I had the enormous honour of interviewing Dr. Ben McKenzie, EM physician and a PhD candidate at the University of Melbourne studying the topic of resuscitation algorithms in anaphylaxis and asthma. The tragic death of his son Ben McKenzie at the age 15 from hypoxic respiratory arrest as a result of anaphylaxis and asthma in 2021 has led Dr. McKenzie on a mission to prevent deaths from anaphylaxis and asthma by educating emergency providers around the world using his AMAX4 algorithm as a framework…
Podcast production, sound design & editing by Anton Helman
Written Summary and blog post Anton Helman September, 2023
Cite this podcast as: Helman, A. McKenzie, B. Crashing Anaphylaxis – AMAX 4 Algorithm and The Max McKenzie Case. Emergency Medicine Cases. September, 2023. https://emergencymedicinecases.com/crashing-anaphylaxis-amax4. Accessed April 23, 2024
Anaphylaxis Definition
According to the World Allergy Organization (WAO)
1 or 2:
1. Acute onset laryngeal involvement, bronchospasm or hypotension after exposure to a known or highly probable allergans for that patient (minutes to several hours) even in the absence of skin symptoms
2. Acute onset of an illness (minutes to several hours) with simultaneous involvement of skin, mucosal tissue, or both
and 1 or more of the following
1.Respiratory compromise (dyspnoea, wheeze-bronchospasm, stridor, hypoxemia
2.Reduced BP or associated symptoms of end organ hypoperfusion (eg hypotonia, syncope, incontinence)
3.Severe GI symptoms (eg severe crampy abdominal pain, repetitive vomiting, especially after exposure to non-food allergens.
The key clinical clues of impending arrest secondary to anaphylaxis are any acute onset of a ) hypotension and/or b) bronchospasm and/or c) upper airway obstruction where anaphylaxis is considered possible, even if typical skin features are not present.
7 Maximum Medications to consider in Crashing Anaphylaxis: Epinephrine, Rocuronium, Ketamine, Bronchodilators, Magnesium Sulphate, Vasopressors, Steroids
1.Push dose epinephrine 1mcg/kg IV push then 1mL/kg/min and titrate
2.Rocuronium 1.2mg/kg IV push paralytic if patient is maintaining muscle tone
3.Ketamine 1-2mg/kg IV induction agent if patient is maintaining muscle tone; consider ketamine infusion 1-10 mg/kg/hr for it’s bronchodilator properties
4.Continuous bronchodilators in circuit (salbutamol 0.5 mg/kg/h (max 15 mg/h) + ipatropium 3 x 250 mcg for a 1-hour continuous nebulization) or IV (eg IV salbutamol 10-15 mcg/kg loading dose, then 5 mcg/min, increase by 5 mcg/min to a maximum of 20 mcg/min)
5.IV Magnesium sulphate 40 mg/kg to 75 mg/kg over 20 to 30 minutes (max 2.5 g)
6.Noradrenaline +/- vasopressin to target a perfusing BP
7.IV steroids [eg. Methylprednisolone 1 to 2 mg/kg (max 80 to 125 mg) or Hydrocortisone 5 to 8 mg/kg (max 400 mg)]
Hypoxic respiratory arrest is the cause of death in the majority of pediatric fatal anaphylaxis cases
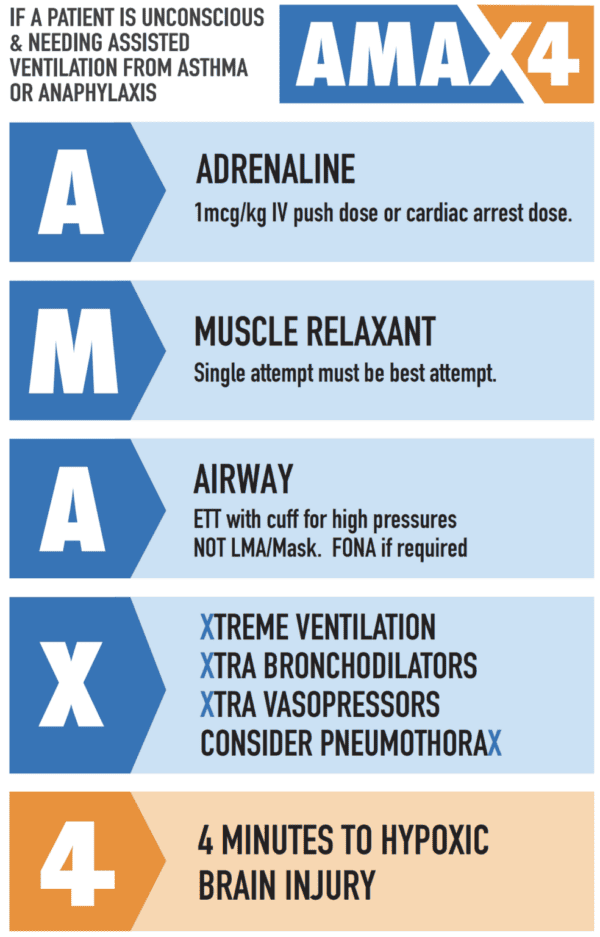
The majority of pediatric patients with severe anaphylaxis suffer a hypoxic respiratory arrest as a result of severe bronchospasm. Hypoxic brain injury after respiratory arrest ensues within 4 minutes, so the necessary treatments need to be coordinated and completed as efficiency and rapidly as possible. Chest compressions do not significantly alter the time to hypoxic brain injury as circulating oxygenated blood does not prevent hypoxic brain injury. The usual CABCs do not apply to this sub-population of crashing anaphylaxis patients with bronchospasm. Airway management is paramount. The old ABCs mnemonic applies.
