In this Part 1 or our two-part podcast series on STIs we discuss a general approach to cervicitis, vulvovaginitis and urethritis, elucidate some key historical features, debate who needs a pelvic exam in the ED, understand who needs what testing, debate self swabs vs physician taken swabs, dig into some specific under-recognized organisms like Mycoplasma Genitalium, figure out who needs what kind of empiric treatment, sexual partner treatment and which discharge instructions are key…
Podcast production, sound design & editing by Anton Helman
Written Summary and blog post by Hanna Jalali, edited by Anton Helman May, 2023
Cite this podcast as: Helman, A. Shafer, R. Varner, C. STIs: Vulvovaginitis, Cervicitis and Urethritis Emergency Recognition and Management. Emergency Medicine Cases. May, 2023. https://emergencymedicinecases.com/stis-cervicitis-vulvovaginitis-urethritis. Accessed April 23, 2024
Why should Emergency Medicine care about STIs?
STIs are on the rise with 20 million identified each year in the United States, and are under-recognized in the ED at least partly because only 30% of patients are symptomatic. While many STIs are relatively asymptomatic and/or relatively benign, certain STIs such as syphilis can have a mortality rate as high as 58%. Additionally, when recognized and treated early, ED physicians can prevent many of the long term sequelae of STIs such as Pelvic Inflammatory Disease and infertility. Many patients do not have access to primary care and the ED may be the only opportunity for screening, counseling and treatment of STIs.
General approach to cervicitis and vulvovaginitis
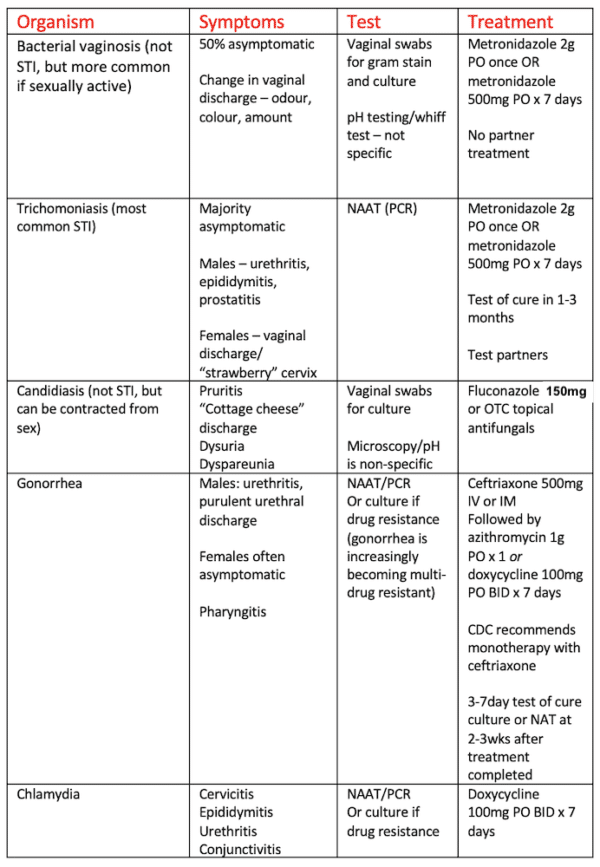
Common causes of vulvovaginitis include bacterial vaginosis, trichomoniasis, while cervicitis is commonly caused by chlamydia and gonorrhea. In the ED on first point of contact the organism is difficult to determine with certainty as no clinical feature or combination of features rules in any of these etiologies. Even with lab testing , the etiology will remain unknown in 83% of patients presenting with STI symptoms. Our approach needs to take this into consideration, especially when counseling patients.
History taking for suspected STI
- Make the patient comfortable: Consider a private setting/exuse visitors from the room, use understandable, non-judgemental language that normalizes questions, ask the patient if they would like a chaperone present
- Elicit symptoms of STIs: STI complaints may include abnormal vaginal or urethral discharge, lower pelvic pain, genital rash, painful/painless ulcer, dysuria, dyspareunia, throat pain, rectal pain or rectal discharge
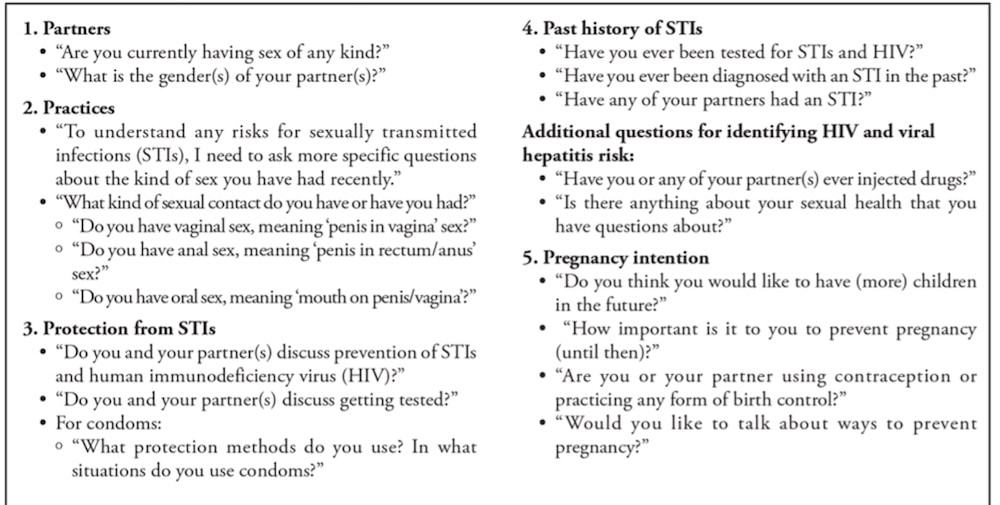
- Assess risk: There is the 5Ps approach to eliciting risk of STIs (see below) however, simply being sexually active in combination with any new symptoms of STI confers a high pretest probability
Are pelvic exams necessary for patients who present with symptoms suggestive of an STI?
