I had the great pleasure of meeting Dr. Mike Winters on his first ever visit to Canada at North York General’s Emergency Medicine Update Conference, where he gave two fantastic presentations. His credentials are impressive: He is the Medical Director of the Emergency Department, Associate Professor in both EM and IM, EM-IM-Critical Care Program co-director and Residency Program Director of EM-IM at the University of Maryland in Baltimore.
Sometimes we are so caught up with the job we need to get done during cardiac arrest that we forget about the important and profound effect that this event has on patients’ families. On this Best Case Ever Dr. Winters tells the story of witnessing his grandfather’s cardiac arrest, being present in the ED during the resuscitation attempts, and how that experience has coloured his practice. We discuss some pearls on communication with patients’ families after death, colour-coded cardiac arrest teams and how to integrate POCUS into cardiac arrest care while minimizing chest compressions.
Published by Anton Helman, May 2016
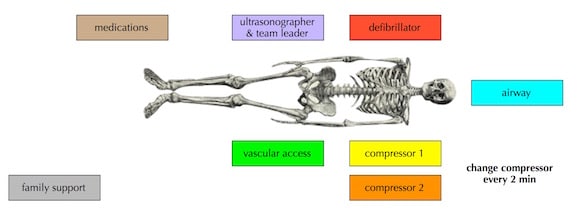
Colour Coded Cardiac Arrest Teams
Some centres have implemented colour coded badges for each member of the cardiac arrest team with specific locations and tasks for each member as outlined in the following diagram by Reuben Strayer:
Reuben Strayer’s cardiac arrest algorithm incorporating colour coded tasks and POCUS here.
Key Elements in Breaking Bad News
- Bring a social worker or nurse or someone who can spend time with the family after you leave the room
- Invite everyone to sit down, and sit down yourself
- Have tissue paper available in the room and offer it prn
- Use the words “died” or “dead” rather than “passed away” or “is no longer with us” early in the conversation
- Explain in simple, clear terms the events that transpired in as few sentences as possible
- After you tell the family that their relative has died pause and wait until they say something rather than rushing to the next steps
- Assure them that everyone involved (witnesses, EMS, ED staff) did everything they could
- Ask them if they have any questions
- When you leave the room tell them how long you will be in the department for and who to direct any further questions to
SPIKES mnemonic for Breaking Bad News
STEP 1: S—SETTING UP the Interview
STEP 2: P—Assessing the Patient‘s PERCEPTION
STEP 3: I—Obtaining the Patient‘s INVITATION
STEP 4: K—Giving KNOWLEDGE and Information to the Patient
STEP 5: E—Addressing the Patient‘s EMOTIONS with Empathic Responses
STEP 6: S—STRATEGY and SUMMARY
Integrating POCUS into Cardiac Arrest Care
- narrowing the differential diagnosis of PEA arrest (tension pneumothorax, massive pericardial effusion with tamponade, massive PE)
- assessing for pulse to minimize chest compression interuptions (manual pulse checks are notoriously inaccurate)
- assess for cardiac standstill (note that 2-16% of patients will get return of spontaneous circulation despite a lack of cardiac activity on ultrasound)
- confirmation of IO line placement using Doppler
- confirmation of endotracheal tube placement
Dr. Helman and Dr. Winters have no conflicts of interest to declare.
Key References
Baile WF, Buckman R, Lenzi R, Glober G, Beale EA, Kudelka AP. SPIKES-A six-step protocol for delivering bad news: application to the patient with cancer. Oncologist. 2000;5:(4)302-11.
Ptacek JT, Eberhardt TL. Breaking bad news. A review of the literature.JAMA 1996;276:496-502.
Blyth L, Atkinson P, Gadd K, Lang E. Bedside focused echocardiography as predictor of survival in cardiac arrest patients: a systematic review. Acad Emerg Med. 2012;19(10):1119-26.
Other FOAMed Resources
For more on breaking bad news, SPIKES mnemonic and communication skills around the death of a patient go to Episode 51
For the key elements of breaking bad news according to Chris Nickson, visit Life in the Fast Lane
For Justin Morgenstern’s take on breaking bad news visit First10EM
Liz Crowe at St. Emlyn’s writes on breaking bad news
For more on POCUS for cardiac arrest visit REBEL EM and Sinai EM
Rob Simard’s Best Case Ever on POCUS in pediatric cardiac arrest
Likelihood of achieving ROSC in a patient with no cardiac activity on POCUS on Scancrit




[…] podcast med dr Winters personliga upplevelser, tips om info till anhöriga och lite mer. Lugnt, vettigt och inte så […]