Hemoptysis can be a hair-raising presentation to the ED. Stellar management of patients with massive hemoptysis requires understanding a few key principles and a flexible approach. In this podcast Anton is joined by EM and intensivist trained Dr. Bourke Tillmann and Dr. Scott Weingart to explore both an approach to life-threatening hemoptysis and one to hemoptysis that is not life-threatening. They answer questions such as: what are the factors to consider in the decision to intubate patients with massive hemoptysis? How can one reliably distinguish hemoptysis from pseudohemoptysis? What is the evidence for tranexamic acid in patients with hemoptysis? What are the best strategies for suctioning blood from the airway to improve visualization during endotracheal intubation in crashing hemoptysis patients? What is the role of bronchoscopy and how should it be integrated into the hemoptysis management algorithm? How does one’s hemorrhage control strategy change when pulmonary embolism is the underlying diagnosis? and many more…
Podcast production, sound design & editing by Anton Helman;
voice editing by Braedon Paul
Written Summary and blog post by Alex Chan, edited by Anton Helman November, 2023
Cite this podcast as: Helman, A. Weingart, S. Tillmann, B. Hemoptysis – ED Approach and Management. Emergency Medicine Cases. November, 2023. https://emergencymedicinecases.com/hemoptysis. Accessed April 23, 2024
Hemoptysis key principles
- Patients are poor at identifying the source of bleeding expelled from the mouth and often confuse hemoptysis with an upper airway or GI source; it is imperative to differentiate hemoptysis from pseudohemoptysis
- Early diagnosis, usually by chest CT with contrast, is important in guiding management
- Source control of the bleeding, which is usually from bronchial arteries, is the ultimate goal in management, which usually requires early involvement of interventional radiology and/or thoracic surgery and/or respirology; call for help early
- Once the side of bleeding in the lungs is identified by either chest X-ray, CT or during mainstem bronchus intubation, patients should be positioned bleeding lung down in lateral decubitus to prevent contamination of the contralateral lung
- Hemorrhage control measures including consideration for nebulized tranexamic acid (TXA) should be employed as a bridge to definitive treatment/source control
- Death from hemoptysis is most often due to respiratory arrest, akin to drowning, rather than exsanguination, and management should be directed accordingly
- Patients are generally better at clearing blood from their lungs by coughing compared to suctioning and airway control measures, so keep the patient spontaneously breathing and coughing whenever feasible; definitive airway management should be considered carefully and only when the patient is no longer able to clear blood spontaneously
- The definition of massive hemoptysis is unclear; more importantly, life-threatening hemoptysis can be identified by signs of respiratory distress, airway obstruction or abnormal gas exchange
- Suctioning of blood with either a meconium aspirator or Ducanto suction catheter is recommended to allow for adequate visualization during endotracheal intubation; standard suction catheters such as Yankauer catheters may not be adequate
- Cricothyrotomy should be performed in situations where suction cannot keep up with the volume of blood in the airway (preventing visualization of the chords) and/or failed first attempt at RSI
EM Cases 5 step approach to hemoptysis
Step 1: Differentiate hemoptysis from pseudohemoptysis
Distinguishing hemoptysis from alternative sources of bleeding may be a challenge, as patients are able to accurately identify the source of the bleed only about 50% of the time.
The following table summarizes the key clinical findings that help differentiate hemoptysis from a GI bleed and upper airway bleed.

Clinical features to differentiate hemoptysis from GI bleed and upper airway bleed
Pearl: Nasopharyngoscopy can help rule out an upper airway source if unsure if the source of bleeding is from the lungs or nasopharynx.
Step 2: Is this massive/life-threatening hemoptysis?
The definition of massive hemoptysis is highly variable. The definition of massive hemoptysis by volume over time ranges from 100mL to 600mL over several hours. Clinicians are poor at estimating volume of expectorated blood.
A more practical definition of massive or life-threatening hemoptysis should take the following under consideration:
- Signs of respiratory distress, signs of airway obstruction or evidence of abnormal gas exchange
- Hemodynamic instability
Step 3: Early diagnosis guides management
Although the differential diagnosis of hemoptysis is broad, initial workup should be focused on 3 critical time-sensitive diagnoses that each require specific management:
- Tracheo-innominate fistula
- Aortobronchial fistula
- Pulmonary embolism
Once the 3 critical time-sensitive diagnoses have been addressed, the broader differential diagnosis should be considered.
