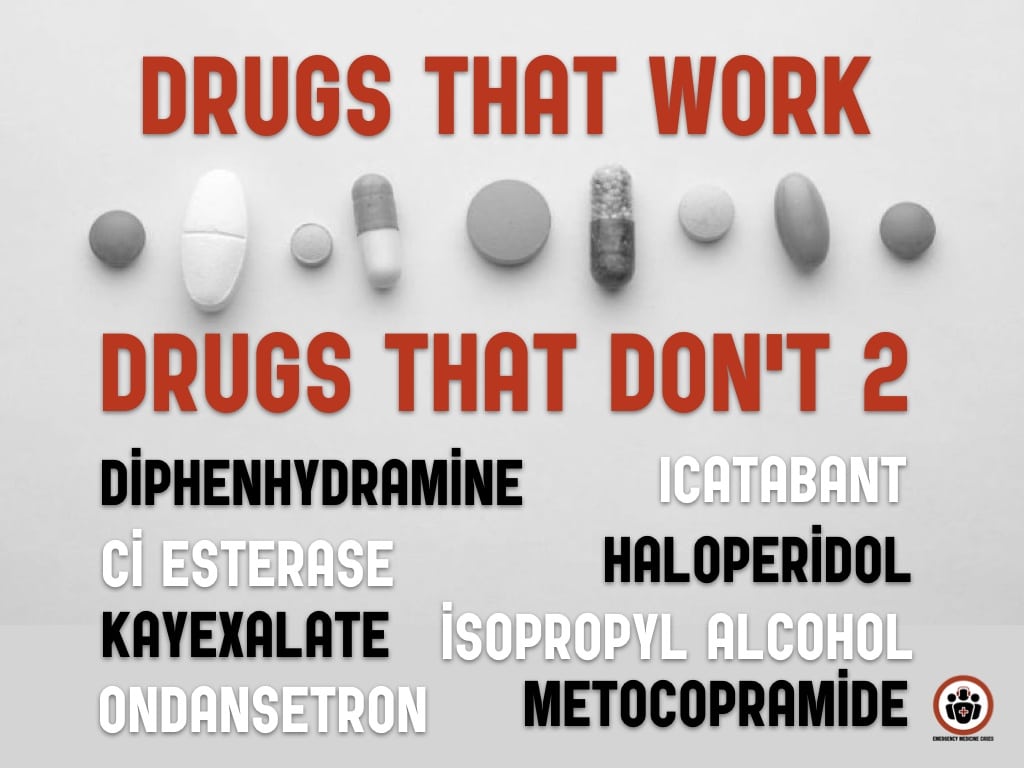
In this Episode 127 Drugs that Work and Drugs that Don’t Part 2 – Antiemetics, Angioedema and Oxygen, with Justin Morgenstern and Joel Lexchin we discuss the evidence for various antiemetics like metoclopramide, prochlorperazine, promethazine, droperidol, ondansetron, inhaled isopropyl alcohol and haloperidol as well as why should not use an antiemetic routinely with morphine in the ED. We then discuss the evidence for various drugs options for a potpourri of true emergencies like angioedema and hyperkalemia, and wrap it up with a discussion on oxygen therapy…
Podcast production, sound design & editing by Anton Helman
Written Summary and blog post by Anton Helman July, 2019
Cite this podcast as: Helman, A. Morgenstern, J. Lexchin J. EM Drugs that Work and Drugs That Don’t Part 2. Emergency Medicine Cases. July, 2019. https://emergencymedicinecases.com/em-drugs-that-work-part-2. Accessed [date]
Go to part 1 of this 2-part podcast on EM drugs that work and drugs that don’t
Antiemetics: Are they all equally effective?
A Cochrane review compared mean nausea scores at 30 minutes of metoclopramide, prochlorperazine, promethazine, droperidol, ondansetron and placebo in ED patients with nausea [1]. The only statistically significant change in baseline VAS at 30 minutes was for droperidol (which is not available in Canada), in a single trial. No other drug was statistically significantly superior to placebo. There is no definite evidence to support the superiority of any one drug over any other drug. Patients in the placebo arms often reported clinically significant improvement in nausea at 30 minutes which may reflect the cyclical nature of nausea.
If an antiemetic is used, choice of drug should be dictated by patient preference, side effects and cost. Sedation is common to all of these antiemetics except ondansetron. Don’t forget that all the antipsychotic antiemetics (prochlorperazine, promethazine, droperidol, haloperidol) can worsen Parkinsonian symptoms through their dopaminergic effects and so should be avoided in patients with Parkinson’s disease.
