The problem until now has been that the older the patient, the more likely the D-dimer is to be positive whether they have a PE or not, so many of us have thrown the D-dimer out the window in older patients and go straight to CTPA, even in low risk patients. If you are a risk averse doc, this strategy will lead to over-utilization of resources, huge costs, length of stay, radiation effects etc; and if you’re not so risk averse, then you might decide not to work up the low risk older patient at all and miss clinically important PEs.

Published by Anton Helman Sept 2014
Cite this podcast as: DeWit, K, Kline, J. Age Adjusted D-dimer with Jeff Kline and Jonathan Kirschner. Emergency Medicine Cases. September, 2014. https://emergencymedicinecases.com/journal-jam-1-age-adjusted-d-dimer-jeff-kline-jonathan-kirschner/. Accessed [date].
Update 2015: Global Emergency Medicine Journal Club: A Social Media Discussion About the Age-Adjusted D-Dimer Cutoff Levels to Rule Out Pulmonary Embolism Trial. Annals of EM, published online March 31st, 2015 Full PDF
Expert Peer Review of this Journal Jam podcast
Dr. Kerstin De Wit (née Hogg), MBChB, MD, MRCP, FCEM, FRCPC. Divisions of Thrombosis & Emergency Medicine, Department of Medicine, McMaster University, Canada. Prepared in September, 2014.
Low Risk Patients…
I agree that cancer and recent hospitalization are risk factors for pulmonary embolism (PE). The Wells score helps to define the low risk population, and includes the clinical gestalt question ‘is PE the most likely diagnosis?’ D-dimer should not be used to rule out PE in the intermediate or high risk patients (or according to the modified Wells PE score – the PE likely group [e.g. score > 4.0]). In the conclusion you state if your clinical gestalt is high, don’t use age adjusted D-dimer, but actually I would extend that statement to say you shouldn’t use D-dimer at all if you have a compelling suspicion.
What about the VQ scan?
A lot of the discussion focuses on CT Pulmonary Angiogram (CTPA). It seems to me that this is a great time to remind emergency physicians that we can also order VQ scans. We should consider VQ as first line-imaging for young patients (decreasing the risk of lung and breast cancer in later life). In other words, if you are a ‘risk averse’ clinician, you should utilize VQ. The path of most harm will include ordering CT scans on lots of young people with positive D-dimers. Many community hospitals have access to a regional Thrombosis unit where the VQ scan can be performed the next day.
The second issue with CT is the ‘over diagnosis’ of PE (or the false positive rate). Many patients are being diagnosed with single subsegmental PE on CT. CT does not visualize a clot, instead it demonstrates a filling defect (causes of which could be many). Emerging evidence is compelling that these are false positive scans. VQ avoids this issue.
Prevalence & your patient population
As a Thrombosis and Emergency clinician, who has worked in both the UK and Canada, I am in a prime position to reflect more on the differences in various countries. The prevalence of PE amongst all patients investigated for PE (starting with D-dimer and clinical probability) is 17% in Manchester. No one ever goes to their GP before attending the Emergency in Manchester. People have an even lower threshold for going to Emergency in the UK than they do in Canada. As such, we were able to rule out PE in around 40% using the Wells score and D-dimer because many people are young and healthy.
The main difference between working in the British ED and in a Canadian ED is that it is hard to get a CT scan in the UK. I mean, very hard. It is impossible to get a CTPA over night and difficult to get a CT during the day. Furthermore it is time consuming to arrange CT. In general, our younger patients (age <40) have VQ scanning.
The effect of this is that the Emergency physician makes very sure that PE is on their differential diagnosis before embarking on diagnostic testing. We always measure D-dimer on low risk patients to screen them prior to ordering imaging. Sometimes I have seen patients in Canada going straight to CT without ever having the Wells score or D-dimer assessment because it is simply faster.
Considerations when ruling out PE
The ideal Emergency Department screening test for PE reduces the number of diagnostic imaging tests. I especially want to reduce the number of radiological investigations I perform on young people and pregnant women. I also want to know what the post-test prevalence for PE is when I have ‘ruled out’ PE to inform my discussion with the patient. As with any rule out test, we have to recognize that there is still a small chance the patient actually may have a PE, and we should ask them to return if their symptoms worsen. When they do return, we should re-evaluate from the beginning, in the same way we deal with head injured patients.
Bottom Line
Using this study could reduce the number of CT scans performed on people over the age of 50. I am uncertain that here in Canada there will be so many low risk patients who are age over 50. The utility of the age adjusted D-dimer, may be modest at best, and we should recognize that all ‘rule out’ strategies have a small false negative rate.
Dr. Jeff Kline’s New Proposed Rule Out Pulmonary Embolism Algorithm
Note that this algorithm has yet to be published in any medical journal, is not peer reviewed, and that it incorporates the Age-adjusted D-dimer
Reference and permission by personal communication
Update 2015: Age-adjusted D-dimer accuracy and clinical implications for suspected PE. Abstract
Update 2015: Global Emergency Medicine Journal Club: A Social Media Discussion About the Age-Adjusted D-Dimer Cutoff Levels to Rule Out Pulmonary Embolism Trial. Annals of EM, published online March 31st, 2015 Full PDF
Dr. Helman and Dr. Kerstin De Wit (née Hogg) have no conflicts of interest to declare.
Key References for this Journal Jam podcast
Righini M et al. Age-Adjusted D-Dimer Cutoff Levels to Rule Out Pulmonary Embolism: The ADJUST-PE Study. JAMA. Mar 2014; 311(11):1117-24. PMID: 24643601
Kirschner JM, Kline JA. Is it time to raise the bar? Age-adjusted D-dimer cutoff levels to exclude pulmonary embolism. Ann Emerg Med. 2014 Jul;64(1):86-7. PMID: 24951413.
Academic Life in Emergency Medicine Global Emergency Medicine Journal Club on Age-Adjusted D-dimer