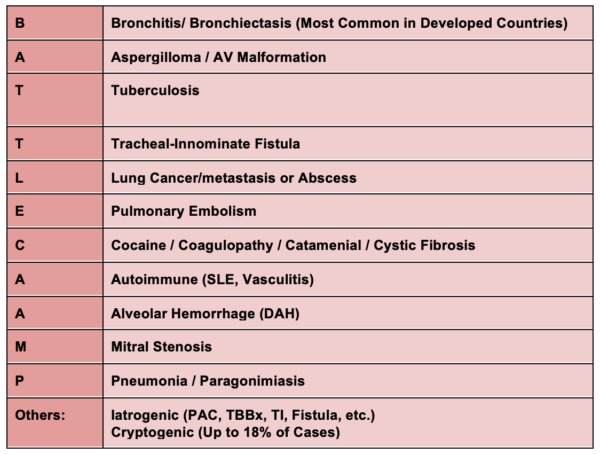
BATTLECAMP mnemonic for differential diagnosis of hemoptysis
CT chest with contrast should be the primary investigation modality to work up hemoptysis
A CT Chest with contrast in arterial phase should be our highest priority for workup of hemoptysis as it has a higher diagnostic yield than bronchoscopy and the diagnostic accuracy decreases with accumulation of blood in the lungs. The earlier the CT is done, the better, because as blood accumulates in the lungs, the accuracy of the CT in visualizing the source lesion decreases. Speak to your radiologist about the best contrast CT protocol for hemoptysis as some protocols are able to visualize both bronchial and pulmonary arteries.
The role of bronchoscopy in the work up and management of hemoptysis
Bronchoscopy can be complementary to CT and provide source control measures such as balloon tamponade with bronchial blockers, instillation of endobronchial epinephrine or endobronchial TXA. However, while bronchoscopy has similar efficacy in localizing the site of bleeding, its diagnostic accuracy is inferior to that of CT Chest and as such should not be used as a replacement for CT. Bronchoscopy should be considered an adjunct to be done following the CT scan in intubated patients. In some cases bronchoscopy may be the only option available for patients too unstable for transport to CT.
The role of chest X-ray in the work up and management of hemoptysis
A portable chest X-Ray may be useful to help localize the side of the bleeding in the minority of cases, but has poor diagnostic accuracy (up to 50% of patients with a normal chest X-ray will have contributory findings on CT) and should not be done acutely if it delays time-to-CT.
Pearl: At some hospitals, it may be possible to complete a CT scan with the patient in lateral decubitus position and the bleeding lung downward to avoid contamination of the contralateral lung; speak to your radiology department in advance to request this trick of the trade.
Step 4: Hemorrhage control measures prior to source control
It is important to understand that the primary cause of death in hemoptysis is respiratory, akin to drowning. However, addressing bleeding, similar to other life threatening hemorrhage should concurrently be address in the ED as a bridge to source control. The thrombotic risk associated with reversal of anticoagulants needs to be weighed against the risk of hemoptysis. Considerations for cessation of hemorrhage include:
- Reversal of anticoagulants with PCCs / direct reversal inhibitors
- Nebulized / IV TXA
- FFP if INR >2
- Cryoprecipitate/fibrinogen concentrate if fibrinogen <2 or suspected
- Replace platelets if <50 and consider DDAVP in uremic patients
- Red blood cells transfusion as necessary
Pitfall: A common pitfall is waiting until PE is ruled out before reversing any coagulopathy or administering TXA. In acutely life-threatening hemoptysis, always reverse any coagulopathy. Anticoagulation can be given later in the case of PE.
Episode 89 – DOACs Part 2: Bleeding and Reversal Agents
The role of TXA in hemoptysis
Although there is a relative scarcity of evidence for the use of TXA in hemoptysis, RCTs do suggest a benefit for inhaled/nebulized as well as IV TXA:
- Inhaled/Nebulized TXA 500-1000mg
- It is physiological sound to deliver the TXA directly to lungs via inhalation
- A small 2018 RCT found that patients receiving inhaled/nebulized TXA had greater resolution in first 5 days of admission compared to placebo for patients with non-massive hemoptysis
- Start with 500mg TID nebulized/inhaled, with consideration for 1g for massive hemoptysis as this dose has shown promising results in case reports
- IV TXA 1-2g
- RCTs demonstrate benefit in the management of non-massive TXA
- Although there is a lack of evidence in massive hemoptysis, it is the preferred route of administration in patients who cannot tolerate a nebulizer and/or cannot adequately clear blood from their airway
Our experts recommend nebulized TXA 1g for all hemoptysis patients with spontaneous respirations who do not have contraindications to TXA.
