Not all bradycardias were created equal. How do we figure out when bradycardia is due to a medical illness and when it is a primary cardiac problem? What are the 4 immediate life threatening diagnosis that we have to entertain and address in the first few minutes of the sick bradycardic patients? What are some key ECG patterns that are sometimes missed by ED docs that can have devastating consequences? How can we better understand Torsades de Pointes by understanding AV blocks? How can we better understand Mobitz l and ll using ‘The Dorian’ approach? What is BRASH syndrome and how can we recognize it? In this main episode podcast 4-step Approach to Bradycardia and Bradydysrhythmias with electrophysiologist, educator and researcher Dr. Paul Dorian and Chair of Education for the ED at Cook County Hospital Dr. Tarlan Hedayati, we dig deep into bradycardia…
Podcast production and editing by Anton Helman
Voice editing by Sheza Qayyum, sound design my Yuang Chen & Anton Helman
Written Summary and blog post by Winny Li, edited by Anton Helman April, 2021
Cite this podcast as: Helman, A. Hedayati, T. Dorian, P. Episode 154 – 4-Step Approach to Bradycardia and Bradydysrhythmias. Emergency Medicine Cases. Month, 2018. https://emergencymedicinecases.com/approach-bradycardia-bradydysrhythmias. Accessed [date]
Go to part 2 of this 2-part podcast on bradycardia and bradydysrhythmias
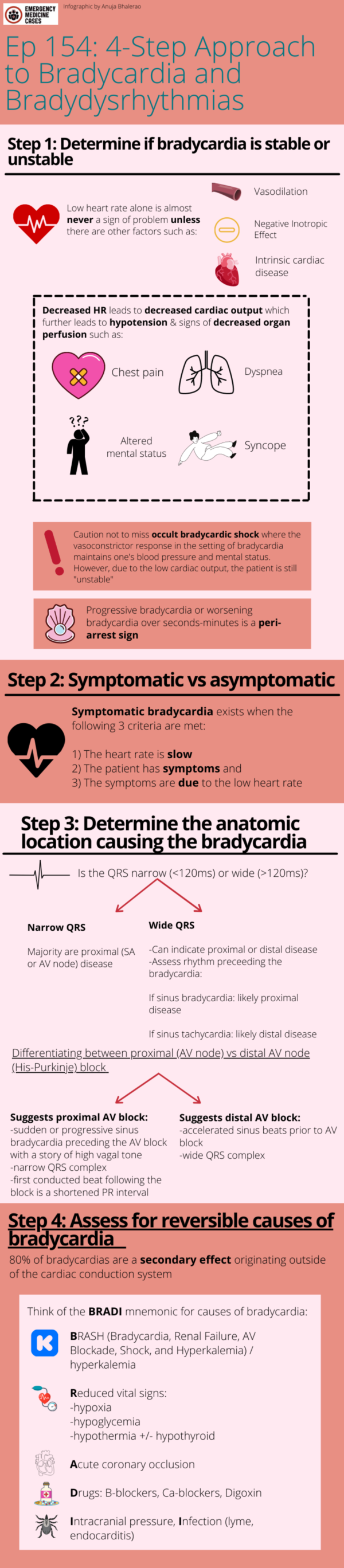
4-step approach to bradycardia in the ED
These steps are often done in parallel.
- Stable vs. unstable
- Symptomatic vs. asymptomatic
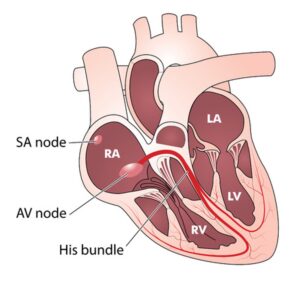
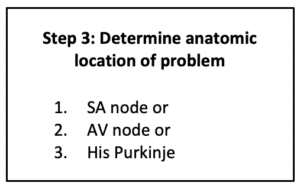
- Determine the anatomic location causing the bradycardia: SA node, AV node or His-Purkinje
- Assess for secondary causes of bradycardia
Step 1: Determine if bradycardia is stable or unstable requiring immediate treatment
The history and physical exam are paramount in helping make the decision of whether a patient with bradycardia is stable or unstable. Athletes and healthy people who are sleeping may normally have heart rates in the 30’s, so the heart rate alone is almost never a sign of instability, unless there is another factor at play: underlying vasodilation, negative inotropic effect or intrinsic cardiac disease. Nonetheless, be extra-weary in patients with progressive bradycardia or worsening bradycardia: 50s then 40s then 30s then 20s. This is a sign of pre-arrest.
Pearl: progressive bradycardia or worsening bradycardia over seconds-minutes is a peri-arrest sign.
