Nontraumatic Eye Emergencies are seldom very satisfying for the emergency physician to manage. However, with systematic approach and timely management they can save a patient’s vision. Dr. George Porfiris and Dr. Simon Kingsley discuss four non-traumatic eye emergency presentations. The painful red eye, the painless red eye, acute painful loss of vision and acute painless loss of vision. Several cases are discussed in which an accurate diagnosis and timely ED management are of critical importance in order to prevent permanent vision loss and significant morbidity. A systematic approach to the eye examination is described with particular attention to important maneuvers such as the swinging flashlight test. The utility of ED ultrasound of the eye is debated, and a discussion around systemic diseases that cause eye problems provides fodder for many clinical pearls.
Written Summary and blog post by Lucas Chartier, edited by Anton Helman November 2010
Cite this podcast as: Porfiris, G, Kingsley, S, Helman, A. Nontraumatic Eye Emergencies. Emergency Medicine Cases. November, 2010. https://emergencymedicinecases.com/episode-9-nontraumatic-eye-emergencies/. Accessed [date].
In this episode, Dr. Porfiris and Dr. Kingsley provide answers to questions such as: When is it okay for EM physicians to be using topical steroids for eye emergencies? How can one distinguish conjunctivitis from Episcleritis and Scleritis? Which systemic diseases do we need to know about that present with eye complaints? What is the best emergency management of acute painless loss of vision due to central retinal artery occlusion? What is the evidence for thrombolysis of central retinal artery occlusion? What is the role of ED ultrasound in non-traumatic eye emergencies? What is the sensitivity of ESR for temporal arteritis? What is the roll of Doppler ultrasound in the diagnosis of temporal arteritis? How is temporal arteritis with ocular manifestations treated differently to temporal arteritis without ocular manifestations? What is the role of MRI in the diagnosis and management of optic neuritis? What is the evidence for IV steroid therapy in optic neuritis? What funduscopic finding is pathagnomonic of subarachnoid hemorrhage?
APPROACH TO THE RED EYE
Characterization of a patient’s eye pain helps determine the location of the pathology:
-
-
- Up‐front, scratchy, ‘sand‐in‐the‐eye’ pain relates to anterior structures such as the lids, conjunctivae, cornea, and foreign bodies;
- Deep, boring, ‘behind‐the‐eye’ toothache pressure‐type pain relates to posterior structures;
- Photophobia relates to uveal tract pathology such as iris, ciliary body and choroid
-
Systematic eye exam for every patient with an eye complaint: 6 parts ‐ visual acuity (the ‘6th vital sign’), visual fields by confrontation, size and reactivity of pupil, extraocular movements (for cranial nerve palsies), anterior segment (slit‐lamp exam) and posterior segment (fundoscopy)
The painful red eye
Acute angle‐closure glaucoma
Characterized by at least 2 of the following symptoms – acute onset ocular pain with nausea vomiting, intermittent blurring of vision with halos seen around lights (due to corneal edema), photophobia, and visual loss – along WITH at least 3 of the following signs – intraocular pressure (IOP) >21 mmHg (often 40‐80 mmHg), conjunctival injection, corneal epithelial edema causing haziness, fixed and mid‐dilated pupil, and shallow anterior chamber (on oblique flashlight test with shadow medial to pupil caused by the bulging anterior chamber when the light is flashed from the patient’s temporal side)
- Risk factors include elderly patients who are far‐sighted (hyperopic), and triggers include transition from light to dark environment (causing mydriasis) as well as many medications – anticholinergic, antimuscarinic, antidepressant, antipsychotic, antihistaminic, and sympathomimetics (most of them through mydriasis)
- ED management (re‐assess IOP q15min in the early phases of treatment):
- Topical beta‐blocker (e.g. 1 drop of Timolol 0.25‐0.5%) to decrease aqueous humour production if no contraindications present (COPD, asthma, bradycardia)
- Topical cholinergic (1‐2 drops of Pilocarpine q15min x2 doses) to cause myosis, decrease angle of the anterior chamber at the trabecular meshwork level, and increase drainage
- Parenteral agents: Acetazolaminde 500mg IV (or PO) to decrease aqueous humour production, and add Mannitol 1.25‐2g/kg IV of 20% solution to exert an osmotic diuresis if a response with other drugs does not occur
- When is acute angle‐closure glaucoma missed?