Step 5: Definitive management and source control will depend on the etiology
Definitive management commonly involves arterial embolization by interventional radiology as ~90% of hemoptysis originates from bronchial arteries. However, definitive management decision making is best made as a team with input from respirology and/or thoracic surgery and/or anesthesia and/or interventional radiology, depending on the underlying diagnosis and local resources.
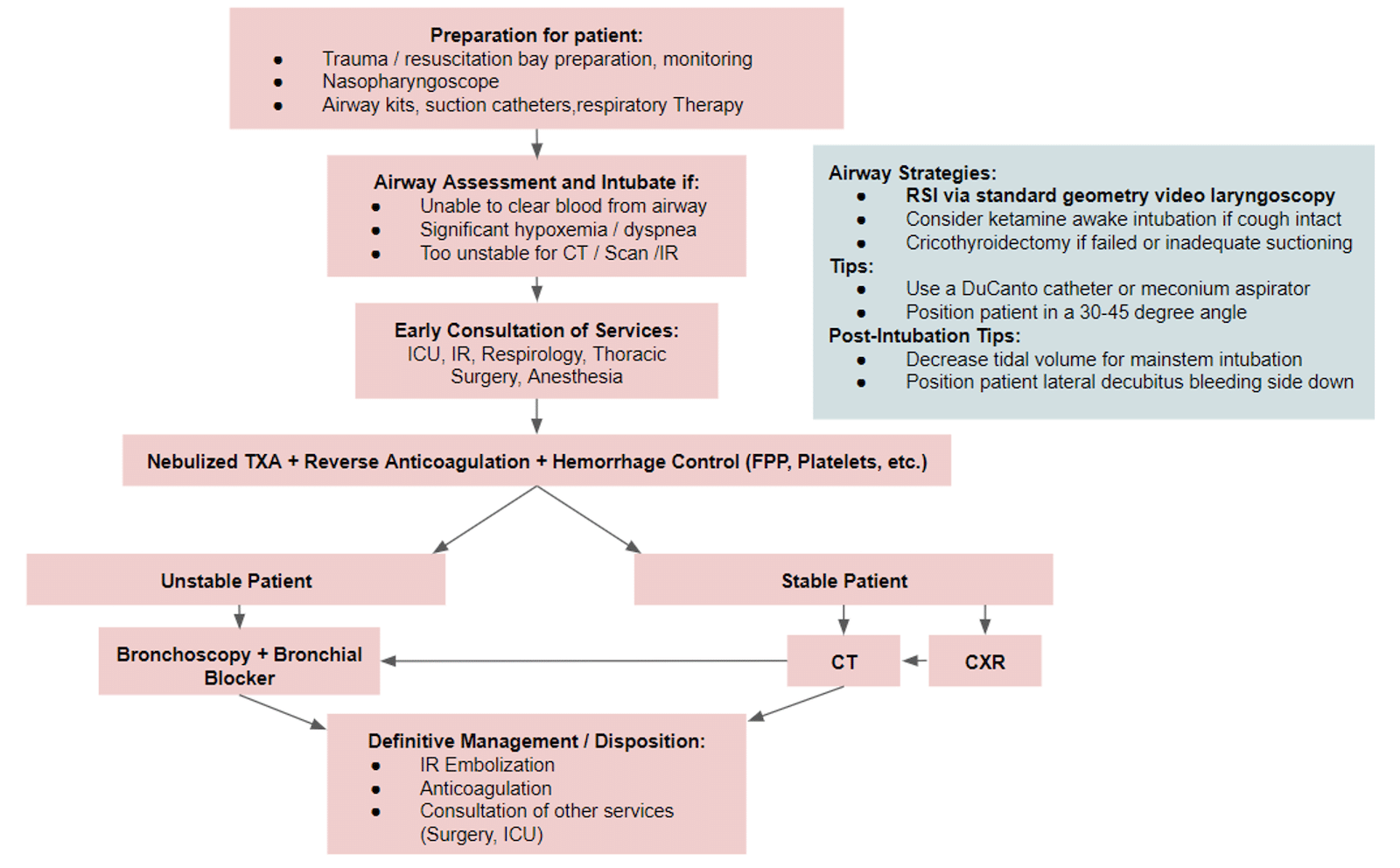
EM Cases approach to massive hemoptysis and management algorithm
There are a few key principles for life-threatening hemoptysis to optimize management:
- About 90% of hemoptysis originates from bronchial arteries under pressure, so bleeding may be brisk and source control is of utmost importance
- Source control can be achieved through a variety of measures depending on the underlying diagnosis, including embolization via interventional radiology, surgery via thoracics, bronchial blocker via respirology or anesthesia; call a friend early
- Patients are generally better at clearing blood from their airway by coughing than we are by suctioning, so maintaining spontaneous respirations is usually preferred over endotracheal intubation whenever possible
- Suctioning should be done via Ducanto catheter or meconium aspirator and if suctioning is overwhelmed by bleeding and first attempt at RSI fails, front of neck access/cricothyrotomy should be performed
Hypoxic respiratory arrest, not exsanguination, is the cause of death in massive hemoptysis
It is important to understand that patients with hemoptysis most often die from hypoxemia rather than exsanguination. Closely monitor the patient’s ability to clear out blood via coughing, and assist with suctioning when necessary. Patients who are able to cough out blood consistently are demonstrating strong respiratory effort, and will prevent blood accumulation better than our suctioning attempts.
Pitfall: A common pitfall is assuming that those patients who are coughing up small amounts of blood are not at risk of hypoxemia and respiratory failure. Patients with a weak cough/poor respiratory effort and hypoxia may be on the verge of respiratory failure as they are unable to prevent blood accumulation in the lungs.
EM Cases massive hemoptysis management algorithm
Airway management in massive hemoptysis
It is important to know that intubation can destabilize the patient, as it can result in increased blood accumulation in the lung(s). If intubation is deemed necessary to facilitate a future intervention or investigation, then the safest strategy is to delay intubation as long as possible.
Indications for endotracheal intubation for massive hemoptysis
- Tiring of respiratory effort/inability to clear secretions with coughing
- Signs of respiratory distress including frank hypoxemia and/or dyspnea