Is inhaled isopropyl alcohol the first line antiemetic of choice?
A Cochrane review suggests a moderate level of evidence for a significant reduction in time to 50% reduction in nausea scores (about 3 points on a 10 point scale) when comparing inhaled isopropyl alcohol (holding an alcohol swab 1-2cm below the nares and inhaling for 5 minutes) to standard antiemetics in postoperative patients with nausea, with fewer patients who received isopropyl alcohol requiring rescue antiemetics [2]. In one ED RCT, when compared to placebo normal saline solution a similar 50% reduction/3 point difference was seen at 10 minutes [3]. In another ED RCT, when comparing ondansetron 4mg po to inhaled isopropyl alcohol the mean decrease in nausea scores were about 1/10 for ondansetron and 3/10 for isopropyl alcohol, with no difference in the proportion of patients requiring rescue mediations (about 1/4) [4]. None of the trials with isopropyl alcohol inhalation found any side effects.
IV haloperidol as antiemetic for gastroparesis and cyclical vomiting syndrome
Haloperidol 5mg IV has been shown to decrease both pain scores and nausea when compared to placebo in gastroparesis [5]. Remarkably, patients in the haloperidol arm had a 27% admission rate compared to 72% in the placebo arm. Haloperidol has also been shown in case reports of patients with cannabis hyperemesis syndrome to be effective in doses ranging from 2.5mg-5mg [6].
Take home: In general, none of the traditional antiemetics (metoclopramide, prochlorperazine, promethazine, droperidol, ondansetron) are better than placebo at improving nausea scores in the first 30 minutes, while isopropyl alcohol may be better than both placebo and traditional antiemetics, with no reported side effects and very rapid administration, while saving nursing resource time. Consider IV haloperidol 2.5-5mg in patients with gastroparesis/cyclical vomiting syndrome/cannabis hyperemesis syndrome.
Routine use of antiemetic with morphine is unnecessary
Two RCT comparing metoclopramide 10g vs placebo in patients requiring morphine for acute pain in the ED showed no statistical difference incidence of nausea and vomiting, which was only 2.7-6.5% with about twice the incidence of side effects [7,8]. The nausea and vomiting associated with patients who receive morphine may have more to do with their pain rather than morphine itself. Our experts recommend treating the pain with morphine alone first, and then once pain is adequately controlled, if patients complain of nausea, only then should antiemetics should be considered. Avoid the sedating antiemetics as the combined effects of morphine plus the sedating antiemetics may lead to oversedation and/or prolonged sedation. If an antiemetic is required despite adequate pain control, ondansetron or isopropyl alcohol inhalation is preferred because of their non-sedating profile.
Take home: Antiemetics should not routinely be co-administered with morphine prophylactically for nausea. Treat the pain first and then assess for ongoing nausea. If persistent despite adequate pain control, consider a non-sedating antiemetic.
What is the preferred antiemetic for nausea and vomiting associated with vertigo?
For patients with benign positional vertigo antiemetics are not required. Instead perform the Epley or Semont maneuvers which are equally effective in resolving symptoms acutely (NNT = 2-3) according to a Cochrane review of 11 studies [9].
Antihistamines are the preferred antiemetic for persistent acute vertigo associated with nausea based on limited evidence. Two RCTs, one comparing lorazepam versus dimenhydrinate (Gravol) showed that symptoms improvement and ability to ambulate at 2 hrs were superior for dimenhydrinate [10], and another comparing betahistine (Serc) to promethazine [11] showed improved nausea scores and clinical symptoms in the betahistine arm.
For chronic vertigo, a Cochrane review of betahistine (Serc) showed a reduction in symptoms at 3 months compared to placebo [12]. Although this review did not show any significant adverse events, beware of the anticholinergic side effects and start with the lowest dose (dimenhydrinate 25mg q4h, betahistine 8mg tid).
Is there any role for icatibant, C1 esterase inhibitors or FFP for angioedema?
While there are several very small industry sponsored trials showing improved time to resolution of symptoms with icatabant vs placebo the largest multicenter, multinational RTC of 121 patients with upper airway ACE-I induced angioedema comparing icatibant vs placebo [13] showed no difference in time to meeting discharge criteria or in time to onset of symptom relief. The main adverse effects of icatibant are reactions at the injection site, which occur in almost all patients due to the large volume of solution required. The cost of icatabant is $9600 USD per injection.
