In this second part of the Weingart-Himmel Sessions on critical care pearls for the community ED on the EM Cases podcast, Dr. Scott Weingart and Dr. Walter Himmel discuss the many controversies and recent changes in fluid management in severe sepsis and septic shock. With the recently published ARISE trial, and some deviations from Early Goal Directed Therapy, we are changing the way we think about fluids in sepsis: the type of fluid, the volume of fluid, the rate of fluid administration, the timing of introducing vasopressors and the goals of fluid resuscitation. In the next section of the podcast we discuss the PAD mnemonic for post-intubation analgesia and sedation, the prevention of delirium, and medication choices to minimize time on the ventilator, and improve prognosis.
Written Summary & blog post prepared by Dr. Anton Helman, December 2014
Cite this podcast as: Helman, A, Weingart, S, Himmel, W. Fluids in Sepsis, Post-intubation Analgesia and Sedation. Emergency Medicine Cases. December, 2014. https://emergencymedicinecases.com/episode-55-weingart-himmel-sessions-2-fluids-in-sepsis-post-intubation-analgesia-sedation/. Accessed [date].
Fluid of Choice in Severe Sepsis & Septic Shock
Choices for initial fluid management in the ED for severe sepsis and septic shock are Normal Saline, Ringer’s Lactate or Plasmalite. Practically speaking, Normal Saline is what North American EDs are most familiar with and is recommended for the first 3-4L of fluid resuscitation despite concerns of hyperchloremic acidosis with larger volumes. If more than 3-4L of fluid is required, some experts suggest switching to Ringer’s Lactate or Plasmalite to minimize the risk of acidosis.
How do colloids such as albumin compare to crystalloids for fluid resuscitation in hypovolemic shock?
The CRISTAL trial comparing albumin and crystalloids showed no difference in 28 day mortality.
Update 2021: Retrospective, cohort review of 109 patients admitted for operative management of newly diagnosed ectopic pregnancy. Use of point-of-care ultrasound (POCUS) showed shorter length of stay in ER and faster time to OR for ruptured ectopic when compared to radiology-based ultrasound alone. Abstract
How Much Fluid, How Fast for Severe Sepsis & Septic Shock
Based on the recent PROCESS and ARISE trials our experts recommend 3-4L over the first 6 hours of resuscitation.
Our experts recommend 2L in the first 30 mins with a minimum of 2 large bore peripheral IVs under pressure bags pumped up to 300mmHg.
Update 2019: A pilot prospective RCT involving 109 patients showed a restrictive IV fluid resuscitation strategy (<60mL/kg/72hrs) can reduce the amount of IV fluid in patients with severe sepsis and septic shock compared to usual care, with no increase in 30-day mortality, organ failure, or adverse events. Abstract-RIFTS
Update 2023: A multicenter randomized controlled trial including 1563 patients with sepsis-induced hypotension refractory to initial treatment with 1-3L of IV fluids comparing a restrictive fluid strategy (prioritizing vasopressors and low intravenous fluid volumes) and a liberal fluid strategy (prioritizing higher volumes of intravenous fluid before vasopressor use) found that death from any cause before discharge home by day 90 was not significantly different between the two groups (14.0% vs 14.9% respectively, estimated difference -0.9%, 95% CI -4.4 to 2.6, P=0.61) (CLOVERS trial). Abstract
Venous Access for Severe Sepsis & Septic Shock
For patients who present to the ED with severe septic shock and no IV access, as a temporizing measure, consider multiple intraosseus (IO) lines. Note that the humerus has the fastest infusion rates, and so should be considered the IO location of choice for the crashing patient.
While norepinephrine, the vasopressor of choice in septic shock, can be administered through an IO or a peripheral IV safely in low doses for a short period of time, if you anticipate that the patient might require pressors, place a central line after the patient has been stabilized (usually after the first 2L of fluid) so that by the time the third liter of fluid is running the pressor has been started.
When to Stop Giving Fluids – Measuring Fluid Status & Goals of Fluid Resuscitation
Knowing when to stop fluid resuscitation is one of the most difficult aspects of sepsis management.
A simple approach to the goals of fluid resuscitation in severe sepsis and septic shock:
Once you’ve given about 2-3L of fluid, if the patient’s mean aterial pressure (MAP) is less than 65, start low dose norepinephrine, stop the fluid and get the patient to the ICU.
