Written Summary and blog post written by Anton Helman, March 2016
This podcast was recorded live at The EM Cases Course
at North York General Hospital in Toronto February 2016
CASE 1: A 37 year-old otherwise healthy woman comes in to your ED complaining of an itchy red rash that started soon after eating some seafood at a restaurant. She complains of a scratchy feeling in her throat, but denies any difficulty breathing, speaking or swallowing. She denies lip or tongue swelling, SOB, abdominal pain, vomiting or fever. On exam, her vitals are normal. She appears uncomfortable, scratching at her neck with an obvious raised patchy red urticarial rash all over her neck and torso. Her voice is normal, lips and tongue do not appear swollen, there’s no stridor and her chest is clear.
Q1: Is this anaphylaxis or is this simply an allergic reaction that we don’t have to treat aggressively?
Diagnostic Criteria for Anaphylaxis
Anaphylaxis is highly likely when any one of the following three criteria is fulfilled:
1. Acute onset of an illness (minutes to hours), with involvement of the skin, mucosal tissues, or both AND at least one of the following:
- Respiratory compromise
- Reduced blood pressure or associated symptoms of end‐organ dysfunction
2. Two or more of the following that occur rapidly (minutes to hours) after exposure to a likely antigen for that patient:
- Involvement of the skin‐mucosal tissue
- Respiratory compromise
- Reduced blood pressure or associated symptoms of end‐organ dysfunction d. Persistent gastrointestinal symptoms
3. Reduced blood pressure after exposure to a known allergen for that patient (minutes to hours)
- Infants and children: low systolic blood pressure (age‐specific) or >30% decreased in systolic blood pressure
- Adults: systolic blood pressure 30% decrease from that patient’s baseline
Adapted from: Sampson HA, Munoz‐Furlong A, Bock SA, et al. Symposium on the definition and management of anaphylaxis: summary report. J Allergy Clin Immunol 2005; 115:584‐91.
Note that according to this definition of anaphylaxis, isolated hypotension after an allergen exposure can be diagnostic for anaphylaxis, and that anaphylaxis can occur without any skin manifestations.
The importance of epinephrine timing, location and dose in anaphylaxis
Q2: Is epinephrine indicated for this patient?
If the “scratching feeling in her throat” is deemed by you to be a significant respiratory symptom that indicates any compromise, then according to the definition, this patient fulfills the diagnostic criteria for anaphylaxis.
All patient who fulfill the criteria for anaphylaxis require the administration of epinephrine. Epinephrine is the only drug to show a mortality benefit in the management of anaphylaxis.
Q3: How will you administer the epinephrine in the ED? What route, what location, what dose?
Epinephrine should be administered as soon as the diagnosis of anaphylaxis is made intramuscularly in the anterolateral thigh. Administering epinephrine IM in the deltoid muscle is not recommended.
Q4: One of the more common causes of death in anaphylaxis is giving the wrong dose. What is the correct dose of epinephrine?

Take home point #1:
The most common cause of death in anaphylaxis
is not giving epinephrine at the right time at the correct dose
Second line agents for anaphylaxis
Q5: What’s the evidence for the effectiveness of the addition of H2 blockers to H1 blockers in the symptomatic relief in allergic reactions and anaphylaxis?
One study from The Annals of EM in 2000 looked at 91 adults presenting to the ED with urticaria, acute angioedema, acute unexplained stridor or acute pruritic rash within 12 hours of ingested food, drug or contact with latex. They found that the combination of 50mg of diphenhydramine plus 50mg of ranitidine compared to diphenhydramine plus placebo was significantly more likely to result in absence of urticaria at 2 hours (91.7% in the ranitidine group vs 73.8% in the placebo group).
While the addition of H2 blockers to H1 blockers may help resolve urticaria faster, the true clinical significance of this is unknown.
Certainly, there is no evidence in the literature to suggest that either H1 or H2 blockers have a mortality benefit in the treatment of anaphylaxis.