- Too unstable to allow safe transport to CT scan or interventional radiology
Endotracheal intubation via RSI and standard video laryngoscopy is the airway strategy of choice for patients with massive hemoptysis
Endotracheal intubation via RSI and standard geometry video laryngoscopy and bougie is our experts’ preferred method for securing the airway in massive hemoptysis. Use a large bore ETT (minimum 8-0) as this allows for placement of a bronchoscope.
Mainstem bronchus intubation for massive unilateral hemoptysis
Intubate the mainstem bronchus of the non-bleeding lung when blood fills the endotracheal tube who’s tip is in the trachea. The right mainstem bronchus is usually preferentially intubated when the ETT is advanced past the corina. If there is no blood appearing in the endotracheal tube, maintain and secure this ETT position. If blood does appear in the ETT, pull back the ETT into the trachea, advance a bougie through the ETT and orient it to the left by pointing the coude tip to the up to the ceiling, rotating it 90 degrees counterclockwise and advancing into the left mainstem bronchus. This may take several attempts.
Ketamine-facilitated awake intubation as an alternative to RSI in massive hemoptysis
Ketamine-facilitated awake intubation can be considered in the patient with an intact cough reflex and adequate respiratory effort. Topicalized awake intubation with lidocaine should not be used as it will likely be ineffective due to the volume of blood expulsion, or result in elimination of the cough reflex.
Patient positioning in massive hemoptysis
Patients should be intubated in a standard position at a 30-45-degree angle to optimize first-pass success and minimize blood entering the upper airway. Once intubated, place them in a lateral decubitus position with the bleeding lung down (as determined by chest X-ray, CT or during mainstem intubation)
Pitfall: A common pitfall is using standard ETT sizes and failing to select a large enough (minimum 8-0) bore ETT, as this will make bronchoscopy impossible.
Adequate suctioning is critical in the successful intubation of a patient with massive hemoptysis
Our experts recommend the DuCanto suction catheter as the preferred tool for large volume suctioning via the SALAD technique as it allows simultaneous suction during exploration with a laryngoscope to and identify the vocal cords, followed by immediate intubation with a bougie.
|
DuCanto suction-assisted laryngoscopy airway decontamination approach to managing massive hemoptysis |
|
DuCanto MSSM SALAD instruction video
If the DuCanto catheter is unavailable, a meconium aspirator attached to the ETT can be used effectively. The aspirator can be attached to the ETT to allow for simultaneous suctioning during intubation. Alternatively, a second provider can advance the meconium aspirator past your video laryngoscope to protect the video during intubation to achieve similar results.