Cardiac output is dependent on heart rate and stroke volume. Depressed cardiac output in the setting of overt bradycardic shock will manifest as hypotension, as well as signs of decreased organ perfusion such as altered mental status, chest pain, dyspnea or syncope – all signs of an “unstable” bradycardic patient. However, be cautious to not miss occult bradycardic shock where the vasoconstrictor response in the setting of bradycardia maintains ones blood pressure and mental status. The patient however may still have low cardiac output and thus be “unstable”. The clinical exam assessing for poor end-organ perfusion (altered LOA, cool extremities, low urine output etc) is critical in diagnosing occult bradycardic shock.
Step 2: Symptomatic vs. asymptomatic
It is important to determine if the bradycardia is causing symptoms (an older patient with underlying cardiac disease with chest pain and syncope), or if symptoms are the cause for bradycardia (vasovagal bradycardia), as this will direct management.
Symptomatic bradycardia exists when the following 3 criteria are met:
- The HR is slow
- The patient has symptoms and
- The symptoms are due to the slow HR
Asymptomatic bradycardia generally does not require any emergency treatment.
Step 3: Determine the anatomic location causing the bradycardia
Correct identification of the location of the problem (SA node vs. A node vs. His Purkinje) guides management of bradycardia. Sinus and AV nodal dysfunction rarely leads to life-threatening complications and are treated with watchful waiting, atropine or sympathetic medications such as epinephrine and dopamine. However, distal His-Purkinje block is much more serious, and tend not to respond to atropine and sympathetic stimulation. These patients almost always need pacing and a definitive pacemaker.
Simplified approach to identifying the location of the problem causing bradycardia:
Common types of bradycardia and syndromes associated with bradycardia
- Sinus bradycardia
- Junctional bradycardia
- 1st Degree AV block
- 2nd Degree AV block
- Ventricular escape rhythm and complete heart block
- Tachy-brady syndrome
- Bradycardia-induced Torsades de Pointes
- BRASH Syndrome
Sinus Bradycardia
Symptomatic sinus bradycardia and syncope of the vasovagal type in young healthy people may be associated with very long pauses (>30 seconds). The duration of the pause should not necessarily be a cause for concern. This is transient and the treatment is reassurance. In some circumstances, symptomatic sinus bradycardia may need to be treated if the quality of life of the patient is significantly impacted.
Junctional Bradycardia
A junctional rhythm occurs when the electrical activity of the SA node is blocked or is less than the automaticity of the AV node/His bundle. The rate is usually <40 bpm. The QRS is typically narrow, and P waves can be retrograde, narrow or absent.

Sinus node dysfunction with junctional rhythm and absence of any p-waves until the end of the tracing.

Marked sinus bradycardia with complete AV block with junctional escape.
Common causes of junctional bradycardia
- B-blocker, calcium channel blocker, digoxin poisoning
- Post cardiac valve surgery
- Inferior MI with RV extension or posterior MI
1st Degree AV block
For the most part, 1st degree AV block with a prolonged PR interval is benign. However, if the patient presents with an acute cardiac-related symptom and the 1st degree AV block is new, it may not be benign.
Pearl: Lyme carditis can present with new, long 1st degree AV block and may degenerate into complete heart block. These patients should be considered for admission for observation on telemetry.
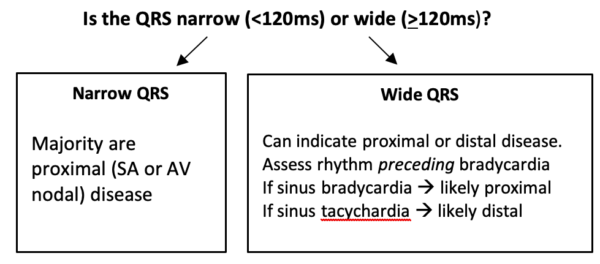
Dr. Dorian’s approach to AV block: proximal vs. distal AV block
Our expert Dr. Dorian prefers to approach AV block by thinking about the location of the block, whether the block occurs in the proximal conducting system (AV node) or the distal conducting system (His-Purkinje). The reason why classifying AV block by 2nd degree Type 1 and 2 is less helpful is because there are instances where “high-grade” AV blocks such as 2:1 AV block (2 p waves for every 1 QRS – see image below) occurs secondary to intrinsic AV nodal disease and the treatment for these patients is generally conservative; whereas patients with distal AV block do not respond to atropine or sympathetic stimulation and need pacing.
The key to teasing apart where the conductive disease lies is looking for the rhythm preceding the onset of the block.
Key ECG clues that help differentiate proximal vs. distal AV block
Clues that suggest proximal AV block
- Sudden or progressive sinus bradycardia preceding the AV block with a story of high vagal tone
- Narrow QRS complex
- First conducted beat following the block is a shortened PR interval
Clues that suggest distal AV block
- Accelerated sinus beats prior to AV block
- Wide QRS complex

2:1 AV block. Wide complex QRS morphology suggests distal AV block.