Update 2017: A double-blind RCT compared the efficacy of levocetirizine plus 4-day course prednisone vs. levocetirizine plus placebo for acute urticaria. The addition of prednisone did not improve the symptomatic and clinical response to levocetirizine. This study did not support the addition of corticosteroid to H1 antihistamine as first-line treatment of acute urticaria without angioedema. Abstract
Update 2017: A retrospective chart review looked at 2376 patients having allergic reactions and compared patients who received H1 antihistamines to those who did not. The study found a higher progression to anaphylaxis in the patients who were not treated. However, there appears to be differences between the two groups – most notably, 7.8% of the antihistamine group, as compared to only 2.8% of the non-treatment group, were treated with epinephrine “before the development of anaphylaxis”. Overall, this study suggests early H1a treatment in the ED or prehospital setting may decrease progression to anaphylaxis. Abstract
Update 2020: An RCT of 262 adult patients presenting to EDs and urgent care centers with acute urticaria requiring an intravenous antihistamine were randomized to either the 2nd generation antihistamine intravenous cetirizine 10 mg or intravenous diphenhydramine 50 mg. Intravenous cetirizine was found to be an effective alternative to intravenous diphenhydramine for treating acute urticaria, with less sedation, fewer adverse events, shorter time spent in treatment center, and lower rates of revisit to treatment center. Abstract
Q6: What about steroids? Which patients require steroids in the ED for anaphylaxis?
There is a paucity of evidence for the efficacy of steroids in patients with allergic reactions or anaphylaxis. Nonetheless, corticosteroids are standard care for patients with anaphylaxis. Our expert’s practice is that if the patient fulfills the diagnostic criteria for anaphylaxis, give epinephrine AND steroids. While there is no good evidence in the literature that the addition of steroids to epinephrine has a mortality benefit or prevents a biphasic reaction, it is still recommended by our expert, but only if the setting of true anaphylaxis.
If the patient does not fulfill the diagnostic criteria for anaphylaxis, then steroids are not indicated.
Remember that steroids take 4-6hrs to become effective, so (in contradistinction to epinephrine) there is no rush to administer them.
If you do give steroids, our expert recommends single dose dexamethasone in the ED, which has the advantage of a long half-life of 53hrs, thus negating the need for prescribing steroids upon discharge.
Take home point #2
If you don’t give epinephrine (ie the patient does not have anaphylaxis) then don’t give steroids.
Observation time in anaphylaxis
Q7: How long to do you need to keep patients with allergic reactions with or without anaphylaxis in the ED? Which patients might you want to observe for a prolonged period of time in the ED?
While traditionally patients with anaphylaxis are obvserved in the ED for 4-6hrs before discharge, there is no literature to support this practice. Some experts recommend observing patients until they become asymptomatic regardless of time. It may be prudent to observe patients longer who have been shown in observational studies to be at high risk for severe anaphylaxis.
The risk factors for severe anaphylaxis are:
- patients taking anti-hypertensive medication
- early symptom onset and late treatment initiation
- asthmatics
- past history of severe reactions
Biphasic reactions in anaphylaxis
Q8: Do we need to worry about biphasic reactions in deciding how long to observe patients for? How effective are steroids at preventing biphasic reactions in anaphylaxis?
Observational data have shown that biphasic reactions in anaphylaxis can occur any time between 1 hour and 7 days after the initial anaphylactic episode in approximately 2-5% of patients.
Recent literature has found that the rate of biphasic reactions may be lower than previously stated. In a Canadian observational study out of Annals of EM in 2013 of 496 anaphylactic patients and 2,323 allergic reactions, clinically important biphasic reactions occurred in only 0.18% of patients with no deaths. While it is tempting to conclude from this study that biphasic reactions are so rare that they become almost irrelevant, this study was not confined to patients with anaphylaxis. The vast majority of these patients did not fulfill the criteria for true anaphylaxis and likely had minor allergic reactions which would have gotten better by themselves, regardless of medications.
In another Canadian retrospective cohort study from Annals of EM in 2015 of 473 anaphylacitc patients and 2,701 allergic reactions, they looked at the number of subsequent allergy-related ED visits within 7 days (a “relapse”) in steroid and non-steroid exposed groups. They found that the 7-day bounce back rate was 5.8% in the steroid group vs 6.7% in the no steroid group. The number needed to treat (NNT) to prevent one ED relapse visit was 176. Again, the issue with this study, was that only a small proportion of patients actually fulfilled the criteria for true anaphylaxis, with only 54% receiving epinephrine.
Therefore, we cannot assume from these studies that steroids play no role in preventing relapses or biphasic reactions in anaphylaxis. Until large validated RCTs can show definitely that steroids are not effective in this respect, it still remains standard care to administer steroids along with epinephrine for patients with true anaphylaxis.
