Episode 12 Part 1: ACLS Guidelines – What’s New & Controversial
In Part 1 of this episode on the latest ACLS Guidelines, Dr. Steven Brooks and Dr. Michael Feldman review and debate what's new and what's controversial in the the 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Within the frameworks of Cardiocerebral Rescusitation and the 3 phase model of rescucitation (electrical, circulatory and metabolic), they discuss the importance of high quality CPR, the de-emphasis on early ventilation and the utility of continuous quantitative waveform capnography. Dr. Brooks and Dr. Feldman answer questions such as: of all the therapeutic manoeuvres we do for the cardiac arrest patient, which ones have been shown to improve survival to hospital discharge? What is the evidence for chest compression machines? What is the utility of bedside ultrasound in the cardiac arrest patient? Why is cardiac arrest survival to discharge in Seattle the best in the world? Should we be performing 'hands-on defibrillation'? and many more.....
Episode 11: Cognitive Decision Making and Medical Error
In this episode on Cognitive Decision Making & Medical Error, Dr. Doug Sinclair, CMO of St. Michael's Hospital and Dr. Chris Hicks show us that, while the ED physician's knowledge base may play a small part in predicting medical error, more important might be how we understand and reflect upon our decision-making processes, how we communicate with our staff and patients, and how we cope with the ED environment and shift work. Medical error is the 6th leading cause of death in North America, and despite huge advances in imaging technology and lab testing as well as an explosion of EM literature in recent years, the misdiagnosis rate detected through autopsy studies has not changed significantly over the past century. Studies on diagnostic error in emergency medicine have shown error rates between 1 and 12%, and it's been suggested that cognitive error, or some flaw in the decision making process (as apposed to a lack of knowledge), is present in about 95% of these cases. Dr. Sinclair and Dr. Hicks elucidate for us how to identify and understand cognitive decision making and medical error, and how we can improve our decision making, reduce medical error and optimize the care of our patients.
Episode 10 Part 2: Trauma Pearls and Pitfalls
In Part 2 of this episode on Trauma Pearls & Pitfalls Dr. Dave MacKinnon and Dr. Mike Brzozowski go through key management strategies and controversies surrounding head, neck, chest, abdominal, pelvic and extremity trauma, followed by a discussion on how best to prepare the trauma patient for transfer to a trauma centre.
Episode 10 Part 1: Trauma Pearls and Pitfalls
In this episode on Trauma Pearls and Pitfalls, Dr. Dave MacKinnon and Dr. Mike Brzozowski discuss the latest in trauma controversies. In Part 1 they give us some key pearls and pitfalls on traumaairway management, the value of the C-spine collar, how to clear the C-spine, vascular access options in trauma, 'Damage Control Rescuscitation', the best resuscitation fluids to use including hypertonic saline, hemostatic drugs such as Tranexamic Acid in trauma, the vulue, or lack thereof, of Recombinant Factor 7a in trauma, and the use of Prothrombin Complex Concentrates in trauma.
Episode 9: Nontraumatic Eye Emergencies
Nontraumatic Eye Emergencies are seldom very satisfying for the emergency physician to manage. However, with systematic approach and timely management they can save a patient's vision. Dr. George Porfiris and Dr. Simon Kingsley discuss four non-traumatic eye emergency presentations. The painful red eye, the painless red eye, acute painful loss of vision and acute painless loss of vision. Several cases are discussed in which an accurate diagnosis and timely ED management are of critical importance in order to prevent permanent vision loss and significant morbidity. A systematic approach to the eye examination is described with particular attention to important maneuvers such as the swinging flashlight test. The utility of ED ultrasound of the eye is debated, and a discussion around systemic diseases that cause eye problems provides fodder for many clinical pearls.
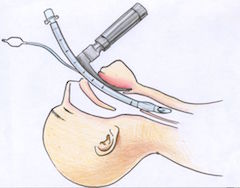
Episode 8: Emergency Airway Controversies
There are so many emergency airway controversies in emergency medicine! Dr. Jonathan Sherbino, Dr. Andrew Healy and Dr. Mark Mensour debate dozens of these controversies surrounding emergency airway management. A case of a patient presenting with decreased level of awareness provides the basis for a review of the importance, indications for, and best technique of bag-valve-mask (BVM) ventilation, as well as a discussion of how best to oxygenate patients. This is followed by a discussion of what factors to consider in deciding when to intubate and some of the myths of when to intubate. The next case, of a patient with severe head injury who presents with a seizure, is the fodder for a detailed discussion of Rapid Sequence Intubation (RSI). Tips on preparation, pre-oxygenation and positioning are discussed, and some great debates over pre-treatment medications, induction agents and paralytic agents ensues. The new concept of Delayed Sequence Intubation is explained and critiqued. They review how to identify a difficult airway, how best to confirm tube placement and how to avoid post-intubation hypotension. In the last case of a morbidly obese asthmatic they debate the merits of awake intubation vs RSI vs sedation alone in a difficult airway situation and explain the best strategies of ventilation to avoid the dreaded bradysystlolic arrest in the pre-code asthmatic. Finally, some key strategies to help manage the morbidly obese patient's airway effectively are reviewed.