Ventricular escape rhythm in the setting of complete AV block
Ventricular escape rhythms have an intrinsic rate of 20-40 bpm. QRS complexes are broad (≥120ms) and may have a LBBB or RBBB morphology.
The presence of a new slow bundle branch block against a sinus tachycardia is concerning for complete AV block requiring pacing.

Complete heart block with underlying sinus tachycardia with a ventricular escape rhythm (RBBB morphology).
Tachy-Brady syndrome
One variant of sinus node dysfunction (sick sinus syndrome) is tachy-brady syndrome. This syndrome tends to occur in older patients with a history of paroxysmal atrial fibrillation, and it manifests as conversion pauses or sinus bradycardia when the patient converts from atrial fibrillation to sinus, giving rise to presyncope/syncope.

Tachy-brady with atrial fibrillation with alternating bradycardia.
Pitfall: A common pitfall is to administer standard rate control agents such as beta blockers and calcium channel blockers to a patient who presents in rapid atrial fibrillation who has underlying tachy-brady syndrome. Rate control drugs will invariably worsen their underlying sinus node disease.
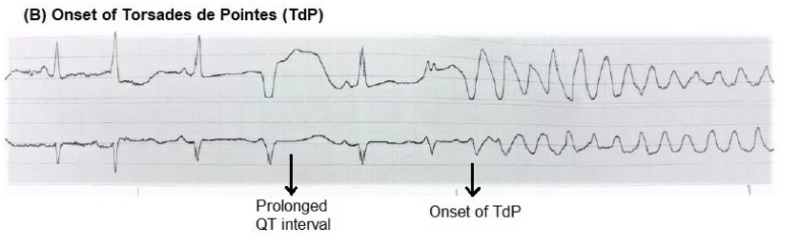
Bradycardia induced Torsades de Pointes
Torsades is a pause-dependent arrhythmia, which is more likely to occur at slower heart rates as bradycardia itself may prolong the QT. The first beat of the tachycardia often occurs on a delayed QT, causing ‘R on T’ which will usher a paroxysm of polymorphic VT. Torsades uncommonly occurs in the setting of sinus bradycardia, but not uncommon in the setting of bradycardia with AV block.
If you see the presence of bradycardia with AV block along with short runs of polymorphic VT, these patients need urgent treatment as they may degenerate into ventricular fibrillation.
Practice your identification of bradydysrhythmias in ECG Cases 20: Approach to Bradycardia and BRADI Mnemonic
BRASH Syndrome
BRASH syndrome (Bradycardia, Renal Failure, AV Blockade, Shock, and Hyperkalemia) refers to a vicious cycle which may occur in the setting of AV node blockers, renal failure and hyperkalemia. A patient on AV nodal blocking agents sustains renal injury, causing hyperkalemia which synergizes with AV nodal blockers causing a worsening spiral of hyperkalemia, renal failure, and bradycardic shock.
BRASH syndrome can be precipitated by dehydration, worsening of CKD due to co-morbidities, medication up-titration, addition of nephrotoxic agent, or any cause of hypoperfusion or renal dysfunction. The patient may be taking their AV blocker at the appropriate dose.
The treatment of BRASH syndrome centers around aggressive therapy for hyperkalemia. Additionally, many patients require a catecholamine infusion to support their perfusion.
Learn more about the management of hyperkalemia at Episode 86- Emergency Management of Hyperkalemia
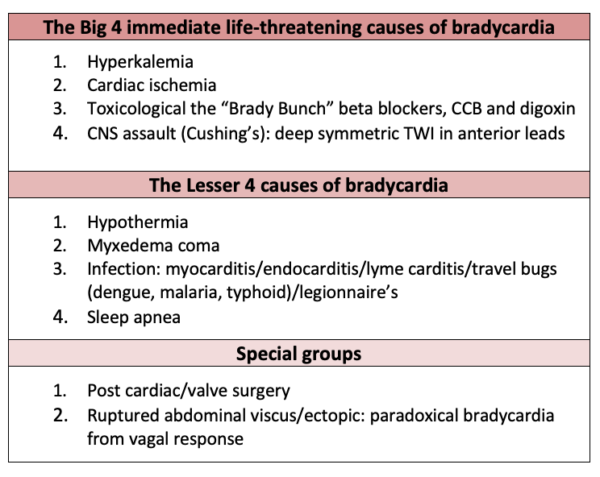
Step 4: Assess for reversible causes of bradycardia
80% of bradycardias are a secondary effect originating outside the cardiac conduction system. Asymptomatic, nocturnal or vagally induced bradycardia is most often benign and needs no specific treatment.