Take home point number #3
While there is no good evidence that steroids decrease the relapse rate or rate of biphasic reactions,
further studies are required to abandon steroids for the treatment anaphylaxis.
The administration of epinephrine in adequate doses early in the illness course may prevent biphasic reactions.
Q9: What counseling do you provide patients who are discharged from the ED after anaphylaxis?
One of the more common reasons for death in anaphylaxis,
is the patient not self-administering the epinephrine auto-injector
or not administering it properly
Sometimes patients do not self-administer the epinephrine auto-injector (even if they are carrying it on their person) or do not administer it properly. It is therefore imperative not only to give the patient a script for epinephrine auto-injectors on discharge from the ED, but to take the time to counsel patients on the use of them. It is recommended for patients to carry 2 epinephrine auto-injectors as the adult ones only contain 0.3mg of epinephrine, and many patients will require 2 doses. In one study only 32% of patients could demonstrate that they knew how to use the epinephrine auto-injector correctly. In the same study, only 36% of pediatric residents showed they could use an auto-injector correctly and, sadly, only 18% of attending physicians could do so.
Epinephrine auto-injector instructions for patients being discharged from the ED after anaphylaxis
- Remove the auto-injector from its case
- Remove the safety release mechanism, making sure that the blue end points away and the orange end points to the thigh (“Blue to the Sky, Orange to the Thigh“)
- Firmly push the auto-injector against the middle of the outer thigh (through the pants if necessary) until a clicking sound is heard
- Hold the auto-injector firmly in place against the thigh for 10 seconds to deliver the medication
- Remove the device from the thigh and call 911
Q10: Besides 2 epinephrine auto-injectors, what other medications will you prescribe on discharge from the ED?
Our expert recommends prescribing a non-sedating antihistamine during the day and a sedating one such as diphenhydramine in the evening for 72 hours. There is no need to prescribe steroids if dexamethasone was given in the ED as the duration of action is approximately 2-3 days.
Anaphylactic Shock
CASE 2: A 63 year-old man gets rushed into your resuscitation room by EMS. He was well until about 30 mins before arrival when he complained to his wife of feeling weak and dizzy. His wife noticed that he looked really unwell and called 911 immediately. EMS found him with a GCS of 13 and blood pressure of 72 on palp. He’s otherwise healthy except for a history of hypertension. There was no history of chest pain, SOB, palpitations, headache, back pain or fever, vomiting or diarrhea and no melena. He saw his Family Physician the day prior, complaining of urinary frequency, and was started on Septra – sulphamethoxazole-trimethoprim. He took it as prescribed about 1 hour ago. EMS started a bolus of normal saline in a peripheral IV and in the ED his BP remains around 70 on palp. A second peripheral line is started, more saline under pressure bags is infused, a quick cardiac, respiratory and belly exam are unremarkable and an ECG and POCUS don’t show any striking abnormalities except that the LV looks hyperdynamic and the IVC looks collapsed.
Q11: Can isolated hypotension be the only finding in anaphylaxis?
As outlined above in the diagnostic criteria of anaphylaxis, isloated hypotension after exposure to a presumed allergen is enough to make the diagnosis of anaphylaxis. Obervational studies show that up to 20% of patients do not have a rash with their anaphylaxis. While this patient could be suffering from septic shock, and consideration should be given to this in the work-up and management, he also fulfills the diagnostic criteria for anaphylactic shock which is a more time-sensitive emergency than septic shock.
Pitfall: Assuming the patient does not have anaphylaxis just because they don’t have a rash
Case continued: This patient gets 0.5mg of 1:1000 epinephrine IM in the antero-lateral thigh and his pressure is still 70/palp, and so 5 minutes later he gets a second dose, and his pressure is still only 70 on palp.
Q12: How would you administer epinephrine in this scenario of a patient in presumed anaphylactic shock who’s had 2 intramuscular doses of epinephrine that haven’t improved his blood pressure?
After 2 intramuscular injections of 0.01mg/kg (max 0.5mg) epinephrine 5 minutes apart, it’s time to move on to IV epinephrine.
