Best Case Ever is a 5-20 minute podcast where an Emergency Medicine Cases guest expert describes a practice changing case, what they learned from it, and clinical pearls and pitfalls you can use on your next shift. Tacit knowledge sharing at it’s best.
Best Case Ever 38 Sickle Cell Acute Chest Syndrome
Sickle Cell Acute Chest Syndrome remains the leading cause of death in patients suffering from Sickle Cell Disease. In his Best Case Ever, Dr. Richard Ward, a hematologist with a special interest in Sickle Cell Disease, describes a case of a Sickle Cell Disease patient who presents with what appears to be a simple pain crisis, but turns out to be a devastating Acute Chest Syndrome. He gives us the key clinical pearls and pitfalls to make this often elusive diagnosis early so that life-saving treatment can be initiated in a timely manner. This is in anticipation of the upcoming episode on The Emergency Management of Sickle Cell Pain Crisis with Dr. Ward and Dr. John Foote.
Best Case Ever 37 Neonatal Lazy Feeder
On this EM Cases Best Case Ever Dr. Anthony Crocco, the Head and the Division Head of Pediatric EM at McMaster University and Medical Director of Pediatric Emergency Medicine at Hamilton Health Sciences Hosptial, discusses an approach to the neonatal lazy feeder and why we should abandon the use of codeine in pediatrics as well as in breastfeeding mothers. The approach to the neonatal lazy feeder should be considered as an approach to altered level of awareness with a wide differential diagnosis, and there is one question that should always be asked of the neontal lazy feeder....
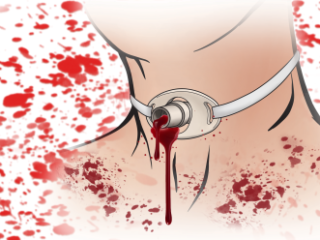
Best Case Ever 36 Tracheo-innominate Fistula
In this Best Case Ever with Dr. Scott Weingart, the brains behind EMcrit.org, we hear the devastating story of a tracheostomy gone bad. Dr. Weingart shares with us what he has learned about how to manage massive hemoptysis in tracheostomy patients, and in particlar, a step-wise approach to managing a tracheo-innominate fistula. We discuss the balance between providing maximal aggrressive critical care while maintaining a deep respect for the risks associated with the procedures we perform. Recorded at North York General's EM Update Conference 2015.
Best Case Ever 35: Taking Action in Emergency Medicine
In anticipation of our series of podcasts on Diagnostic Decision Making with Dr. Walter Himmel, Dr. Chris Hicks and Dr. David Dushenski we have Dr. Hicks presenting his Best Case Ever. Taking action in Emergency Medicine requires not only careful consideration of the best evidence, the experience of the clinician, the patient's values and the system that you work in, but also the will to act. Dr. Hicks describes a case of a patient who suffers a cardiac arrest, where the diagnosis is quite obvious to everyone in the room (and the required action is as well), yet a delay in treatment occurs nonetheless.
Best Case Ever 34: Inferior MI Presenting with Abdominal Pain
In a previous Best Case Ever, 'Thinking Outside the Abdominal Box', Dr. Brian Steinhart reviewed some important can't-miss-diagnoses that can present elusively with abdominal pain. In this Carr's Cases Series on Inferior MI Presenting with Abdominal Pain, we continue in the theme of 'Thinking Outside the Abdominal Box' with David Carr explaining how he figured out that a man presenting with classic biliary colic was diagnosed with an inferior MI with right ventricular extension.
Best Case Ever 33: Over-correction of Hyponatremia
Rapid over-correction of Hyponatremia can have devastating consequences: for one, osmotic demyelination syndrome (ODS) can result in destruction of the pons and a locked-in state. We don't see ODS very much as it's onset is delayed and usually sets in after the patient is admitted to hospital (or worse, sent home). Nonetheless, we need to know how to manage Hyponatremia in the ED so that we prevent ODS from ever happening. In this Best Case Ever, Dr. Melanie Baimel describes the case of a young woman who came in to the ED after drinking alcohol and taking Ecstasy, wanted to leave AMA after her Hyponatremia had inadvertently been corrected too rapidly, and the conundrum that ensues. In the upcoming episode, Dr. Baimel and the first ever Internal Medicine specialist on EM Cases, Dr. Ed Etchels, discuss a rational step-wise approach to managing Hyponatremia, tailored for the EM practitioner; when you might consider giving DDAVP in the ED, the best way to correct Hyponatremia, how to manage the patient who's Hyponatremia has been corrected too quickly, and an easy approach to the differential diagnosis. Get a sneak peak at the algorithm that will be explained and reviewed in the upcoming episode...... [wpfilebase tag=file id=577 tpl=emc-play /] [wpfilebase tag=file id=578 tpl=emc-mp3 /]