C1 esterase inhibitors (berinert, cinryze, haegarda) have been shown to be effective in reducing the time to symptom resolution in hereditary angioedema when given early by 1-3 hours [14,15,16]. These medications are not available at most community hospitals in Canada and usually have to be transported to the ED, which precludes the advantages of early administration, and decisions about securing the airway usually need to be made early in the presentation. However, acute angioedema is typically a self-limited event. More importantly, these medications have never been shown to prevent airway obstruction, the need for endotracheal intubation or mortality which are arguably the only outcomes of interest in the ED. The cost of a single dose of C1 esterase inhibitor is $3000-$5000 USD.
There are no trials on the efficacy of FFP in angioedema and it’s off-label use for this indication is based on a few case reports. FFP takes time to thaw, has a significant adverse event profile and has no evidence for benefit. Our experts do not recommend the use of FFP in ED patients with angioedema.
Learn more about management of severe angioedema in EM Quick Hits 19
Take home: There is little role for icatibant, C1 esterase inhibitors or FFP in the emergency management of angioedema since they have never been shown to decrease the rate of airway obstruction, need for endotracheal intubation, or mortality and they often need to be transported from outside the ED and/or take time to thaw, long after the need to secure the airway. C1 esterase inhibitors may shorten the duration of symptoms, but their cost may be prohibitive and all of the trials were industry sponsored.
There is no role for Kayexalate in ED patients with hyperkalemia
A 2005 Cochrane review did not show any evidence that Kayexalate improves potassium levels [17]. There are multiple case reports of Kayexalate causing GI necrosis and perforation which led the FDA to issue a warning in 2011 cautioning against the use of Kayexalate [18, 19]. Our experts conclude that there is no role for kayexalate in the ED.
Learn more about hyperkalemia in Episode 86- Emergency Management of Hyperkalemia
Supplemenatal oxygen in acutely ill patients with adequate oxygen saturations may increase mortality
A metaanalysis of 8 RCTs (8000 patients) with suspected MI showed that oxygen therapy did not reduce the risk of in-hospital or 30-day mortality [20].
A metaanalysis of 13 RCTs (17000 patients) with COPD or vented ICU patients showed that normoxia was associated with a lower mortality than hyperoxia (2% vs. 9%) [21].
A systematic review of 37 studies with traumatic brain injury, stroke and sepsis showed that in all but one study, hyperoxia was associated with a higher mortality rate [22].
A systematic review and metaanalysis in Annals of Emergency Medicine in 2019 showed that hyperoxia was associated with an increased risk of in hospital mortality and 30-day mortality. The mean number needed to harm resulting in one death with hyperoxic therapy was 71 (NNH = 71) [23].
Take home: Hyperoxia has been shown in MI, stroke, sepsis, ventilated ICU patients and traumatic brain injury to be harmful and may increase mortality. The majority of critically ill patients in the ED with oxygen saturations >90-92% should not receive supplemental oxygen. There are some important exceptions such as carbon monoxide poisoning.
Resources for good quality evidence based impartial reviews of drug effectiveness
- Therapeutics Initiative
- Therapeutics Education Collaborative
- The Medical Letter
- Prescrire International
- Cochrane Reviews
Go to part 1 of this 2-part podcast on EM drugs that work and drugs that don’t
References
- Furyk JS, Meek RA, Egerton-warburton D. Drugs for the treatment of nausea and vomiting in adults in the emergency department setting. Cochrane Database Syst Rev. 2015;(9):CD010106.
- Hines S, Steels E, Chang A, Gibbons K. Aromatherapy for treatment of postoperative nausea and vomiting. Cochrane Database Syst Rev. 2018;3:CD007598.
- Beadle KL, Helbling AR, Love SL, April MD, Hunter CJ. Isopropyl Alcohol Nasal Inhalation for Nausea in the Emergency Department: A Randomized Controlled Trial. Ann Emerg Med. 2016;68(1):1-9.e1.
- Freedman SB, Ali S, Finkelstein Y. Aromatherapy Versus Oral Ondansetron for Antiemetic Therapy Among Adult Emergency Department Patients: A Randomized Controlled Trial. Ann Emerg Med. 2019;73(2):208-209.
- Roldan et al. Trial Comparing Haloperidol Combined With Conventional Therapy to Conventional Therapy Alone in Patients With Symptomatic Gastroparesis. AEM November 2017.
- Hickey J. L., Witsil J. C., Mycyk M. B. Haloperidol for treatment of cannabinoid hyperemesis syndrome. The American Journal of Emergency Medicine. 2013;31(6):1003.e5–1003.e6. doi: 10.1016/j.ajem.2013.02.021.
- Bradshaw M, Sen A. Use of a prophylactic antiemetic with morphine in acute pain: randomised controlled trial. Emerg Med J. 2006;23(3):210-3.