Steps for drawing up epinephrine for push dose epinephrine and epinephrine infusion
- Inject 1 mg of epinephrine 1:10,000 (one amp of crash cart epi)
into a 1L bag of normal saline - Draw up 10mL from the 1L bag in a 10mL syringe (The concentration of epinephrine in the syringe is now 1 mcg/mL)
Push Dose: 10 mL every 2-5 minutes (10 mcg)
- note that the onset = 1 minute and duration = 5-10 minutes
Dose of epinephrine given via infusion: 1mL/min (1 mcg/min) and titrate to a maximum of 20mL/min
Note that starting May 2016, the current 1:1,000 vs 1:10,000 concentration of epinephrine will be replaced by 1mg/mL and 0.1mg/mL respectively to minimize confusion leading to medication dosing error.
Case Continued: You give your push dose epinephrine and you’ve maxed out on 20mL/min infusion and the patient remains hypotensive.
Q: What is your next move after maxing out on your IV epinephrine infusion?
Do not underestimate profound vasodilatory shock that occurs in anaphylactic shock. First, aggressive fluid resuscitation is indicated for patients with anaphylactic shock via rapid infuser or short large peripheral IVs with pressure bags. Second, consideration may be given to a second vasopressor. There exists some anecdotal evidence for vasopressin as a second line vasopressor, however our expert recommends whatever vasopressor with alpha properties that you are most familiar with.
Vasopressin dose: 1-5mg IV bolus followed by infusion of 1-5mg/hr
Take home point #4
Anaphylaxis, can present with isolated hypotension, or hypotension plus vomiting, or hypotension plus wheezing without rash.
Not recognizing this in a timely manner can lead to misdiagnosis and death.
Pearl: a cognitive forcing strategy that can be employed whenever you are presented with a patient who appears to be in septic shock, is to ask yourself “could this be anaphylactic shock” and inquire about possible recent allergen exposure, previous anaphylaxis and the rapidity of onset.
CASE 3: A 43 year-old is brought to the ED by his wife with an allergic reaction to Cloxacillin. He complained of nausea, vomited once and some shortness of breath along with his urticarial rash. He was given epinephrine 0.5mg IM, and soon after started complaining of chest pain. His ECG shows an obvious anterolateral STEMI.
Q: What happened here? Did you cause an MI with your IM epinephrine? Did this man have underlying coronary disease that you should have asked about as a contraindication to epinephrine?
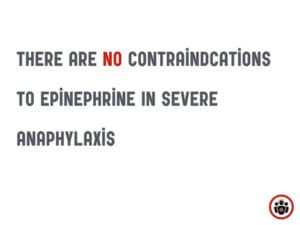
Epinephrine in the correct dose for anaphylaxis generally does not cause MIs. There are no absolute contraindications to epinephrine in severe anaphylaxis.
The diagnosis is in this case is Kounis Syndrome.
Kounis Syndrome: Anaphylaxis of the coronary arteries
Kounis syndrome is essentially an allergic myocardial infarction; an acute coronary event in the setting of an anaphylactic reaction.
There are 3 subtypes of Kounis Syndrome:
Type I – normal coronary arteries and no cardiovascular risk factors
Type II – pre‐existing coronary artery disease
Type III – coronary stent thrombosis due to anaphylaxis
A bit of basic pathophsyiology is helpful to understanding how one ends up with a STEMI after anaphylaxis:
There is a high density of mast cells present in the coronary arteries in people with coronary artery disease. When anaphylaxis occurs, chemical mediators induce coronary artery vasospasm as well as platelet activation. In patients with existing CVD, these conditions can promote plaque rupture and stent thrombosis.
The management of patients with Kounis syndrome can be challenging. The emergency provider must treat both the allergic and cardiac manifestations of anaphylaxis. Unfortunately, no guidelines exist for the management of patients with acute coronary events in the setting of anaphylaxis. Theoretically, epinephrine may worsen coronary vasospasm and worsen myocardial ischemia. Nonetheless, epinephrine should still be given as the initial treatment of choice. In one case series, 24% of patients with Kounis syndrome received epinephrine and there were no deaths. Cardiac catheterization with intracoronary vasodilator infusion or thrombus evacuation has been used successfully to treat patients with Kounis syndrome.
Take home points for Anaphylaxis and Anaphylactic Shock
- The number one cause of death in anaphylaxis is failure to give epinephrine in a timely manner, in the correct location and in the correct dose.
- There are no contra-indications to epinephrine when it comes to severe anaphylaxis.
- Consider anaphylaxis in every patient who presents in shock, because anaphylaxis can present with isolated hypotension
For more on anaphylaxis and anaphylactic shock on EM Cases:
Episode 187 Crashing Anaphylaxis & the AMAX4 Algorithm – The Max McKenzie Case
Rapid Reviews Video on Anaphylaxis & Anaphylactic Shock
Dr. Helman and Dr. Carr have no conflicts of interest to declare.