A three-pronged nuanced approach to the goals of fluid resuscitation in severe sepsis and septic shock:
- Clinical Factors – level of awareness, renal output, mottled skin, HR, MAP of 65 (approximate BP of 90/55), JVP
- Fluid Tolerance – point of care ultrasound for IVC width and collapsibility, fluid in the lungs and JVD
For an analysis on the value of IVC POCUS for assessing fluid tolerance visit the EDE blog
- Fluid Responsiveness –a) Passive Leg Raise Test – patient sits up in bed at a 45 degree angle and the BP is noted; then lie the patient supine and raise their legs 45 degrees – if there is an augmentation in their BP then the patient will likely benefit from more fluid (sensitivity 86%, specificity 90%) b) End-tidal CO2 c) Pulse Pressure Variability
An in depth review of Fluid Responsiveness assessment on Life in the Fast Lane
A podcast analysis of the different methods for measuring Fluid Responsiveness on Taming the SRU
Starting Norepinephrine in Severe Sepsis & Septic Shock
The current trend in critical care is to start pressors EARLY rather than waiting until the patient crashes to start pressors.
Once you’ve administered about 2-3L of fluid, if the patient’s mean arterial pressure (MAP) is less than 65, start norepinephrine at a low dose of 1-2 micrograms/min via a peripheral IV or IO or central line, titrate up to 5 micrograms/min to maintain a MAP of 65 , stop the fluids completely andtransfer fluid administration to a central line. If a MAP of 65 cannot be maintained despite 5 micrograms/min of norepinephrine then titrate the norephinephrine further to 10-15 micrograms/min and give 250-500ml Ringer’s Lactate boluses based on fluid tolerance, fluid responsiveness and serial lactate measurements.
The ARISE Trial in Severe Sepsis & Septic Shock
The ARISE Trial was a 2014 prospective RCT at multiple centers with 1600 patients with severe sepsis and septic shock that examined the benefit of protocolized Early Goal Directed Therapy which included monitoring the Central Venous Pressure (CVP) and the Central Venous Oxygenation Saturation (ScVO2) vs usual care. There was no difference in 90 day mortality between usual care and Early Goal Directed Therapy (19% in both groups).
The ARISE trial showed that monitoring CVP and ScVO2 had no added benefit, and can be removed from the Early Goal Directed Therapy algorithm as displayed in the algorithm below.
The conclusions that can be drawn from the literature to date on resuscitation goals for the patient with severe sepsis or septic shock are the following:
- Early antibiotic administration
- Adequate volume resuscitation
- Maintenance of End-organ perfusion
The PROCESS trial came to similar conclusions to the ARISE trial and is reviewed on the Boring EM blog
Scott Weingart’s emcrit podcast on the ARISE trial
Ken Milne’s SGEM podcast on the ARISE trial
Update 2015: NEJM publishes the PROMISE trial with similar results to PROCESS and ARISE. Full Article
Update 2014: Surviving Sepsis Campaign’s official update after ARISE and PROCESS Trials 2014 Full PDF
Update 2015: Surviving Sepsis Campaign’s official update after PROMISE trial Full PDF
Update 2016: Long-term beta blocker use may decrease lactate levels in severely septic patients. Abstract
The Importance of Adequate Early Post Intubation Analgesia & Sedation
Under treatment or over treatment of pain and agitation in the ED will increase the likelihood of the patient developing acute delirium, which has been associated with an increased mortality rate in ICU patients suffering from severe sepsis or septic shock.
Update 2022: A multicenter, prospective clinical trial including 388 mechanically ventilated adult patients found that 3.4% of patients experienced awareness with paralysis. Abstract
Update 2022: A secondary analysis of the SPICE-III (Sedation Practice in Intensive Care Evaluation) open label RCT found that patients under the age of 65 sedated with dexmedetomidine and propofol combination had increased mortality with increasing dexmedetomidine dose, whereas increasing the dose of propofol was associated with decreased adjusted 90-day mortality. Abstract
PAD – A Simple Mnemonic for The Order of Medications Post-Intubation Analgesia & Sedation
‘PAD’
Pain – IV Fentanyl 50-200 micrograms titrated to effect
Agitation – IV Propofol 30microgrms/kg/min or Dexmedetomidine (not available in most EDs and is very expensive)
Delirium – delirium will likely be prevented if you manage Pain and Agitation
For patients who are aggressively attempting to pull out their ETT and require immediate sedation and analgesia, consider Ketamine 0.7mg/kg IV (approx. 50mg IV), then 0.15-0.25mg/kg q5-10 mins prn titrated to effect.
