Written by Dr. Paul Hannam, introduction by Dr. Howard Ovens, August 2015
Access and Equity in the ED: Who Speaks for the Most Vulnerable?
I view the emergency department as a safe refuge, a modern-day secular sanctuary. We are the one health-care service that never turns anyone away; we provide shelter to the homeless on cold winter nights, safety for battered women, and food for the hungry. I have always felt this “sanctuary” role was part of the core mission of the ED, one with a great potential for improving lives, or at least providing comfort.
I’m passionate about preserving the ED as a safe harbour, but how do we measure our performance in this role? What outcomes do we follow and what data do we require to meet societal expectations around transparency and accountability? Do some patients wait longer than others in our EDs to be seen or to receive analgesics, and are we selective about who gets expensive or life-saving interventions? The research on these questions is conflicted; some authors have suggested staff biases do have an impact on these things1 while others feel the reasons behind varying treatment are complex and not simply related to prejudice2; most of our staff would reject any notion that they discriminate. Better and more comprehensive data could help clarify these important issues.
The regional health authority I report to is interested in collecting data on patients such as income, sexual preferences, and religious identity to inform analyses of the challenges vulnerable groups face in accessing services and to help develop strategies to address any gaps. While embracing the intentions, ED leaders have been concerned about the process of data collection and potential unintended effects on patients and staff. In this guest blog, Dr. Paul Hannam, Director of the ED at Toronto East General Hospital (an ED serving a diverse population with a high proportion of disadvantaged patients) discusses some of the subtler aspects of these issues.
– Dr. Howard Ovens
Health Equity, Trust and Data Collection in the Emergency Department
It is after midnight and I am thinking about one of my patients as I clean up after my shift. The patient, whom I’ll call “Amir,” was a middle-aged male with a laceration on his back. He had dressed the wound and finished his shift as a taxi driver before coming to the ED accompanied by his two children. Although not specifically relevant to his care, I guessed Amir to be from the Middle East – I asked about his background as a lead in to inquire about his immunization status. English was not his first language, but we were able to communicate well enough. He seemed formal if slightly distant.
I also recall the look Amir gave me as I exposed the injured area and noted a series of scars nearby. It was clear he did not want to talk about these scars. One of the staff I work with had endured torture in another country before arriving in Canada. From her I learned enough to recognize the signs and to know when not to talk about it. As providers, we need to recognize the imbalance in our relationship with patients. If I were to ask about the scars, would it be because I can help him, or because I am curious? Regardless, Amir did not want to talk about his past tonight with his family present. Looking at the record in front of me, I noted the blank spaces where he had declined to provide a phone number or emergency contact. This is not uncommon among those who have been mistreated by authority. I asked if he needed anything else as we finished up — a purposely open-ended question. Amir paused while looking at me and said, “No, thank you.”
For the most vulnerable groups in our community, the emergency department represents more than a location to cast a broken bone or have some stitches placed. We see first-hand the effects of poverty, discrimination, and abuse in the patients we meet. In response, EDs routinely feed and provide shelter for the homeless, arrange support for the frail elderly in the community, manage all phases of addiction and substance abuse, and provide a safe environment for psychiatric assessment during a crisis. No patient is turned away – this remains fundamental both to the practice of emergency medicine and to the principle of health equity. In the Canadian context, health equity is “a means of realizing the principles of the Canada Health Act, which among the central tenets is that residents should have access to health care without financial or other barriers as obstructions.”[1]
In recent years there has been a move toward data collection at the point of care in order to measure differences in access to care. However, while a visit to the ED may represent a useful opportunity for health equity data collection, my encounter with Amir prompted me to reflect on the appropriateness of this activity. When we ask such probing questions before a patient receives care, do the benefits outweigh the risks?
Value of data
In Ontario, the province where I practise, collecting personal information related to health equity has become a priority, particularly since the discontinuation of the mandatory Canadian long-form census in 2010. At that time, prominent voices within the Canadian Medical Association pointed out the implications of a switch from mandatory to voluntary reporting and the subsequent risk of under-representation of disadvantaged populations.[2] [3] Health equity information collected on a voluntary basis at the point of care has similar limitations.
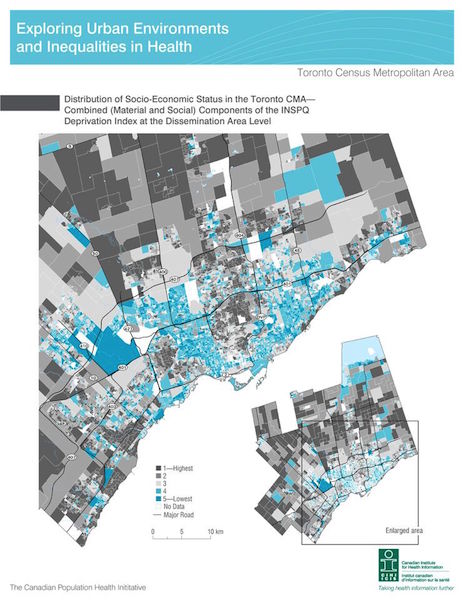
One reason to collect individual data is to better define the community we serve. However, I can already see the distribution of factors related to health outcomes in my community using a well-validated measure of health inequity called the “deprivation index.” The deprivation index has been shown to correlate both with increased visits to the ED for care[4] as well as increased mortality over time.[5] This index has been tested in many settings and meets the essential criteria of having predictive validity, reliability, and responsiveness to local changes.[6]
If we ask socio-economic questions of all our patients at the point of care, we need to be sure that the information is not already available, that it will be sufficiently complete to be useful, and that we have clarity about how it might be applied.