References
Sampson HA, Muñoz-furlong A, Campbell RL, et al. Second symposium on the definition and management of anaphylaxis: summary report–second National Institute of Allergy and Infectious Disease/Food Allergy and Anaphylaxis Network symposium. Ann Emerg Med. 2006;47(4):373-80.
Lin RY, Curry A, Pesola GR, et al. Improved outcomes in patients with acute allergic syndromes who are treated with combined H1 and H2 antagonists. Ann Emerg Med. 2000;36(5):462-8.
Grunau BE, Wiens MO, Rowe BH, et al. Emergency department corticosteroid use for allergy or anaphylaxis is not associated with decreased relapses. Ann Emerg Med 2015; 66:381‐9.
Grunau BE, Li J, Yi TW, et al. Incidence of clinically important biphasic reactions in emergency department patients with allergic reactions or anaphylaxis. Ann Emerg Med. 2014;63(6):736-44.e2.
Lee S, Bellolio MF, Hess EP, Erwin P, Murad MH, Campbell RL. Time of Onset and Predictors of Biphasic Anaphylactic Reactions: A Systematic Review and Meta-analysis. J Allergy Clin Immunol Pract. 2015;3(3):408-16.e1-2.
Rohacek M, Edenhofer H, Bircher A, Bingisser R. Biphasic anaphylactic reactions: occurrence and mortality. Allergy. 2014;69(6):791-7.Regis AC, Germann CA, Crowell JG. Myocardial Infarction in the Setting of Anaphylaxis to Celecoxib: A Case of Kounis Syndrome. J Emerg Med. 2015;49(2):e39-43.
Ralapanawa DM, Kularatne SA. Kounis syndrome secondary to amoxicillin/clavulanic acid administration: a case report and review of literature. BMC Res Notes. 2015;8:97.
Lieberman P, Simons FE. Anaphylaxis and cardiovascular disease: therapeutic dilemmas. Clin Exp Allergy 2015; 45:1288‐9.
Simons FER, Gu X, Simons KJ. Epinephrine absorption in adults: intramuscular versus subcutaneous injection. J Allergy Clin Immunol 2001; 108:871‐6.
Sheikh A, Ten Broek VM, Brown SG, et al. H1‐antihistamines for the treatment of anaphylaxis: Cochrane systematic review. Cochrane Database Syst Rev 2007; CD006160.
Choo KJ, Simons FE, Sheikh A. Glucocorticoids for the treatment of anaphylaxis: Cochrane systematic review. Cochrane Database Syst Rev 2012; CD007596.
Brown SG, Blackman KE, Stenlake V, Heddle RJ. Insect sting anaphylaxis; prospective evaluation of treatment with intravenous adrenaline and volume resuscitation. Emerg Med J. 2004;21(2):149-54.
More FOAM Resources on Anaphylaxis
Ken Milne of Skeptics Guide to Emergency Medicine: SGEM#57: Should I Stay or Should I Go (Biphasic Anaphylactic Response)
Kane Guthrie of Life in The Fast Lane: Pearls and Pitfalls
Bryan Hayes of Academic Life in EM: Epinephrine Dosing for Patients on Beta Blockers
Justin Morgenstern of First10EM: The first 10 minutes of management
Zlatan Coralic goes over IV Epinephrine infusions on ALiEM
Scott Weingart’s handy Push dose pressors pocket card
Now test your knowledge with a quiz.







Thanks for a great episode – helped me to get my 15min of fame in the ED today! Current 4th year medical student in the States and listened to the episode on the way to my shift. First medical code was 56y male who came in with acute ‘dizziness’ in addition to vague abdominal pain. Hypotensive to 60s/40s so initially worried about AAA or GI bleed (FOB+). I had just listened to the ‘master clinician’ catch of isolated hypotension and mentioned anaphylaxis to the staff. He quickly developed diffuse erythema with itching, wheezing, and GERD-like syx before we pushed epi. Improved markedly over the next 10 minutes and stated that he also had a ‘marble in his throat’. Luckily we got the epi in soon enough to avoid an airway.
He was able to tell us later he had an Advil for back pain about 10 min before the symptoms started, apparently had used Excedrin or Tylenol exclusively in the past.
Thanks -John