-
- Elderly, disabilities, dementia, psychiatric pts where a thorough history and physical may be challenging
- Pts who present primarily with headache or abdo pain and vomiting
-
- Consider acute angle‐closure glaucoma in any pt who has had recent eye surgery
Anterior uveitis or iritis
- Symptoms – deep, aching pain radiating to periorbital or temporal area, worse with eye movements and accommodation, and with PHOTOPHOBIA (very important)
- Signs – ciliary flush (erythema that is worse closer to the iris, and not in the periphery as in conjunctivitis), pain relief with cyclolegics but not with topical anesthetics, and consensual photophobia (light in the unaffected eye, because it causes bilateral myosis, causes pain), and abnormal slit lamp exam with keratitic precipitates or hypopyon, and cells and flare in the anterior chamber, which scintillate for milliseconds at a time like ‘snowflakes in the car’s headlights’ when driving at night under an oblique slit lamp light
- Important diagnosis to make in order to prevent long‐term vision loss consequences due to scarring, malfunction in the shape of the iris, and the increased likelihood of retinal detachment, and also to screen for the 50% of cases that have underlying infectious or autoimmune diseases such as herpes, tuberculosis, syphilis, toxoplasmosis, as well as the seronegative spondyloarthropathies – inflammatory bowel disease, ankylosing spondylitis, reactive arthritis, psoriatic arthritis; also Behçet, rheumatoid arthritis, SLE, sarcoidosis, and scleroderma
- ED management:
- Cycloplegic drops to prevent myosis, which acts as both pain control and breaking up of the synechiae caused around the iris – Homatropine (1 drop TID of 2‐5% solution) lasts a few days and is probably best, or:
- Cyclopentolate (1 drop TID of 0.5‐2% solution), which lasts 1 day; Mydriacyl, which lasts only 2‐3hrs, is good for diagnosis but not for treatment
- Steroids should only be used in conjunction with ophthalmologist consultation due to the concern for worsening of underlying infection or development of corneal ulcer, both of which may lead to loss of vision
- Ophthalmological follow‐up within 24hrs
The painless red eye
Kawasaki disease
- Acute systemic vasculitis of mucosal vessels of unknown etiology in children mnemonic Warm C‐R‐E‐A‐M
- Warm ‐ Fever >39°C for 5 days, PLUS 4 of the 5 following signs (or less in ‘atypical’ form of the disease):
- C ‐ Conjunctivitis, bilateral non‐exudative
- R ‐ Rash, polymorphic (e.g. urticarial, maculopapular) and on the body (not vesicular nor bullous)
- E – Edema or erythema of the hands, eventually leading to desquamation
- A ‐ Adenopathy with at least one anterior cervical lymph node >1.5cm (not generalized over the whole body)
- M – Mucosal involvement: fissured red lips, strawberry tongue
- Incomplete Kawasaki: American Guidelines ‐ “If the typical clinical findings of Kawasaki disease are present in a child with fever for less than five days, or if three classic features plus coronoary artery findings on echocardiography are found, the diagnosis still can be made and treatment initiated”
- Features that go against the diagnosis of Kawasaki: exudative conjunctivitis or pharyngitis, discrete intra‐oral lesions, bullous or vesicular rash and generalized lymphadenopathy
- Pearls: almost always look unwell/very irritable, fever is minimally responsive to anitpyretics, often have peri‐anal erythema, and there is often a sharp demarcation at the wrist and ankles from the redness in the extremities
- Abnormal tests – High platelets, WBC, ESR and CRP, LFTs (especially AST/ALT), sterile pyuria in urine (WBC present but no bacteria), as well as normochromic, normocytic anemia and hyponatremia
- Treatment – High dose ASA and IVIG, best if treat within 10d of onset of symptoms (lower complication rate)
APPROACH TO LOSS OF VISION
Painless loss of vision
- Ddx of painless acute visual loss not related to trauma
- vascular occlusion, retinal detachment, vitreous hemorrhage, macular disorders, neuro‐ophthalmologic disease, hysteria, and secondary to methanol or viagra
- Pearls – loss of vision over seconds is usually due to a vascular etiology, such as ischemia of the retina; posterior vitreous detachment will often cause debris to obstruct the light but the patient can see through it, vs. retinal detachment whereby there is a frank field deficit
Temporal arteritis:
- Vasculitis of autoimmune etiology affecting the arterial branches of the internal carotid artery (ophthalmic and temporal arteries) that is often preceded by features of polymyalgia rheumatica (PMR)
- Definition from the American College of Rheumatologists: age over 50, new headache, abnormality of the temporal artery (tenderness or pulselessness), ESR >50, and positive temporal artery biopsy; 3 out of 5 positive criteria result in a sensitivity of 93% for the diagnosis, and a specificity of 91%
- Symptoms – jaw claudication and diplopia are most predictive, but also temporal area pain and subacute peripheral vision loss, low grade fever, constitutional symptoms lasting weeks to months (anorexia, fatigue, myalgias, night sweats, weight loss), ataxia, decreased hearing
- Signs – beading, prominence or tenderness of the temporal artery is the most predictive, but also temporal scalp area tenderness, hyperesthesia and hypersensitivity, and vestibular or hearing impairment at time of presentation