Proponents of not performing a pelvic exam for females with symptoms suggestive of an STI site studies that suggest no change in management when pelvic exams are performed for assessment of adnexal mass or during first trimester bleeding to assess for ectopic pregnancy in the outpatient setting. No studies to date prove that pelvic exams have no impact on management in patients suspected of an STI in the ED setting. Our experts recommend pelvic exams for all females suspected of an STI as they can both identify concerning lesions such as ulcers that patient’s may not visualize/identify themselves and to help facilitate swabs to identify the specific etiology.
Indications for lab testing for STIs in the ED
Our experts recommend liberal testing for STIs because studies suggest that providers are poor at predicting STIs clinically, unidentified/untreated STIs may increase future risk of PID, PPROM, preterm birth, infertility, and small for gestational age birth, and because risks of testing are low. Having one STI should be considered a biomarker for having other STIs.
Indications for testing for STIs in the ED include:
- Symptoms of STI/risk factor(s) of STI (see above)
- Patient requests screening
- Pregnant people or considering pregnancy in the near future
Pitfall: A common pitfall is neglecting to test for other STIs such as syphilis, HIV and hepatitis in patients diagnosed with an STI. Having one STI should be considered a biomarker for for risk of other STIs.
Mycoplasma genitalium – an increasing cause of cervicitis/urethritis and PID
This is an organism that is often missed. Mycoplasma genitalium presents with symptoms of urethritis/cervicitis similarly to Gonorrhea and Chlamydia or may be asymptomatic.
Consider this organism in:
- Patients who have refractory urethritis, cervicitis or PID
- Patients with persistent symptoms of cervicitis/urethritis despite negative Gonorrhea/Chlamydia or recent treatments for Gonorrhea/Chlamydia
The test for Mycoplasma genitalium NAAT/PCR (culture available but takes 6 months)
Treatment depends on macrolide sensitivity:
- If macrolide sensitive: doxycycline 100mg PO BID x 7 days plus azithromycin 1g PO x 1 day then azithromycin 500mg PO x 3 days.
- If macrolide resistant: doxycycline 100mg PO BID x 7 days plus moxifloxacin 400mg PO OD x 7 days.
Summary of lab tests for ED patients suspected of vulvovaginitis/cervicitis/urethritis STI
- Gonorrhea and Chlamydia vaginal/cervical swabs testing (note that vaginal swabs have been shown to be as accurate as cervical swabs for Gonorrhea and Chlamydia and that swabs have been shown to be more accurate than urine testing in a 2023 meta-analysis)
- Gonorrhea C&S if drug resistant gonorrhea prevalent in local community
- Vaginal gram stain and culture (for Trichomoniasis and Bacterial vaginosis)
- Consider PCR swab for Mycoplasma geniatalium in patients with persistent cervicitis/PID/urethritis
- Strongly consider testing for HIV/Hepatitis/syphilis in anyone with a presumptive or confirmed diagnosis of STI
- Rectal/pharyngeal testing should be done in patients who have rectal/pharyngeal symptoms, men who have sex with men (MSM), sex workers (or those with contact), or those who have had sexual contact with confirmed case
Are self performed vaginal swabs as accurate as physician performed vaginal/cervical swabs for STIs?
There is evidence to suggest that there is no significant difference in diagnostic accuracy between self-performed vaginal swabs and physician performed cervical or vaginal swabs, so you can provide patients the option. However, this does not preclude the recommendation to perform a pelvic exam. Self-performed swabs should be reserved for those patients who refuse a pelvic exam or her prefer self-swabs.
Empiric treatment of cervicitis/urethritis
Empiric treatment of cervicitis/urethritis in the ED: Ceftriaxone 500mg IM/IV followed by doxycycline 100mg PO BID x 7 days.
(note the change in recommendation from 250mg ceftriaxone to 500mg due to increasing rates of drug-resistant Gonorrhea)
There is a balance between preventing long term sequelae of untreated STIs and preventing multi-drug resistance that has occurred with organisms like gonorrhea. The choice to treat empirically is patient specific however generally the benefits outweigh the risks of empiric treatment in:
- Patients with clinical high pretest probability of urethritis, cervicitis or vulvovaginitis
- Severe clinical condition
- Multiple risk factors for STI (sex work, unprotected sexual activity, travel)
- Poor access to follow-up after testing
- Age and potential for pregnancy/currently pregnant
It is important to engage in shared decision making with your patients and gauge their wishes regarding early treatment versus following up with primary care once results are available.