- Talbot-stern J, Paoloni R. Prophylactic metoclopramide is unnecessary with intravenous analgesia in the ED. Am J Emerg Med. 2000;18(6):653-7.
- Hilton MP, Pinder DK. The Epley (canalith repositioning) manoeuvre for benign paroxysmal positional vertigo. Cochrane Database of Systematic Reviews 2014, Issue 12. Art. No.: CD003162
- Marill KA, Walsh MJ, Nelson BK. Intravenous Lorazepam versus dimenhydrinate for treatment of vertigo in the emergency department: a randomized clinical trial. Ann Emerg Med. 2000;36(4):310-9.
- Motamed H, Moezzi M, Rooyfard AD, Angali KA, Izadi Z. A Comparison of the Effects and Side Effects of Oral Betahistine with Injectable Promethazine in the Treatment of Acute Peripheral Vertigo in Emergency. Journal of clinical medicine research. 2017; 9(12):994-997.
- Murdin L, Hussain K, Schilder AGM. Betahistine for symptoms of vertigo. Cochrane Database of Systematic Reviews 2016, Issue 6. Art. No.: CD010696. DOI: 10.1002/14651858.CD010696.pub2.
- Sinert R, Levy P, Bernstein JA, et al. Randomized Trial of Icatibant for Angiotensin-Converting Enzyme Inhibitor-Induced Upper Airway Angioedema. J Allergy Clin Immunol Pract. 2017;5(5):1402-1409.e3.
- Maurer M, Aberer W, Bouillet L, Caballero T, Fabien V, Kanny G, et al. Hereditary angioedema attacks resolve faster and are shorter after early icatibant treatment. PLoS ONE. 2013;8:e53773.
- Craig TJ, Levy RJ, Wasserman RL, Bewtra AK, Hurewitz D, Obtułowicz K, et al. Efficacy of human C1 esterase inhibitor concentrate compared with placebo in acute hereditary angioedema attacks. J Allergy Clin Immunol. 2009;124:801–8.
- Craig TJ, Bewtra AK, Bahna SL, et al. C1 esterase inhibitor concentrate in 1085 Hereditary Angioedema attacks–final results of the I.M.P.A.C.T.2 study. Allergy. 2011;66(12):1604-11.
- Mahoney BA et al. Emergency interventions for hyperkalemia (Review). Cochrane Data Syst Rev 2005 Issue 2.
- Rogers FB, Li SC. Acute colonic necrosis associated with sodium polystyrene sulfonate (Kayexalate) enemas in a critically ill patient: case report and review of the literature. J Trauma 2001; 51(2): 395-7.
- Bomback AS et al. Colonic necrosis due to sodium polystyrene sulfate (Kayexalate). Am J Emerg Med 2009; 27: 753.e1-e2.
- Sepehrvand N, James SK, Stub D, Khoshnood A, Ezekowitz JA, Hofmann R. Effects of supplemental oxygen therapy in patients with suspected acute myocardial infarction: a meta-analysis of randomised clinical trials. Heart. 2018;104(20):1691-1698.
- Grensemann J, Fuhrmann V, Kluge S. Oxygen Treatment in Intensive Care and Emergency Medicine. Dtsch Arztebl Int. 2018;115(27-28):455-462.
- Stolmeijer R, Bouma HR, Zijlstra JG, Drost-de klerck AM, Ter maaten JC, Ligtenberg JJM. A Systematic Review of the Effects of Hyperoxia in Acutely Ill Patients: Should We Aim for Less?. Biomed Res Int. 2018;2018:7841295.
- Gottlieb M, Goldstein C, Ward EJ. Is the Liberal Use of Oxygen Associated With Worse Outcomes Among Critically Ill Patients?. Ann Emerg Med. 2019;73(2):180-182
Drs. Helman, Morgenstern and Lexchin have no conflicts of interest to declare
Now test your knowledge with a quiz.

Hi! I’ve been an inpatient nurse for a long time, I only gave morphine IV push fast (suggested admin time) once or twice and they immediately threw up. Ever since then, I dilute it in 10 ml NS, and give slowly, pausing if they start to gag. Some people take more than 5 minutes. I’ve never had a problem with vomiting after that! After a few doses they are usually fine to give over 2-3 minutes. Has anyone studied that? Maybe for the opioid naive it needs to be given IVPB x 2 then IVP. Or slowly.
Great episode
Please keep it going!
Question about angioedema:
Do we need to keep them in the ED until symptoms completely resolved or they can be safely discharged if no airway compromise after a few hours of observation. My experience is that in some cases the symptoms last for a long time and they’re stuck in the ED for hours with no improvement.
Thank you jn advance!