Trust in the clinical setting
A second issue related to collecting personal information relates to trust. As providers we need to ask patients a variety of personal questions to provide proper health care. Our patients answer these questions because they trust that we need the information in order to help, we will keep the information private, and they won’t be suffer as a result of the answer. The therapeutic relationship is built on this trust.
Unfortunately, studies of patient perceptions consistently show that vulnerable populations are also the most likely to distrust socio-demographic questions not directly related to their own care. A study published in 2013 confirmed this to be the case in Ontario.[7] In the qualitative portion of the study, the primary areas of concern included privacy of the information, potential discrimination based on the information, and relevance/how the information would be used.
Another Canadian qualitative study of both emergency department patients and community leaders reported “. . . collecting ethnicity data in a clinical context is not a neutral process. The potential harms to individuals are considerable and include harms that may directly contribute to exacerbating inequities and serve as barriers to healthcare access.”[8]
Competing priorities
Finally, we need to validate any questions we ask our patients before prioritizing one over another, or asking them of every patient we meet. One article lists 39 ED-based public health initiatives that are advocated in peer-reviewed literature, ranging from alcohol-abuse detection to screening for domestic violence to surveillance screening for HIV.[9] All of these are important goals for the health of a community, but it isn’t practical to prioritize them all. As one author suggests, “In a world without resource constraints the issue of public health screening in the ED might be moot, the ED could become the ‘Everything Department.’ ”[10] Just as important, there is variable evidence regarding patient related outcomes for these initiatives. My impression is that a clear link to a specific intervention determines the success or failure of an initiative.
We know from experience and from population studies that certain groups have less access to health services. We also know that these groups are the most likely to be suspicious of authority and of how personal information is used. Establishing trust can be a challenge in a fast-paced environment such as an emergency department. Asking potentially sensitive questions of patients at time when they are most in need can provide us with vital information for health-care planning, but we need to be able to clearly articulate:
- how the questions meet the established criteria mentioned above, such as prospective validation;
- how exactly the information will be used to address health inequities; and
- why this should be a priority over other public health interventions in an urgent-care setting.
Ideally, effective communication on these topics would reach the most vulnerable groups prior to them presenting to an ED.
By providing a safety net to the most vulnerable and to the broader population, the practice of emergency medicine represents health equity in action. In this role, above all else we need the trust of the community we serve.
For my patient, I was able to address his injury and arrange for appropriate follow-up care given the resources available to him. I know that because it was relevant to him at the time and because we talked about it. I didn’t ask my patient how much money he made, what specific language he spoke at home, or what his sexual orientation was. I’m not sure these would have helped his recovery given the information I already had. However, I am sure he would not have wanted to answer such questions, and that likely he has very good reasons to be suspicious of people in positions of authority. Despite our vastly different backgrounds, income levels, and the differences in how we experience Canadian culture, we were able to establish the trust necessary to communicate effectively. I also believe he trusts our hospital enough to return to the emergency department if he should need care.
– Dr. Paul Hannam
References
1. Solomon et al. Defining Health Equity HealthcarePapers 2014;14(2):62-65
2. CohenM et al. Ideology trumps evidence with new voluntary survey CMAJ 2010;182(12):E541
3. Collier R Long-form census change worries health researchers CMAJ 2010;182(12):E563-E564
4. Tozer A et al. Socioeconomic status of emergency department users in Ontario, 2003 to 2009. CJEM 2014;16(3):220-225
5. Ross N et al. The Contribution of Neighbourhood Material and Social Deprivation to Survival: A 22-Year Follow-up of More than 500,000 Canadians. Int. J. Environ. Res. Public Health 2013;10:1378-1391
6. Pampalon R et al. Validation of a deprivation index for public health: a complex exercise illustrated by the Quebec index Chronic Diseases and Injuries in Canada 2014;34(1):12-22
7. Kirst M et al. Sociodemographic data collection for health equity measurement: a mixed methods study examining public opinions International Journal for Equity in Health 2013;12:75
8. Varcoe C et al. Harms and benefits: Collecting ethnicity data in a clinical context Social Science & Medicine 2009; 68:1659–1666
9. Kelen G Public Health Initiatives in the Emergency Department: Not So Good for the Public Health? Acad Emerg Med 2008;15(2):194-196
10. Gaddis G et al. The Provision of Public Health Services in the Emergency Department: “Begin with the End in Mind” Acad Emerg Med 2008;15(2):198-200
Dr. Paul Hannam is Chief and Medical Director of the Department of Emergency Medicine at Toronto East General Hospital.
Twitter: @PHannam123
Email: phann@tegh.on.ca
Dr. Helman, Dr. Hannam & Dr. Ovens have no conflicts of interest do declare




[…] of cohort D patients as a “safe refuge and modern-day secular sanctuary” — as described in a recent blog on this […]