This EM Cases episode is Part 1 of The Highlights of The University of Toronto, Divisions of Emergency Medicine, Update in EM Conference from Whistler 2015 with Paul Hannam on Pearls and Pitfalls of Intraosseus Line Placement, Anil Chopra on who is at risk and how to prevent Contrast Induced Nephropathy, and Joel Yaphe on the Best of EM Literature from 2014, including reduction of TMJ dislocations, the TRISS trial (on transfusion threshold in sepsis), PEITHO study for thrombolysis in submassive PE, Co-trimoxazole and Sudden Death in Patients Receiving ACE inhibitors or ARBs, the effectiveness and safety of outpatient Tetracaine for corneal abraisons, chronic effects of shift work on cognition and much more…
Recorded February 2015. Written Summary & Blog Post Written by Keerat Grewal & Edited by Anton Helman, March 2015.
Cite this podcast as: Hannam, P, Chopra, A, Yaphe, J, Helman, A. Whistler’s Update in EM Conference 2015 Highlights Part 1. Emergency Medicine Cases. March, 2015. https://emergencymedicinecases.com/episode-61-whistlers-update-in-em-conference-2015-highlights-part-1/. Accessed [date].
Intraosseus (IO) Line Pearls – Dr. Paul Hannam
Choosing and Landmarking a Site for an Intraosseus Line
Proximal Tibia: Find the tibial tubercle, move 2cm inferiorly and 1 cm medially and insert the IO line 90 degrees to the bony plane

Advantages of Humerus site: faster infusion rates and is easily landmarked.
Disadvantage of Humerus site: The arm must be immobilized in adduction, across the abdomen to prevent dislodging the needle. Requiring the arm to be immobilized may interfere with other resuscitative measures.
Avoid all bone sites where there is: a fracture, previous attempt, trauma or circulatory compromise proximal to the site
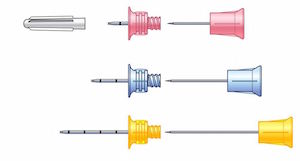
Choosing an IO Needle Length
EZ-IO kits have three needle lengths (15mm, 25mm and 45mm) and comes with weight-based recommendations for which needle to use for a given patient. Rather than using weight-based recommendations, our experts find it more useful to select the needle length according to the soft tissue thickness between the skin and bone of the patient at the given site. Estimate the soft tissue thickness and choose the needle that would accommodate that thickness. It is better to overestimate than underestimate the length of the needle required.
Update 2015: The squeeze test is an additional method to confirm IO placement, check it out on ALiEM.
Stabilizing and Securing the IO Needle
Ensuring that the needle does not move once it is placed is vital to avoiding leaking from the site. Even small movements of the needle can increase the diameter of the hole in the bone resulting in a leak from the IO site. Dislodgement or leak of the IO site increases the risk of compartment syndrome.
Two methods to securing the IO needle:
- Use the stabilizer supplied with the EZ-IO kit.
- Stack gauze on both sides of the IO needle and tape down.
Flushing the IO Line
After stabilizing the IO needle, you need to flush the IO with 10cc of normal saline to clear away bone fragments and allow good flow through the line.
It is important to flush the IO SLOWLY (over 8-10 seconds) to avoid causing a potentially lethal fat embolism.
Cadaver literature has shown that generating > 2000 mmHg of pressure through bone results in an increased risk of fat emboli. Rapidly flushing an IO line with 10cc over 1 second can generate pressures of approximately 3000 mmHg and therefore, increases the risk of a fat embolus.
Infusing fluids through an IO Line
For patients who require resuscitation, infuse fluids using a pressure bag with pressure pumped up to 300mmHg.
Infusing fluids without a pressure bag by gravity alone, will not generate enough pressure to adequately resuscitate your patient.
Reducing Pain Associated with IO infusion Using the 2-2-2 Lidocaine Rule
Needle placement is not a very painful aspect of IO insertion. The infusion of fluids is more painful. Consider using lidocaine prior to the infusion
Use The 2-2-2 rule:
- 2% lidocaine without preservative (from the crash cart) and without epinephrine
- 2 cc of lidocaine
- Wait 2 minutes for analgesic effect
Removing an IO Needle
Use any syringe with a luer lock and screw it onto the top of the IO needle. Then pull out the IO needle using the syringe.
Contrast-Induced Nephropathy – Dr. Anil Chopra
Defining Contrast-Induced Nephropathy (CIN)
- Occurs within 1-3 days of receiving CT contrast
- Rise in creatinine of 25% or more; or
- Absolute rise in creatinine of 44
Risk Factors for Contrast-Induced Nephropathy
Patients with no risk factors for CIN have negligible risk for CIN
The most important Risk factors for CIN include:
- History of Diabetes
- History of CHF
- History of Nephropathy
- Creatinine clearance <45
- Recent CT contrast study
Risk of Contrast-Induced Nephropathy
In the largest ED study from 2013 of 5006 patients, the risk of CIN at 48-96h after a contrast enhanced CT study in the emergency department was approximately 7% (1).
Risk factors for developing nephropathy were largely associated with comorbidities (as listed above), and not age.