Meconium aspirator attached to ETT
Standard ED suction catheters such as the Yankauer suction catheter may not provide you with enough suctioning volume for patients with massive hemoptysis.
Indications for cricothyrotomy in massive hemoptysis
If the ability to suction is overwhelmed by the volume of blood in the airway, intubation will not be possible. A supraglottic airway, followed by front of neck access/cricothyrotomy should be performed immediately.
Cricothyrotomy Master Class from EM Cases Summit
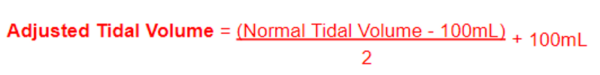
Ventilatory settings for massive hemoptysis
A good rule of thumb to calculate your adjusted tidal volume following mainstem intubation:
References
- AAFP. (2022). Hemoptysis: Evaluation and Management. American Family Physician.
- Alberto-Pasco. (2013). Association of TXA to mortality and bood transfusion among patients with hemoptysis at Hipolito Unanue Hospital of Lima. Revosta peruana de medicina experimental y salud publica, 357-358.
- Atchinson, R. (2021). The emergency department evaluation and management of massive hemoptysis. American Journal of Emergency Medicine.
- Bair. (2004). An evaluation of a blind rotational technique for selective mainstem intubation. Academy of Emergency Medicine, 1105-1107.
- Bellam. (2016). Efficacy of TXA in hemoptysis: a RCT pilot study. Pulmonary Pharmacological Therapeutics, 80-83.
- Brown, C. (2023). Hemoptysis. In Rosen’s Emergency Medicine: Concepts and Clinical Practice 10th Edition (pp. 189-193).
- Chang, J. (2023). TXA in the Treatment Paradigm for Hemoptysis. Chest.
- Charya, A. (2021). Management of life-threatening hemoptysis in the ICU. Journal of Thoracic Disease.
- Cutshall. (2022). Treatment of massive hemoptysis with repeated doses of nebulized TXA. Cureus.
- Davidson, K. (2019). Managing Massive Hemoptysis. Chest.
- Dempsey. (2020). Inhaled Tranexamic Acid for Massive Hemoptysis in the Setting of Oral
- Anticoagulation: A Case Report. Clinical Practice Cases in Emergency Medicine, 572-575.
- Dempsey, J. (2020). Inhaled TXA for Massive Hemoptysis in the setting of oral anticoagulation: case report. Clinical Practice and Cases in Emergency Medicine, 572-576.
- Farkas, J. (2021). Severe Hemoptysis. Retrieved from Internet Book of Critical Care: https://emcrit.org/ibcc/hemoptysis/
- Gopinath, B. (2023). Nebulized vs IV TXA in Hemoptysis: A Pilot Randomized Controlled Trial . Chest.
- Hankerson. (2015). Nebulized Tranexamic Acid as a Noninvasive Therapy for Cancer-Releated Hemoptysis. Journal of Palliative Medicine.
- Kinoshita. (2019). Effect of TXA on mortality in patients with hemoptysis: a nationwide study. Critical Care.
- Komura. (2018). Hemoptysis? Try TXA. Journal of Emergency Medicine, 97-99.
- Koppen, L. (2020). What literature is available for TXA in hemoptysis. Retrieved from University of Illinois Chicago: https://dig.pharmacy.uic.edu/faqs/2020-2/march-2020-faqs/what-literature-is- available-for-the-use-of-inhaled-tranexamic-acid-in-hemoptysis/
- Lee, Y. (2012). The clinical implications of bronchoscopy in hemoptysis patients with no explainable lesions in computed tomography. Respirology Medicine, 413-419.
- Lombardo. (2022). Evaluation of inhaled TXA for hemoptysis. Society of Critical Care Medicine Conference , 382.
- Lordan. (2003). The pulmonary physician in critical care – illustrative case 7: assessment and management of massive hemoptysis. Thorax, 814-819.
- Mansoor, A. (2018). Hemoptysis. In Frameworks for Internal Medicine (pp. 603-611).
