Although it doesn’t get the spotlight much in emergency medicine, the ED diagnosis and management of elbow injuries is of significant clinical importance. There are several easy-to-miss injuries that can lead to functional impairment. Even minor errors in management can result in long term consequences for patients. In this EM Cases main episode podcast with Dr. Arun Sayal, the brains behind the CASTED Course and Dr. Dale Dantzer, upper extremity orthopedic surgeon at North York General Hospital, we discuss pitfalls in the diagnosis and management of elbow injuries and answer questions such as: What is an easy way to remember the surgical indications for radial head fractures? What is the significance of a coronoid process fracture and how does it change management when seen with a radial head fracture? What is the best way to assess for pronation and supination of the forearm? Why is it so important to assess for the extensor mechanism on physical exam for patients with olecranon fractures? What is a quick easy way to test the peripheral nerves of the upper extremities? Which often missed soft tissue injuries of the elbow require urgent operative management? and many more…
Podcast production, sound design & editing by Anton Helman
Written Summary and blog post by Shaun Mehta and Lorraine Lau, edited by Anton Helman March, 2019
Cite this podcast as: Helman, A. Sayal, A. Dantzer, D. Ten Pitfalls in the Diagnosis and Management of Elbow Injuries. Emergency Medicine Cases. March, 2019. https://emergencymedicinecases.com/elbow-injuries. Accessed [date]
Key concepts in elbow injuries diagnosis and management
- At 3 weeks of immobilization, there is high risk for chronic elbow stiffness and possible long-term disability
- While we don’t need to memorize orthopedic classification systems, we should glean key points from them
- Keep your differential broad for elbow injuries just like you would with a patient presenting with chest pain
- Learn how to recognize uncommon elbow injuries
Radial head fractures: Sometimes not so simple
The most common adult elbow fracture is a radial head fracture, often seen following a FOOSH—or fall on an outstretched hand—type of mechanism. Since force is transmitted along the entire extremity, ensure you fully examine from the sternoclavicular joint to the hand.
Radial head fracture mechanism of injury
Valgus stress = lateral force. The normal carrying angle of the elbow is slightly valgus. The vector of force with a FOOSH therefore goes through the lateral elbow where the radial head meets the elbow. This explains why the radial head and neck are often implicated, and why medial ligamentous structures are susceptible to injury as the medial side “opens up”.
Radial head fracture physical exam
To identify the radial head, make an equilateral triangle using the following landmarks:
- Olecranon (laterally)
- Lateral condyle (superior and anterior to the olecranon)
- Radial head = third point of the triangle
Pronating and supinating the forearm brings out the radial head.
The elbow is not just a hinge-joint
The elbow moves in supination and pronation, as well as flexion and extension. Ensure all ROMs are assessed on physical exam.

Testing pronation of the forearm. Ensure the elbows are held tight against the trunk. Normal pronation = 90 degrees with thumbs parallel to the floor.

Testing supination of the forearm. Ensure the elbows are held tight against the trunk. Normal supination = 90 degrees with thumbs parallel to the floor.
Pearl: Ask your patient to put their thumbs up while pronating and supinating to get a better sense of how close to their full range of motion they can get.
This video reviews the bony surface anatomy of the elbow including the radial head.
Make note of any mechanical blocks, with difficult pronation and supination being common in a radial head injury. Consider an Essex-Lopresti injury – this is a fracture-dislocation injury involving the radial head (fracture) and DRUJ – distal radioulnar joint (dislocation). Treatment for this specific injury is immobilization in supination.
Pitfall #1. Failure to test properly for pronation and supination range of motion. Testing for pronation and supination ROM with the elbows held tight against the trunk may reveal a subtle radial head or neck fracture or an Essex-Lopresti fracture-dislocation.
It is important to assess flexion/extension of the elbow with gravity eliminated because the weight of the forearm when gravity is not eliminated may be more painful for the patient and thus hinder full range of motion. One way to “eliminate gravity” is to have the patient point the tip of their elbow directly at you with their forearm parallel to the floor, and then asking them to flex and extend their elbow fully.
X-ray interpretation for radial head fractures
First, get a true lateral view x-ray for all elbow injuries
A true lateral x-ray is crucial for all elbow injuries. On a 2-dimensional image of an x-ray without orthogonal views, you can easily miss subtle findings. Subtle misalignments can sometimes only be picked up on one view and not on another.