- Think of temporal arteritis in elderly patients who present ‘Weak & Dizzy’ because often symptoms are vague
- ESR and CRP – Normal ESR values increase with age (age 2 for men, and [age + 10] 2 in women), and biopsy‐positive temporal artery cases with normal ESR vaules are not uncommon , but the combination of normal ESR and CRP has a sensitivity of 99% in ruling out the diagnosis
- Do not rely on on a normal ESR alone to rule out temporal arteritis
- Treatment – Steroids, with PO formulation if no ocular symptoms are present and IV if they are; do not delay treatment even if biopsy cannot be performed for a few days as earlier treatment has been shown to lead to better improvement (60% if treated within 24hrs of symptoms, vs. only 5% if treated after 24hrs)
Central Retinal Artery Occlusion (CRAO):
- Sudden abrupt painless vision loss (i.e. stroke of the retina, with the same car‐diovascular risk factors), either complete (with light‐dark perception only over the whole visual field), or with central vision retained (due to the different vas‐cular distribution of the fovea)
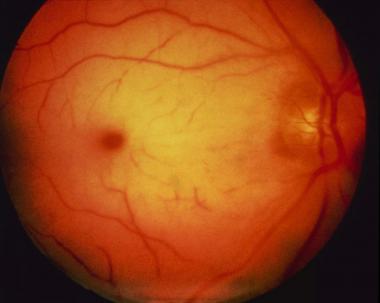
- Signs – Positive RAPD (rapid afferent pupillary defect) with a blanched, non‐perfused retina with the pathognomonic cherry‐red spot, i.e. the red fovea underlying the almost transparent retina, lateral to optic disk
- Management – Time‐sensitive goal to restore blood flow and remove obstruction through vigorous massage of eyeball to break the clot down and send it downstream to convert it to a branch occlusion, antiplatelet therapy (ASA), and decrease IOP (timolol, acetazolamide, and mannitol), possibly thrombolytics on a case‐by‐case basis, and breathing into a paper bag 10min each hour to increase the CO2 with resultant arterial vasodilation
Central Retinal Venous Occlusion (CRVO)
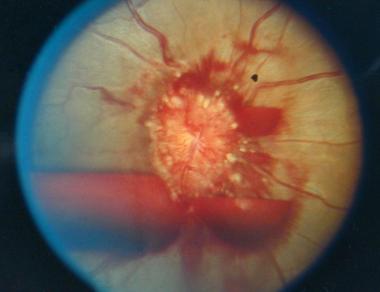
- “DVT of the eye”, vascular engorgement (gradual changes); tell‐tale – big angry stormy eye on fundcoscopic exam; hyperaemic, ‘blood and thunder’ exam
Painful loss of vision
Optic neuritis
- Inflammation of the optic nerve (due to demyelination), usually in women 15‐45, causing the classic triad of unilateral loss of vision, eye pain (especially with eye movement) and dyschromatopsia (washed out colors, especially red, as if looking through frosted glass)
- Signs – Markedly decreased visual acuity (often to light perception only), with a normal eye and funduscopic exam – “the patient sees nothing, and you see nothing on exam” (may sometimes see blurred disk margins and swollen veins), with positive RAPD (the pupils paradoxically dilate when the flashlight is swung from the unaffected to the affected eye due to the decreased light perception; also seen in vitreous hemorrhage, retinal detachment or ischemia, and retrobulbar hemorrhage); If plaques are seen on MRI, more likely to develop multiple sclerosis
- Treatment – The Optic Neuritis Treatment Trial showed that IV methylprednisolone 250mg qid x 3d followed by an oral prednisone taper over 1wk restores vision more quickly, and delays the development of multiple sclerosis by 2yrs
Pearls from the experts on Nontraumatic Eye Emergencies
Infectious conjunctivitis
- The most important part of management is irrigation and washing out of the eye
- Contact lens wearers should be prescribed anti‐pseudomonals such as Tobramycin (aminoglycoside), or Ciprofloxacin
- Suspect gonococcal infection with recent unprotected sexual intercourse, especially if there is substantial purulent discharge that re‐accumulates rapidly after wiping, or in infants 3‐6 days of life with red eyes after vaginal birth, which require admission and IV antibiotics
4 non‐traumatic eye emergencies that require prompt ophthalmological consultation:
- Acute angle‐closure glaucoma
- severe uveitis
- acute loss of vision (from CRAO, temporal arteritis, retinal detachment or optic neuritis)
- significant corneal ulceration of >1mm in length
Terson syndrome
- In subarachnoid hemorrhage (SAH), the sudden rise in intracranial pressure may lead to retinal veins rupture, resulting in a subhyloid hemorrhage with boat shape from central disk on fundoscopy (pathognomonic for SAH)
Dr. Helman, Dr. Simon and Dr. Porfiris have no conflicts of interest to declare.
Key References
Hockberger RS, Walls RM. Rosen’s Emergency Medicine – Concepts and Clinical Practice, 2-Volume Set,Expert Consult Premium Edition – Enhanced Online Features and Print,7, Rosen’s Emergency Medicine – Concepts and Clinical Practice, 2-Volume Set. Elsevier Health Sciences; 2009.
Tintinalli J, Stapczynski J, Ma OJ et al. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, Seventh Edition (Book and DVD). Mcgraw-hill; 2010.
Newburger JW, Takahashi M, Gerber MA, et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a statement for health professionals from the Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease, Council on Cardiovascular Disease in the Young, American Heart Association. Pediatrics. 2004;114(6):1708-33.
Volpe NJ. The optic neuritis treatment trial: a definitive answer and profound impact with unexpected results. Arch Ophthalmol. 2008;126(7):996-9.






Great podcast. Listening to it now, May 2016 and it was great. Never heard of Terson’s syndrome but great teaching point for me and my residents!!!