Simulation practice is invaluable for teams to accomplish this goal of airway control and delivery of life-saving medications within 4 minutes.
Food allergy is the most common trigger of severe anaphylaxis with bronchospasm in pediatric patients.
Endotracheal intubation via RSI is the airway strategy of choice and should not be delayed in the unconscious patient with suspected anaphylaxis
Endotracheal intubation via RSI is the airway strategy of choice and should not be delayed in the unconscious patient with suspected anaphylaxis as this strategy can handle the high airway pressures (50-100 cmH20) associated with severe bronchospasm. Supraglottic devices and BVM cannot handle the high airway pressures and therefore not recommended in this patient population. An endotracheal tube with an inflated cuff is the only effective method to oxygenate an arrested anaphylaxis or asthma patient. ETT has the added benefits of preventing aspiration and avoid airway obstruction as a result of progressive upper airway edema. Time to full sedation should not delay the endotracheal intubation attempt in the arrested patient.
The initial attempt at securing the airway should be done by the most experienced person in the room immediately. If the first attempt at endotracheal intubation fails (“can’t intubate, can’t ventilate), front of neck surgical access such as a cricothyrotomy should be performed immediately.
Initial breaths after securing the airway should be delivered via manual bag compressions and lateral chest squeeze after each breath delivered (rather than with a ventilator) while maximal medical therapy is continued. Once switched onto the ventilator, use 6mL/kg volume, low I:E ratio, RR 8-12, no PEEP initially, and avoid breath stacking.
The risk of obstructive hyperinflation and pneumothorax
If the airway maneuvers and medicines are not effective immediately, consider pneumothorax and do not hesitate to perform bilateral finger thoracostomies if necessary.
The Max Mckenzie case
AMAX4 website AMAX4 – Every Second Counts includes more details of the AMAX4 algorithm, a pdf download lanyard card, lecture series and more.
Mike Betzner’s EMU talk on the crashing asthmatic/anaphylaxis patient
References
- Cardona V, Ansotegui IJ, Ebisawa M, El-Gamal Y, Fernandez Rivas M, Fineman S, Geller M, Gonzalez-Estrada A, Greenberger PA, Sanchez Borges M, Senna G, Sheikh A, Tanno LK, Thong BY, Turner PJ, Worm M. World allergy organization anaphylaxis guidance 2020. World Allergy Organ J. 2020 Oct 30;13(10)
- McKenzie, B. AMAX4 Lecture Series. Obtained from https://www.amax4.org/lecture September, 2023.
Drs. Helman and McKenzie have no financial conflicts of interest to declare





2021 UK Resuscitation guidelines for treatment of refractory anaphylaxis is:
Peripheral low-dose IV adrenaline infusion:
• 1 mg (1 mL of 1 mg/mL [1:1000]) adrenaline in 100 mL of 0.9% sodium chloride
• In both adults and children, start at 0.5–1.0 mL/kg/hour and titrate according to clinical response
Based on this guidance, the preparation contains 1000 mcg in 100 mL, or 10 mcg/mL.
An infusion rate of 0.5–1.0 mL/kg/hour works out as 5-10 mcg/kg/hr which is notably different from your IVI dose of 1mcg/kg/min.
For example, in a 60kg patient:
UK Resuscitation: 5-10 mcg/min
You: 60 mcg/min
Are you sure about your dose?
Thanks for picking up that error – it’s been edited to the correct dose