- Mazi. (2022). TXA use for massive hemoptysis in a child: a case report. Cureus.
- Modi. (2019). Inhaled TXA in vasculitis-induced massive hemoptysis. Chest.
- Modi, R. (2019). Inhaled TXA in Vasculitis-Induced Massive Hemoptysis. Chest Annual Meeting 2019 – Abstract.
- Mondoni, M. (2018). Bronchoscopy in Patients with Hemoptysis and Negative Imaging Tests. Chest.
- Morgenstern, J. (2015). Massive Hemoptysis. Retrieved from First10EM: https://first10em.com/massive-hemoptysis/
- Murphy, D. (2020). The value of a bronchoscopy in patients with non-massive hemoptysis and a clear or benign CT scan. Clinical Respirology Journal, 430-436.
- Mahony, A. (2022). Meta-Analysis on the Utility of Bronchoscopy in Addition to CT Thorax in the
- Investigation of Lung Cancer in patients with hemoptysis. Respiration, 1139-1147.
- Neil. (2020). Inhaled TXA as a novel treatment for pulmonary hemorrhage in critically ill pediatric patients: an observational study. Critical Care Explorations.
- Petersen, L. (2020). Hemoptysis with no malignancy suspected on CT rarely requires bronchoscopy. European Clinical Respiratory Journal.
- Rezaie, S. (2018). TXA for Everyone: Inhaled TXA for Hemoptysis. Retrieved from RebelEM: https://rebelem.com/txa-for-everyone-inhaled-txa-for-hemoptysis/
- Ruiz. (1994). Acido tranexamico vs placebo en hemoptisis por TBC pulmonar: estudio pilato double ciego. PhD Thesis.
- Sanghvi. (2019). Tranexamic acid for treatment of pulmonary hemorrhage after tissue. American Journal of Emergency Medicine.
- Sims, T. (2020). Hemoptysis. In Tintinalli’s Emergency Medicine: A Comprehensive Guide 9th Edition. 432-436.
- Thirumaran, M. (2009). Is investigation of patients with haemoptysis and normal chest radiograph justified? Thorax, 854-856.
- Tscheikuna. (2002). TXA in patients with hemoptysis. Journal of the Medical Association of Thailand, 399-404.
- Tscheikuna, J. (2002). Transexamic acid in patients with hemoptysis. Journal of the Medical Association of Thailand, 399-404.
- Vallabh. (2022). Efficacy of nebulized TXA for severe hemoptysis at a tertiary academic medical centre.Society of Critical Care Medicine Conference, 461.
- Wand. (2018). Inhaled TXA for Hemoptysis Treatment: A RCT. Chest.
- Weingart, S. (2011). A novel set-up to allow suctioning during direct endotracheal and fiberoptic intubation. Retrieved from EMCrit: https://emcrit.org/emcrit/ett-as-suction-device/
- Weingart, S. (2017). A Wee Bit More on Massive Hemoptysis. Retrieved from EMCrit: https://emcrit.org/emcrit/wee-massive-hemoptysis/
- Weingart, S. (2017). Having a Vomit SALAD with Dr. Jim DuCanto – Airway Management Techniques during Massive Regurgitation, Emesis, or Bleeding. Retrieved from EMCrit: https://emcrit.org/emcrit/having-a-vomit-salad-with-ducanto/
- Weingart, S. (2017). Management of Massive Hemoptysis. Retrieved from EMCrit: https://emcrit.org/emcrit/massive-hemoptysis/
Drs. Helman, Weingart and Tillmann have no conflicts of interest to declare
Now test your knowledge with a quiz.





My first night shift alone as a new grad ped’s BMT nurse (>20 yrs ago) was with brand new BMT rotation MD and 8 y/o maybe day +5 post transplant (no counts) had alveolar hemorrhage 2* chemo. on our unit all rooms PICU equipped. Spitting started 2 day prior, sats dropping, spit more frequently more volume, nonstop products (plt <5) cryo? Factors? Kitchen sink nebs? Spit/suctioned out all products putting in. No sleep cos cough & sats drop. Was a helpful child patient. Intubated during dx scope start on next shift. Felt like in war trenches with that new MD.
Doctor, thank you for a great podcast and fir sharing your wisdom.
I am questioning if ventilation with CPAP or PEEP could, as well as improving oxygenation, help stem the bleeding until definite measures are taken? The literature is scant on this question.