Benzodiazepines may increase the incidence of delirium and prolong the time on the ventilator, and so are not favored as a first line for sedation. If you choose to use benzodiazapines, be sure to control pain first with fentanyl before any benzodiazepine is administered, and use small doses (eg: 1-2mg Midazolam)
Scott Weingart’s emcrit podcast on Post Intubation Analgesia & Sedation
EP Monthly’s review of post-intubation sedation
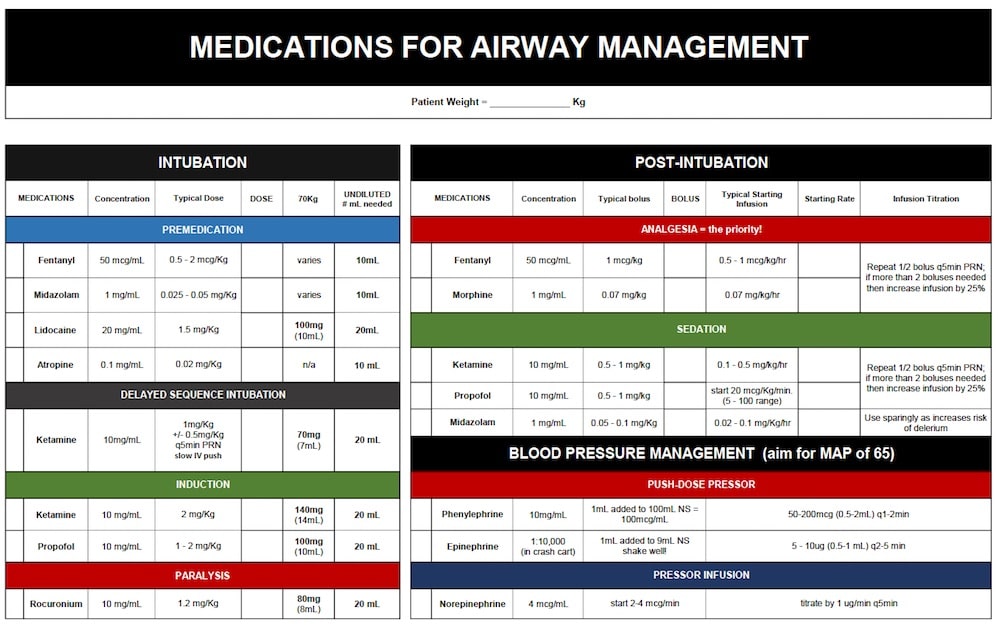
Listen to the podcast for a short bonus discussion on the rationale and indications for push dose pressors and download the pocket card PDF from emcrit.
EM Quick Hits 26 on Post Intubation Analgesia & Sedation 2021
Medications for Airway Management card PDF 2017
More on airway management on EM Cases:
Episode 8: Emergency Airway Controversies
Episode 54: Preoxygenation and Delayed Sequence Intubation
KEY REFERENCES
Annane, D. Effects of Fluid Resuscitation With Colloids vs Crystalloids on Mortality in Critically Ill Patients Presenting With Hypovolemic Shock. The CRISTAL Randomized Trial JAMA. 2013;310(17):1809-1817. doi:10.1001/jama.2013.280502. Full Text
The ProCESS Investigators. A Randomized Trial of Protocol-Based Care for Early Septic Shock. N Engl J Med 2014; 370:1683-1693May 1, 2014DOI: 10.1056/NEJMoa1401602 Abstract
The ARISE Investigators and the ANZICS Clinical Trials Group. Goal-Directed Resuscitation for Patients with Early Septic Shock. N Engl J Med 2014; 371:1496-1506October 16, 2014DOI: 10.1056/NEJMoa1404380. Abstract
Fraser, Gilles L., John W. Devlin, Craig P. Worby, Waleed Alhazzani, Juliana Barr, Joseph F. Dasta, John P. Kress, Judy E. Davidson, and Frederick A. Spencer. 2013. Benzodiazepine Versus Nonbenzodiazepine-Based Sedation for Mechanically Ventilated, Critically Ill Adults. Critical Care Medicine. Abstract.
Barr, J. et al. Clinical Practice Guidelines for the Management of Pain, Agitation, and Delirium in Adult Patients in the Intenstive Care Unit. Crit Care Med. 2013;41:263-306. PAD Guidelines PDF
Dr. Helman, Dr. Himmel and Dr. Weingart have no conflicts of interest to declare





“For patients who are aggressively attempting to pull out their ETT and require immediate sedation and analgesia, consider Ketamine 7mg/kg IV (approx. 50mg IV), then 0.15-0.25mg/kg q5-10 mins prn titrated to effect.”
I think it should be 0.7mg/kg IV of ketamine.
Thanks for pointing out the error – it has been fixed accordingly.