To identify a true lateral view, look for:
- Superimposition of the trochlea and the capitellum
- The “hourglass” or “figure of 8” appearance
Consider a radial head injury in any of the following:
- Disruption of the usual smooth continuous concave shape of the radial head (may be very subtle or not visible on initial x-rays)
- Anterior sail sign
- Posterior fat pad sign
- Disruption of the radiocapitellar line

Joint effusion showing anterior “sail sign” and posterior fat pad sign

Radiocapitellar line. A line drawn through the middle of the radius normally goes through the middle 1/3 of the capitellum.
Pitfall #2: Accepting an inadequate AP x-ray view of the elbow if the patient is unable to extend the elbow enough. Consider separate x-ray views of the humerus and forearm to better assess the integrity of the bones of the elbow.
ED management of radial head fractures: The 30-3-33 Rule
Most radial head and neck fractures are not surgical and can be treated conservatively with a simple sling for comfort. For patients with significant pain and swelling, consider placing a backslab splint. Do not immobilize the elbow for >3 weeks due to risk of chronic elbow stiffness.
Pitfall #3. Immobilizing the elbow for >3 weeks. Prolonged immobilization may lead to chronic elbow stiffness and long term functional impairment.
The Mason classification gives guidance on when radial head/neck fractures may require operative fixation. For a simpler approach, consider expeditious surgical consultation if the fracture satisfies the 30-3-33 rule:
- >30 degrees angulation
- > 3 mm displacement of the fracture fragment
- > 33% surface area of the radial head involved
Looking for the second injury: the coronoid process fracture and the “terrible triad”
In suspected radial head and neck injuries, make sure to examine the coronoid process, or the anterior proximal portion of the ulna. Coronoid fractures tend to cause elbow instability and may require ORIF, and may be a sign of elbow subluxation or dislocation. They occur with FOOSH and elbow hyperextension, and present with pain over the antecubital fossa. Ask the patient if they felt a pop and subsequent reduction of the elbow during the fall. Coronoid fractures can be subtle on x-ray. It is imperative to look carefully for coronoid fractures on x-ray for all elbow injured patients as these tiny fractures may indicate an unstable joint.

Subtle coronoid process fracture.
Look out for the terrible triad of the elbow: a radial head fracture, coronoid fracture and elbow subluxation/dislocation. On x-ray, there may not be a sail sign because the hemarthrosis escapes the joint due to significant ligamentous injury.
A terrible triad injury is significant and requires a call to orthopedic surgery ASAP. Immobilize with a long arm posterior plaster splint, positioning the forearm in supination.
Pitfall #4. Failure to look for a second injury after diagnosing a radial head fracture. Specifically, look for a coronoid process fracture and subtle signs of subluxation by ensuring that the clear space around the trochlea is symmetrical and smooth.
Terrible triad: radial head fracture, coronoid process fracture and elbow subluxation
Posterior Elbow Dislocations
Posterior elbow dislocation mechanism of injury
The mechanism once again is a FOOSH but with elbow hyperextension usually a high force. Elbow dislocations (as opposed to shoulder dislocations) are associated with major ligamentous disruption. 90% of elbow dislocations are posterior. Posterior elbow dislocations are more common in teens.
Posterior elbow dislocation physical exam clues
On exam, the patient is often holding their elbow in 45 degrees of flexion. The posterior protuberance of the olecranon sitting posterior to the humerus is best seen from behind the patient. Palpate the medial condyle, lateral condyle and tip of the olecranon; normally they form a symmetrical isosceles triangle. If they don’t, consider a subluxation or dislocation of the elbow.
Pitfall #5. Assuming no dislocation if the joint appears in place in the ED. Some patients with elbow dislocation will have reduced spontaneously prior to your assessment. Usually the patient will recall the sensation that the joint “popped out” and then “popped back in” again. The x-ray may be unrevealing however, all elbow dislocations are associated with major ligament disruption and thus require rigid immobilization, even when the x-ray is normal.
As with any fracture or dislocation, perform a pre- and post-reduction neurovascular exam and look for signs of compartment syndrome.
Posterior elbow subluxation x-ray interpretation
Frank posterior elbow dislocations are obvious on x-ray. However subtle subluxations are often missed. For subtle subluxation look at the x-ray for a smooth, symmetric clear space around the trochlea, similar to assessing the clear space of the ankle mortise. Again, patients may have reduced their dislocation spontaneously before your assessment in the ED and the x-ray may be normal. If a fracture is identified and the story is consistent with a dislocation that was reduced spontaneously, this should be managed similarly to a dislocation found of x-ray that is reduced in the ED.
Elbow dislocation closed reduction: Traction-countertraction technique
Before the reduction attempt, place the forearm in supination. Muscle relaxation is crucial for any attempt to be successful.
