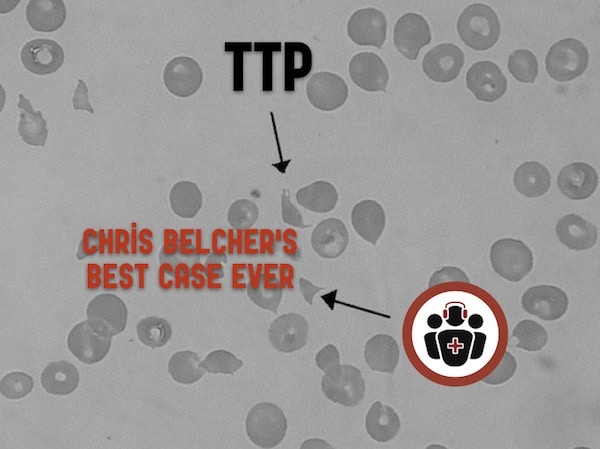
As EM Cases has grown and expanded over the past 7 years I’ve had the pleasure of working with a team of talented people. This Best Case Ever was produced by two all-star EM residents from Ottawa, podcaster Dr. Rajiv Thavanathan and editor Dr. Richard Hoang. In this all-resident Best Case Ever we interview Dr. Chris Belcher from University of Kentucky about TTP – Thrombotic Thrombocytopenic Purpura, that rare but often elusive clotting disorder that picks off multiple organs and has a near 100% mortality rate without treatment…
Podcast produced by Rajiv Thavanathan, edited by Richard Hoang and Anton Helman December, 2016
-
TTP pentad mnemonic = FAT RN
- Fever (in only 50%)
- Anemia (microangiopathic hemolytic anemia presenting with severe fatigue)
- Thrombocytopenia (often with purpura)
- Renal (sometimes manifests as dark urine)
- Neuro Symptoms (almost any neurologic presentation including altered level of awareness, seizures, hemiplegia, paresthesias, visual disturbance, and aphasia)
All features do not need to be present for the diagnosis to be made. Only 20-30% present with the classic pentad. If a patient has three or more of this pentad with schistocytes on the blood smear and a normal INR/PTT, they likely have TTP.
Diagnoses often confused with TTP
- HUS (Hemolytic Uremic Syndrome)
- ITP (Immune Thrombocytopenic Purpura)
- DIC (Disseminated Intravascular Coagulation)
It is important to distinguish TTP from HUS, ITP and DIC based on clinical presentation and blood tests because they are managed differently.
HUS vs TTP: TTP usually has more CNS involvement whereas and HUS usually has more severe renal involvement. In HUS, a recent history of diarrhea is more often present.
ITP vs TTP: Patients with ITP are usually not very sick and have normal red cells whereas patients with TTP are usually very sick with schistocytes on blood smear.
DIC vs TTP: Patients with DIC usually have multiple sites of significant bleeding, significantly elevated INR, PTT and D-dimer, whereas patients with TTP usually don’t bleed overtly and have normal or mildly elevated INR, PTT and D-dimer.
Indications for first line therapy with plasma exchange in TTP
Plasma exchange is indicated in the presence of microangiopathic hemolytic anemia (schistocytes, elevated LDH, and indirect hyperbilirubinemia) and thrombocytopenia in the absence of other obvious causes such as DIC.
Dr. Belcher Dr. Thavanathan, Dr. Hoang and Dr. Helman have no conflicts of interest to declare.
References
Scully M., Hunt B.J., Benjamin S., et al. Guidelines on the diagnosis and management of thrombotic thrombocytopenic purpura and other thrombotic microangiopathies. Br J Hematol 2012;158:323-335.
Sadler JE. Thrombotic thrombocytopenic purpura: a moving target. Hematology Am Soc Hematol Educ Program. 2006:415-20. Review.
Other FOAMed Resources on TTP
EM Cases Episode 37 Transfusions, anticoagulants and bleeding
Fantastic review of Thrombotic Thrombocytopenic Purpura on EMDocs by Brit Long




Why in the world did this patient with TTP have a pH of 6.1, bicarb 3 latctate of 28. The only cases I have seen with lactates that high are metformin overdoses