Discharge counseling for patients with suspected/confirmed STI
- For all STIs it is important to discuss sharing information with sexual partners and encourage that partners present to care and get treatment
- All partners with sexual contact with a patient 60 days prior to onset of symptoms or positive test should to be referred for evaluation
- Expedited partner treatment – in some jurisdictions prescriptions may be written for sexual parteners that are not directly assessed by the physician – find out the laws in your jurisdiction
- Involve your jurisdiction’s public health early, and report as per jurisdictions requirements; inform patients about these requirements
- Ask patients to abstain from sexual intercourse for 7 days while being treated with doxycycline or 7 days after one time dose of azithromycin/ceftriaxone
- Counsel on safe sex practices going forward
ED Quality Improvement
- Consider having discharge checklist for patients being discharged with suspicion for or diagnosis of STI as there are multiple counseling points that need to be considered.
- When testing for STIs in the ED, consider whether your department has a quality assurance program to reach patients with the results of their tests.
- Consider having testing/treatment kits that allow for efficient empiric testing and treatment.
- Have easy access to local jurisdiction Public Health policies available to providers to help with counseling and mandatory reporting.
References
-
- Ahmad, F. A., Fischer, K., Gu, H., Bailey, T. C., Jeffe, D. B., Carpenter, C. R., & Payne, P. R. O. (2022). Impact of risk-based sexually transmitted infection screening in the emergency department. Academic Emergency Medicine: Official Journal of the Society for Academic Emergency Medicine, 29(7), 879–889.
- (2021, July 22). STI Treatment Guidelines. Centers for Disease Control and Prevention. https://www.cdc.gov/std/treatment-guidelines/default.htm
- Chernesky, M. A., Jang, D., Portillo, E., Smieja, M., Gilchrist, J., Ewert, R., & MacRitchie, C. (2012). Self-collected swabs of the urinary meatus diagnose moreChlamydia trachomatis and Neisseria gonorrhoeaeinfections than first catch urine from men: Table 1. Sexually Transmitted Infections, 89(2), 102–104.
- Chlamydia, G. (2019). Bacterial STI Testing: Quick Reference. https://www.publichealthontario.ca/-/media/documents/B/2019/bacterial-sti-quick-reference.pdf
- Vaginal Swab vs Urine for Detection of Chlamydia trachomatis, Neisseria gonorrhoeae, and Trichomonas vaginalis: A Meta-Analysis. Ann Fam Med. 2023 Mar-Apr;21(2):172-179.
- Greenwald, A., Kelly, A., & Thomas, L. (2023). Trauma-informed care in the emergency department: concepts and recommendations for integrating practices into emergency medicine. Medical Education Online, 28(1).
- Hilbert, S. M., & Reno, H. E. L. (2018). Management of Patients with Sexually Transmitted Infections in the Emergency Department. Emergency Medicine Clinics of North America, 36(4), 767–776.
- Is it time to rethink your use of chaperones? (n.d.). CMPA. Retrieved May 7, 2023, from https://www.cmpa-acpm.ca/en/advice-publications/browse-articles/2019/is-it-time-to-rethink-your-use-of-chaperones
- KAMWENDO, F., FORSLIN, L., BODIN, L., & DANIELSSON, D. (1996). Decreasing Incidences of Gonorrhea- and Chlamydia-Associated Acute Pelvic Inflammatory Disease. Sexually Transmitted Diseases, 23(5), 384–391.
- Lunny, C., Taylor, D., Hoang, L., Wong, T., Gilbert, M., Lester, R., Krajden, M., & Ogilvie, G. (2015). Self-Collected versus Clinician-Collected Sampling for Chlamydia and Gonorrhea Screening: A Systemic Review and Meta-Analysis. PLOS ONE, 10(7), e0132776.
- Schoeman, S. A., Stewart, C. M. W., Booth, R. A., Smith, S. D., Wilcox, M. H., & Wilson, J. D. (2012). Assessment of best single sample for finding chlamydia in women with and without symptoms: a diagnostic test study. BMJ, 345(dec12 1), e8013–e8013.
- Sexton, M. E., Baker, J. J., Nakagawa, K., Li, Y., Perkins, R., Slack, R. S., Baker, D. C., Jucha, B., Arora, S., & Plankey, M. W. (2013). How reliable is self-testing for gonorrhea and chlamydia among men who have sex with men? The Journal of Family Practice, 62(2), 70–78. https://pubmed.ncbi.nlm.nih.gov/23405376/
- Stewart, C. M. W., Schoeman, S. A., Booth, R. A., Smith, S. D., Wilcox, M. H., & Wilson, J. D. (2012). Assessment of self taken swabs versus clinician taken swab cultures for diagnosing gonorrhoea in women: single centre, diagnostic accuracy study. BMJ, 345(dec12 1), e8107–e8107.
Drs. Helman, Shafer and Varner have no conflicts of interest to declare
Now test your knowledge with a quiz.





Leave A Comment