- Assistant immobilizes humerus with elbow flexed at 30 degrees, applies countertraction at middle or distal humerus
- Apply traction to distal forearm with forearm supinated
- If unsuccessful, apply downward pressure at mid-forearm and the olecranon posteriorly while maintaining in-line traction
Pitfall #6. Failure to position the forearm in supination before posterior elbow dislocation reduction. It is important to place the forearm in supination to allow the trochlea of the humerus to more easily pass over the coronoid process of the olecranon during closed reduction.

Traction counter traction technique for closed reduction of elbow dislocation. Ensure that the forearm is supinated and that pressure is not applied over the antecubital fossa.
If the traction countertraction technique fails, standing at the posterior aspect of the humerus, hook the fingers of both your hands anterior to the condyles, trying to avoid compression in the antecubital fossa. Put both your thumbs on the olecranon at the junction with the triceps and use the leverage you can produce between your fingers and thumbs to push the olecranon up and over the trochlea.
Immobilize the elbow at 90 degrees of flexion with a well padded backslab and counsel the patient to expect that they will be unable to extend beyond 30 degrees for 6 weeks, may not regain full extension for at least 2-3 months, and are unlikely to return to weight-bearing exercises before 4 months. Simple dislocations (no fracture) require closed reduction and a brief period (<3 weeks) of immobilization in a back slab while elbow dislocations associated with a fracture usually requires ORIF and should be seen by orthopedics within 72 hours.
Olecranon fractures: it’s all about extensor mechanism integrity
Mechanism of injury: Olecranon fractures typically occur after a direct blow to the olecranon in older patients.
Physical exam: In the case of a suspected olecranon fracture, the most important element to assess is the extensor mechanism and the integrity of the triceps. Similar to the importance of assessing the integrity of the extensor mechanism of the knee for patella and quadriceps tendon injuries with an active straight leg raise test to predict the likelihood of operative intervention, make sure to check extension against mild resistance – one way to do this is to have the patient point the tip of their elbow directly at you with their forearm parallel to the floor, and then asking them to extend their elbow against the resistance of your hand.
Perform a neurovascular exam, specifically checking for ulnar nerve sensation and power. Also look for the second injury, in particular a subluxed elbow. All olecranon fractures are intra-articular, so look for asymmetry in the intact olecranon-coronoid interface to suggest subluxation.
Management: well padded posterior splint and sling
- Non-operative treatment: for < 2 mm displacement
- For olecranon fractures with 2 mm-5 mm displacement, management depends on patient age, extensor mechanism function and surgeon preference
- Operative treatment: for fractures with > 5 mm displacement and/or complete loss of extensor mechanism
Pitfall #7. Failure to assess the integrity of the extensor mechanism for patients with olecranon fractures. Patients with olecranon fractures who are unable to extend their elbow against resistance are likely to require operative intervention.
Monteggia fracture-dislocation
The forearm is a ring structure, and so force often results in injuries in two locations. If you see a fracture in one location, it is commonly associated with a dislocation in another location. A caveat to this rule is a “nightstick” fracture, which is an isolated forearm fracture from direct force to the forearm.
A Monteggia injury involves a fracture of the ulna and dislocation of the radial head. A Galeazzi injury involves a fracture of the radius and dislocation of the distal ulna or DRUJ. An easy way to remember which injuries are involved in a Monteggia fracture-dislocation is with the FUME mnemonic.