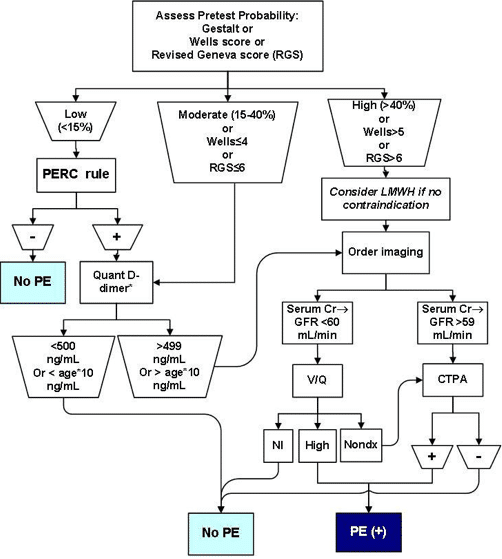



The box “>499 OR > Age x 10” box is the kicker. So we still say “OR”, so are we not committing to the use of the age adjusted D-dimer. Seems like it’s then up to the clinician. So it sounds like it’s up to the clinician and that we aren’t committing to this age adjusted d-dimer
Thanks for the comment Noah. Just to clarify, Dr. Kline is suggesting that if a patient is deemed low risk by the Well’s score but is PERC positive then they should go on to have a D-dimer. If the patient is under 50 years of age then a D-dimer of <500ng/L rules out PE, but if the patient is over 50 years old then a D-dimer that is less than the patient's Age X 10 rules out PE.
How’s about trimester adjusted d-dimer?
I believe Dr. Kline has been working on a trimetster adjusted D-dimer, however in my conversations with Phil Wells, he believes it is a hopeless endevour. We will have to wait and see.
Anton,
Thanks again for the great podcast. I was just reading your algorithm above on PE.
Two questions/comments:
1. The algorithm suggests to only apply the PERC rule for low risk Wells.
I think this is doing PERC a disservice. If you look at the data (meta analyis reference below) the low risk Wells has a prevalence of PE of 2.9%, moderate wells has a prevalence around 15% (closer to the inclusion criteria for PERC). By applying PERC to a population with a prevalence of 2.9% to bring the probability slightly below 2%, seems fairly pointless and markedly different from how it was validated (<15% CPTP, reference below).
I’ve been advocating that the PERC rule (with gestalt <15%) should be applied before any decision rule or d-dimer. Did Kline address this?
2. Did Kline talk about the issue of using age-adjusted d-dimer with our assay that has a cut-off of 230? I spoke with our lab medicine department and they really don't know how to process this new info and changing tests is not an insignificant thing for them.
Many thanks for giving this some thought and for your work.
References:
Lucassen W, Geersing G-J, Erkens PM, Reitsma JB, Moons KG, Büller H, et al. Clinical decision rules for excluding pulmonary embolism: a meta-analysis. Annals of Internal Medicine. 2011;155(7):448–60.
Singh B, Parsaik AK, Agarwal D, Surana A, Mascarenhas SS, Chandra S. Diagnostic Accuracy of Pulmonary Embolism Rule-Out Criteria: A Systematic Review and Meta-analysis. Annals of Emergency Medicine. 2012 Jun;59(6):517–20.e4.