Always assess for easily reversible causes of bradycardias, the most common being AV nodal drugs, and high vagal tone.
The 4th step often needs to be done in parallel with steps 1-3 in order to rule out secondary cause or causes that if treated, may preclude the need for atropine, sympathetic stimulation and pacing. Identification of contributing factors for symptomatic bradycardia should be considered throughout the resuscitation since reversal of the cause will likely return the patient to a state of adequate perfusion.
If you prefer mnemonics to aid in recall of the differential diagnosis of bradycardia…
BRADI mnemonic for causes of bradycardia
- BRASH/hyperkalemia
- Isolated hyperkalemia
- BRASH syndrome (Bradycardia, Renal failure, AV node blockade, Shock and Hyperkalemia)
- Reduced vital signs
- Hypoxia
- Hypoglycemia
- Hypothermia +/- hypothyroid
- Acute coronary occlusion
- Inferior MI: nodal ischemia and vagal response, self-limiting or responds to atropine
- Anterior MI: infranodal ischemia, often requires pacing
- Drugs: withdraw if stable, reverse if unstable
- Beta-blockers
- Calcium channel blockers
- Digoxin
- Intracranial pressure, Infection (Lyme, endocarditis): treat underlying
Take home points on 4-step approach to bradycardia
- Be cautious with your history and physical exam to not miss occult bradycardic shock
- Bradycardia alone rarely causes instability, with the exception of progressive bradycardia, which is a sign of pre-arrest
- Determine if symptoms are causing bradycardia (vasovagal) or if bradycardia is causing symptoms
- Identify location of problem – which will determine whether urgent pacing is required or not
- Is the QRS narrow? Indicating proximal (SA/AV node disease); Is the QRS wide? Proximal or distal (His Bundle disease)
- Assess rhythm prior to bradycardia: sinus brady more likely to be proximal, sinus tachycardia more likely to be distal disease
- Junctional bradycardia is most commonly caused by toxicity from AV node blockers, post valve surgery and inferior MI
- Tachy-brady syndrome occurs in the setting of elderly patient with paroxysmal afib; do not treat these patients with AV node blockers
- Torsades can occur in the setting of bradycardia with AV block, and these runs of polymorphic VT can degenerate into Vfib
- Concurrently rule out secondary causes of bradycardia by considering the “Big 4 life threats” and “Lesser 4” causes
Practice your identification of bradydysrhythmias in ECG Cases 20: Approach to Bradycardia and BRADI Mnemonic
For part 2 of this series on Bradycardia go to Episode 155 Treatment of Bradycardia and Bradydysrhythmias
- F.M. Kusumoto, M.H. Schoenfeld, C. Barrett, J.R. Edgerton, K.A. Ellenbogen, M.R. Gold, et al.2018 ACC/AHA/HRS guideline on the evaluation and management of patients with bradycardia and cardiac conduction delay. J Am Coll Cardiol (2018) Oct 31. pii: S0735-1097(18)38984-8.
- Sidhu, S., & Marine, J. E. (2020). Evaluating and managing bradycardia. Trends in Cardiovascular Medicine, 30(5), 265-272.Deal N. Evaluation and management of bradydysrhythmias in the emergency department. Emerg Med Pract. 2013;15(9):1-15.
- Deal N. Evaluation and management of bradydysrhythmias in the emergency department. Emerg Med Pract. 2013;15(9):1-15.
- Ufberg JW, Clark JS. Bradydysrhythmias and atrioventricular conduction blocks. Emergency Medicine Clinics of North America. 2006;24(1):1-9.
- Yeung, A. Baranchuk. Diagnosis and treatment of Lyme carditis. J Am Coll Cardiol, 73 (2019), pp. 717-726.
- Namboodiri, N. (2010). Bradycardia-induced Torsade de Pointes–An arrhythmia Less Understood. Indian pacing and electrophysiology journal, 10(10), 435.
- Tintinalli JE, Stapczynski JS, Ma OJ, Cline D, Meckler GD, Yealy DM, eds. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. Eight edition. McGraw-Hill Education; 2016.
- Ashworth SW, Levsky ME, Marley CT, Kang CS. Bradycardia-associated torsade de pointes and the long-qt syndromes: a case report and review of the literature. Military Medicine. 2005;170(5):381-386.
- Farkas, J. D., Long, B., Koyfman, A., & Menson, K. (2020). BRASH syndrome: Bradycardia, renal failure, AV blockade, shock, and Hyperkalemia. The Journal of Emergency Medicine, 59(2), 216-223.
Drs. Helman, Dorian and Hedayati have no conflicts of interest to declare
Now test your knowledge with a quiz.


Excellent