FUME mnemonic for Monteggia injury
Fracture of
Ulna is called
Monteggia when at the
Elbow, the other bone (radius) is dislocated
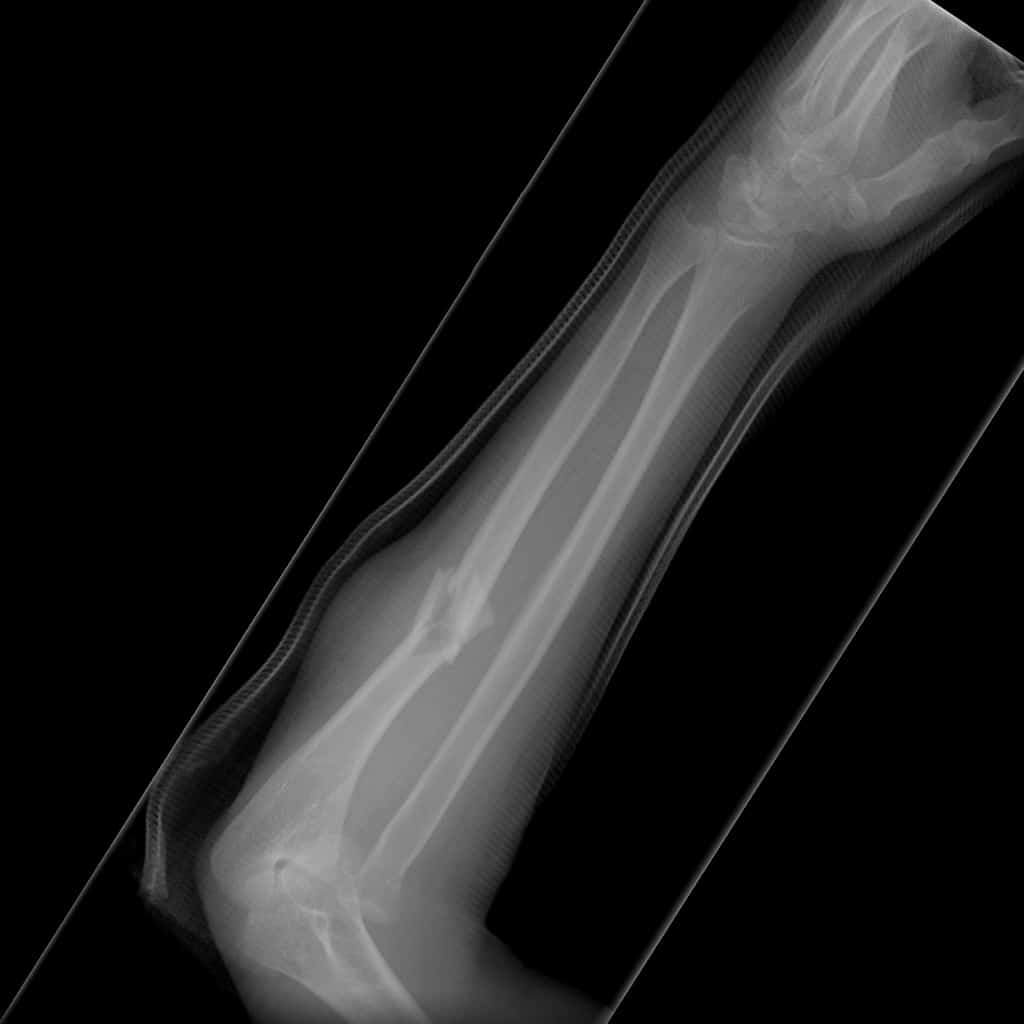
Monteggia fracture-dislocation. Note the radial head dislocation.
It is imperative to carefully assess for radial head subluxation for all ulna fractures by assessing the radiocapitellar line.

Radiocapitellar line. A line drawn through the middle of the radius normally goes through the middle 1/3 of the capitellum.
Pitfall #8. Failure to assess the radiocapitellar line for patients with ulna fractures. Monteggia fracture-dislocation is un unstable injury and is managed operatively, while an isolated nondisplaced ulna fracture is managed nonoperatively. Scrutinize the x-ray for radial head subluxation for all patients with ulna fractures.
Operative soft tissue injuries of the elbow
Distal biceps tendon injury
Distal biceps tendon injuries present in younger patients after lifting (or attempting to lift) a heavy object, whereas a proximal injury is often seen in older patients due to degenerative changes. Distal biceps tendon rupture requires urgent surgery, because after 3 weeks the muscle shortens/retracts and the tendon is difficult or impossible to retrieve. Distal biceps tendon rupture can be easily missed because they may not present with the classic “popeye sign” the way proximal biceps tendon ruptures do.
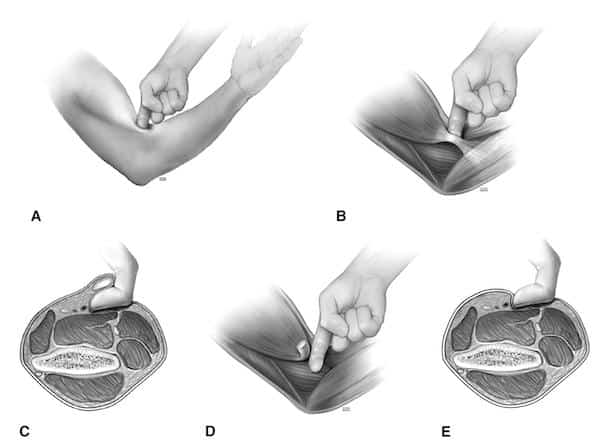
On exam, perform the Hook test: use your index finger to hook the biceps approaching it from the lateral/radial side. If there is no tendon palpable (an empty space without being able to “hook” the biceps tendon with your finger), there is likely a distal biceps rupture. For more details, see EM Cases Episode 58.
