common reason for an emergency doc to be sued in Canada. This is partly because missed orthopedic injuries are far more common than missed MIs for example, but it’s also because it’s easy to miss certain orthopedic injuries – especially the ones that aren’t super common. And orthopedics is difficult to learn and remember for the EM practitioner as there are so many injuries to remember.
And so, you guessed it – on this episode we’re going to run through some key not-so-common, easy to miss orthopedic injuries, some of which I, personally had to learn about the hard way, if you know what I mean.
After listening to this episode, try some cognitive forcing strategies – for every patient with a FOOSH that you see, look for and document a DRUJ injury. Wait, hold on….I don’t wanna give it all away at the top of the post.
Let’s hear what EM doc and sports medicine guru Ivy Cheng, and the orthopedic surgeon who everyone at North York General turns to when they need help with a difficult ortho case, Hossein Medhian, have to say about Commonly Missed Uncommon Orthopedic Injuries.
Written Summary & Blogpost written and prepared by Keerat Grewal and Anton Helman, Oct 2014
Cite this podcast as: Cheng, I, Medhian, H, Helman, A. Commonly Missed Uncommon Orthopedic Injuries. Emergency Medicine Cases. October, 2014. https://emergencymedicinecases.com/episode-52-commonly-missed-uncommon-orthopedic-injuries/. Accessed [date].
Quick Reference Cards for each injury discussed in this episode (click on card to view pdf)
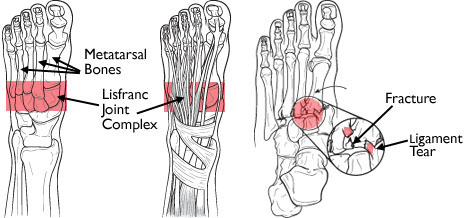
Lisfranc Injuries – Commonly Missed Uncommon Orthopedic Injuries
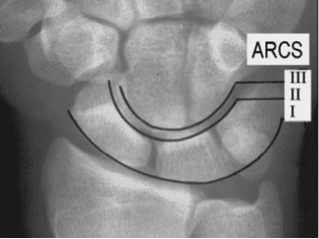
Perilunate Injuries –
Commonly Missed Uncommon Orthopedic Injuries
Distal Radius Ulnar Joint (DRUJ) Injuries
Pelvic Apophyseal Avulsion Fractures
For more on missed orthopedic injuries on EM Cases:
Episode 1 Occult Fractures and Dislocations
Episode 58 Tendon and Ligament Commonly Missed Uncommon Orthopedic Injuries
For more on Orthopedic Pearls & Pitfalls download our free interactice eBook EM Cases Digest Vol.1 MSK & Trauma
Dr. Helman, Dr. Mehdian and Dr. Cheng and no conflicts of interest to declare.
Key References
- Anderson, RB, Hunt, KJ, & McCormick, JJ. Management of common sports-related injuries about the foot and ankle. 2010. J Am Acad Orthop Surg, 18(9): 546-56. Abstract
- Caswell, F & Brown C. Identifying foot fractures and dislocations. 2014. Emerg Nurse, 22(6): 30-4. Abstract
- Stanbury, SJ & Elfar, JC. Perilunate dislocation and perilunate fracture-dislocation. 2011. J Am Acad Orthop Surj, 19(9): 554-562. Abstract
- Boyd, KT, Peirce, NS, & Batt, ME. Common hip injuries in sport. 1997. Sports Med, 24(4): 273-88. Abstract
- Moeller, JL. Pelvic and hip apophyseal avulsion injuries in young athletes. 2003. Curr Sports Med Rep, 2(2): 110-5. Abstract
Now test your knowledge with a quiz.



















i am so ever grateful to you for the great work
This MSK episode was just great. Precisely the kind of info on these zebras that we need to bring them into our awareness and great detail on mechanisms and management. It certainty elevated my understanding of Lisfranc, as it had been my impression that this was a rare injury, requiring a considerable force, usually occurring when a driver hits something hard with the foot jammed on the brakes.
Lisfranc, as I am sure everyone knows, was Napoleon’s physician, and the metatarsal/tarsal joint was where he performed his eponymous front foot amputations (with an axe) on those soldiers unfortunate enough to have stepped on a piece of exploding ordinance.
Great work guys. We in ER practice are indebted to the entire team.
[…] EM Cases: Missed Ortho Injuries […]
Thank You for the the informative evuidence-based practice knowledge ,It adds a real life case presentation and hone the experience