Consequences of Contrast-Induced Nephropathy
The majority of patients with CIN improve within 72 hours, almost always within 1 week.
Less than 1% patients of patients with CIN require dialysis. However, when patients require dialysis as a result of CIN, they have a high mortality rate; >50% die within that hospital admission, 80% die within two years.
Preventative Measures for Contrast Induced Nephropathy by Creatinine Clearance
- Creatinine clearance > 45: no issue with contrast
- Creatinine clearance 30-45: give 300-1000mL bolus of crystalloid fluid before AND after study, discuss contrast options with your radiologist (non-ionic contrast, low-osmolality contrast or lower amount of contrast)
- Creatinine clearance < 30: consider alternative study (i.e. ultrasound), consider consultant opinion (e.g. surgery), consider non-contrast scan. If contrast deemed imperative, give 300-1000mL bolus of crystalloid fluid before AND after study. Discuss with your radiologist.
NAC and Bicarbonate to Prevent Contrast-Induced Nephropathy
The use of NAC and Bicarb for prevention of CIN is controversial. There are no good ED-based studies that have definitely shown either of these measures to significantly decrease the risk of CIN beyond giving a fluid bolus before and after the study, however some hospital protocols have NAC and/or Bicarb as options for the highest risk patients.
Metformin and Contrast CT
Patients who are taking metformin, do not require an alteration in the study you are ordering or the contrast. After they receive the contrast, some radiology departments advise patients to hold their metformin for a certain number of days.
Metformin does not increase the risk of CIN.
Metformin increases the risk metabolic acidosis.
Update 2015: What is the risk of CT contrast induced nephropathy? Check out an in-depth analysis on BoringEM.
Update 2015: For a detailed evidence-based analysis that questions whether CT contrast nephropathy even exists visit: PulmCrit: Pulmonary Intensivist’s Blog
Update 2015: How effective are risk prediction models for contrast induced nephropathy? Check out this systematic review published in the BMJ.
Best of the 2014 Emergency Medicine Literature – Dr. Joel Yaphe
TRISS Study: Lower versus Higher Hemoglobin Threshold for Transfusion in Septic Shock (2)
Background: Previous recommendations for early goal directed therapy in sepsis, aimed for a hematocrit of > 30%, and Hb >90.
This was a multi-center study of ICU patients in septic shock. Patients were randomized into two groups 1) Hb > 90, 2) Hb > 70. The primary outcome was death at 90 days.
No difference in the primary endpoint was found between two groups.
Take home message: Patients in septic shock with Hb of 70 or above generally do not require RBC transfusion.
Topical Tetracaine Used for 24 Hours is Safe and Rated Highly Effective by Patients for the Treatment of Pain Caused by Corneal Abrasions (3)
This was a double blinded RCT of 116 patients with uncomplicated corneal abrasions as a result of either mechanical trauma, UV exposure, or FB removal.
Exclusion criteria:
- >36 hrs post injury,
- previous eye surgery or cataracts,
- contact lens wearers,
- injured both eyes,
- ocular infection,
- grossly contaminated FB in eye,
- injury requiring urgent opthalmological evaluation (i.e. penetrating eye injury, large or complicated abrasions, significant disruption of vision).
Patients were randomized into two groups
1) topical tetracaine (1%) or
2) placebo – topical saline
Patients were instructed to use the eye drops every 30 minutes for up to 24 hours as needed. Patients also received acetaminophen 1g Q6H and chloramphenicol drops.
Primary safety outcome: Repeat ED exam at 48h, telephone follow up at 7d and 1 month monitoring for complications.
Secondary outcomes: pain score and patient’s perceived effectiveness.
Results showed that topical tetracaine was safe with no reported complications. Note that the study was not powered appropriately, allowing for up to 6% chance of complications. There was no significant difference in pain scores between the groups. Tetracaine was rated significantly higher for effectiveness by the patients.
Interestingly, whether the patients were randomized to the treatment arm or the placebo arm, the time to resolution of pain symptoms was similarly short (within 12 hours).
Take home message: consider topical tetracaine eye drops for patients with small abrasions (be selective), use for a short duration of time 6-12 hours.
Dr. Yaphe’s editorial:
There is no good evidence for any benefit for the use of anti-inflammatory or antibiotic topical eye drops in the management uncomplicated corneal abraisons. So presently, looking at the body of evidence, consider only giving a short course of tetracaine in these patients.
Update 2015: For our Journal Jam podcast with Salim Rezaie on a systematic review of topical anesthetics for corneal abraison go here.
PEITHO Study: Fibrinolysis for Patients with Intermediate Risk Pulmonary Embolism (4)
This was an RCT that included 1006 patients > 18 years of age with a confirmed PE, with symptoms 15 days or less prior to randomization. Patients also had evidence of myocardial injury (elevated troponin) and RV dysfunction (on ECHO or CT).
Patients with BP > 180/110 were excluded from the study.
Randomization of patients into two groups
1) full dose tenecteplase, or
2) placebo
Both groups received unfractionated heparin.
Primary outcome: death or hemodynamic decompensation within 7 days.