Pitfall #9. Assuming that urgent operative intervention is not required for all biceps tendon injuries. While proximal biceps tendon ruptures are usually managed nonoperatively, distal biceps tendon ruptures are usually managed operatively within 2-3 weeks of the injury.
Triceps tendon injury
Triceps tendon injuries often present in young, muscular male patients after forced extension from a FOOSH mechanism. They complain of pain in the posterior elbow region, and may have felt a pop during the injury.
Assess the extensor mechanism and feel for a divot on the posterior aspect of the elbow just proximal to the olecranon where the triceps tendon inserts. Place these patients in a sling and follow up with orthopedics. Operative management is usually required within 6 weeks of injury.
Pitfall #10: Routinely ordering ultrasound imaging for suspected biceps or triceps injuries. Ultrasound imaging is not required to diagnose biceps tendon rupture or triceps tendon rupture. Ultrasound reports may be misleading and are not recommended by our experts in this setting. These are clinical diagnoses.
Learn more about pediatric elbow injuries at EMU 365: Pediatric Elbow Nightmares
References for ten pitfalls in the diagnosis and management of elbow injuries
- Tintinalli, Judith E., et al. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. Eighth edition. New York: McGraw-Hill Education, 2016.
- Marx, John A., and Peter Rosen. Rosen’s Emergency Medicine: Concepts and Clinical Practice. 8th ed. Philadelphia, PA: Elsevier/Saunders, 2014.
- Pappas N, Bernstein J. Fractures in brief: radial head fractures. Clinical orthopaedics and related research. 468 (3): 914-6.
- Regan W, Morrey B. Fractures of the coronoid process of the ulna. J Bone Joint Surg Am. 1989;71 (9): 1348-54.
- Gottlieb M, Schiebout J. Elbow Dislocations in the Emergency Department: A Review of Reduction Techniques. J Emerg Med. 2018;54(6):849-854.
- Skelley NW, Chamberlain A. Anovel reduction technique for elbow dislocations. Orthopedics 2015;38:42–4.
- Wiegand L, Bernstein J, Ahn J. Fractures in brief: Olecranon fractures. Clin Orthop Relat Res. 2012;470(12):3637-41.
Drs. Helman, Sayal and Dantzer have no conflicts of interest to declare
Now test your knowledge with a quiz.









Simple elegant Focused informative clinically relevant.
Thank you!
Excellent podcast – so helpful and will definitely improve my clinical practice.
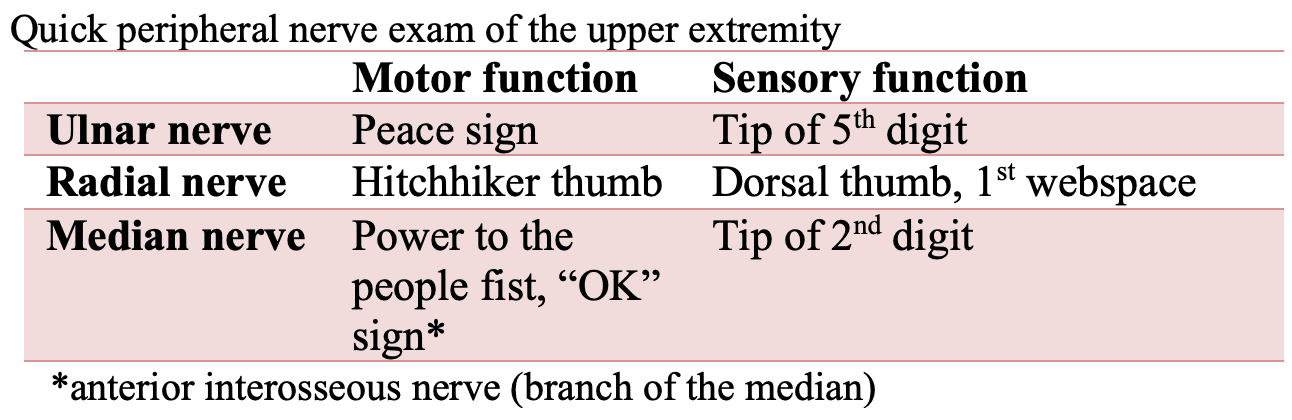
Hi, I love the easy way to test the nerves post elbow dislocation – please would you clarify how to provide resistance to demonstrate weakness e.g, for median do you ask the patient to open their fist whilst clasping it closed?