Secondary outcomes: major bleeding
There was a lower death/hemodynamic decompensation rate in the lysed patients (2.6% vs 5.6%), with most of the difference in hemodynamic decompensation, not death.
However, the Number needed to harm (NNH) was 14 for hemorrhagic stroke/major extracranial bleed!
Take home message: Save thrombolysis for unstable patients (i.e. patients in shock). Patients with elevated Troponin and signs of RV dysfunction on imaging who are not in shock should be monitored carefully and providers should be prepared to give rescue treatment (IV thrombolysis or interventional methods) if the patient decompensates.
Co-trimoxazole and Sudden Death in Patients Receiving Inhibitors of Renin-Angiotensin System (5)
This was a retrospective database review of 1.6 million patients in Canada. Co-trimoxazole (Septra) had an increased risk of death in patients on ACEI or ARBS compared to other antibiotics. The postulated mechanism was secondary to hyperkalemia.
Take home message: Avoid use of Septra in patients on ACEI or ARBs. If Septra is required, check the patient’s serum potassium before administering the drug.
The “Syringe” Technique: A Hands-free Approach for the Reduction of Acute Nontraumatic Temporomandibular Dislocations in the Emergency Department (6)
This was a prospective convenience sample of 31 patients aged 18-65 over 3 years in two hospital EDs.
The syringe technique:
- The patient bites down with their posterior molar teeth on a 5-10 cc syringe on the side of the dislocation.
- The syringe is rotated so that it pushes the posterior molars posteriorly. The direction of rotation is clockwise for a right dislocation, or counterclockwise for the left (see Fig 5).
Results: 30 of 31 patients successfully reduced with this method, the majority within 2 minutes.
Take home message: The syringe technique is a non-invasive, safe option for reduction of TMJ dislocation that avoids the need for procedural sedation.
Syringe Technique to Reduce TMJ Dislocation
Chronic Effects of Shift Work on Cognition: Findings from the VISAT Longitudinal Study (7)
This was a prospective cohort study of 3232 employed and retired workers. Various measures of cognition were taken at 0, 5, and 10 years. Workers were classified into two groups 1) shift work either current or past, or 2) never participated in any shift work.
Exposure to shift work was associated with a chronic impairment of cognition. This was highly significant if shift work was performed for more than 10 years.
Recovery of cognitive functioning back to baseline after having stopped any form of shift work took approximately 5 years.
Key References
[wptabs type=”accordion” style=”ui-lightness” effect=”slide” mode=”vertical”][wpspoiler name=”Click Here to View”] [wptabcontent]
1. Traub SJ, Kellum JA, Tang A, Catalado L, Kancharia A & Shaprio NI. Risk factors for radiocontrast nephropathy after emergency department contrast-enhanced computerized tomography. 2013. Acad Emerg Med, 2013, 20(1): 40-45. Abstract
2. Holst LB, Haase N, Wetterslev J, Wernerman J, Guttornsen AB, Karlsson S et al. Lower versus higher hemoglobin threshold for transfusion in septic shock. NEJM, 2014, 371: 1381-1391. Abstract
3. Waldman N, Denise IK & Herbison P. Topical tetracaine used for 23 hours is safe and rated highly effective by patients for the treatment of pain caused by corneal abrasions: A double-blind, randomized clinical trial. Acad Emerg Med, 2014, 21(4), 374-82. Abstract
4. Meyer G, Vicaut E, Danays T, Agnelli G, Becanttini, C, Beyer-Westerndorf J et al. Fibrinolysis for patients with intermediate-risk pulmonary embolism. NEJM, 2014, 370(15): 1402-11. Abstract
5. Fralick M, Macdonald EM, Gomes T, Antoniou T, Hollands S, Mamdani MM & Juurlink DN. Co-trimoxazole and Sudden Death in Patients Receiving Inhibitors of Renin-Angiotensin System. BMJ, 2014, 349: g6169. Full PDF
6. Gorchynski J, Karabidian E & Sanchez M. The “Syringe” technique: A hands-free approach for the reduction of acute nontraumatic temporomandibular dislocations in the emergency department. J Emerg Med, 2014, 47(6): 676-81. Abstract
7. Marquie JC, Tucker P, Folkar S, Gentil C & Ansiau A. Chronic effects of shift work on cognition: Findings from the VISAT longitudinal study. Occup Environ Med, 2014, 72(4): 258-64. Abstract
8. Thrombolysis for Pulmonary Embolism and Risk of all-cause mortality, major bleeding, and intracranial hemorrhage: a meta-analysis. Chaterjee S et al. JAMA 2014; 23:2414-21. Full PDF
[/wptabcontent][/wpspoiler] [/wptabs]
Dr. Helman, Dr. Hannam & Dr. Chopra have no conflicts of interest to declare








Hello Dr. Helman
I just wanted to thank you for doing an amazing job. I am an intern in Germany and I love your episodes. They are often practice changing for me and my superiors are very supreised with my knowledge :-) when we discuss different cases. Although I am working in cardiology right now there is unfortunately no emergency speciality here in Germany, So every specialty has to mange its own ed department which is confusing,
Anyway I really wanted to thank you please keep up doing this!!!!
Best regards from Germany
Max