Topics in this EM Quick Hits podcast
David Carr the mighty return of Carr’s Cases! (00:38)
Sarah Reid on differentiating septic arthritis from transient synovitis in pediatric limp (18:52)
Anand Swaminathan on managing tracheostomy complications in the ED (27:50)
Nour Khatib on rural medicine and ethylene glycol poisoning (37:52)
Justin Morgenstern on RCTs for ketamine in patients with severe agitation (48:17)
Podcast production, editing and sound design by Anton Helman
Written summary & blog post by Sarah Reid and Anton Helman November, 2021
Cite this podcast as: Helman, A., Swaminathan, A., Khatib, N., Reid, S., H. Carr, D., Morgenstern J. EM Quick Hits 34 – Carr’s Case, Septic Arthritis vs Transient Synovitis, Managing Tracheostomies, Ethylene Glycol Poisoning, Ketamine for Agitation. Emergency Medicine Cases. November, 2021. https://emergencymedicinecases.com/em-quick-hits-november-2021/. Accessed [date].
Pediatric nontraumatic limp – differentiating transient synovitis from acute bacterial osteoarticular infection (septic arthritis, osteomyelitis)
- Age and fever dictate differential for nontraumatic pediatric limp

Causes of non-traumatic limp by age/presence of fever
- Workup to consider:
- Xrays
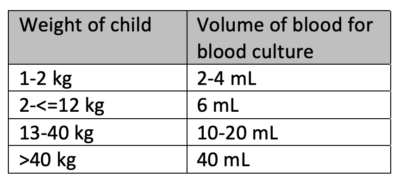
- CBCD, CRP, blood culture if infection/inflammatory cause suspected to help distinguish between transient synovitis and osteoarticular infection
- US (for effusion, soft tissues) if significant fever and/or elevation of inflammatory markers and/or severe pain
- MRI with gadolinium is the most accurate noninvasive test for osteoarticular infection and should be considered for patients with persistent pain/fever

Differentiating transient synovitis and acute bacterial osteoarticular infection
- Volume of blood matters when obtaining blood for culture and sensitivity which is essential, as hematogenous spread is common in children with osteoarticular infections
- https://www.cps.ca/documents/position/osteoarticular-infections-in-children
- Peltola H. and Paakkonen M. Acute Osteomyelitis in Children. N Engl J Med. 2014;370:352-360.
- Tu J, et al. Test characteristics of history, examination and investigations in the evaluation for septic arthritis in the child presenting with acute non-traumatic limp. A systematic review. BMJ Open 2020;10:e038088.
Approach to tracheostomy emergencies in the ED
EM Cases Best Case Ever with Scott Weingart on Tracheo-innominate Fistula
Ethylene glycol poisoning
- Ethylene glycol is a toxic alcohol found in engine coolants, cleaning products, radiator antifreeze, degreasing agents, foam stabilizers and metal cleaners that is intoxicating like ethanol
- As the alcohol (which is nontoxic itself) is metabolized to an acid (which is toxic) patients develop hypotension, tachycardia, tachypnea, depressed level of awareness, renal failure and potentially seizures. The symptoms usually develop over 6-24hrs but can be delayed up to 4 days if ethanol is coingested.
- Diagnostic clues to toxic overdose include tachycardia and tachypnea (in an attempt to blow off CO2), high anion gap metabolic acidosis with high osmolar gap, not sobering up as expected, low ethanol level in a highly inebriated patient
- Early after ingestion an anion gap metabolic acidosis has not had time to develop but osmolality is expected to be high. Later after ingestion an anion gap metabolic acidosis is expected while the osmolality may be normal. Absence of an anion gap metabolic acidosis or high osmolar gap does not rule out toxic alcohol poisoning.
- Coingestion of ethanol delays the toxic effects of ethylene glycol and can be used as an effective treatment when fomepazol antidote is not available.
- Additional treatments besides fomepazol or ethanol includes pyridoxine, correction of acidosis with a bicarbonate infusion to target pH = 7.2, and dialysis
EM Cases Episode 160 Toxic Alcohols – Minding the Gaps with Emily Austin & Margaret Thompson
Evidence for ketamine for severe agitation and excited delirium
- The first ever ED RCTs comparing ketamine to haloperidol + benzodiazepine for severely agitated patients were published in 2021
- A randomized, single ED study of 93 patients compared ketamine (4 mg/kg IM or 1mg/kg IV) and haloperidol/lorazepam (haloperidol 5-10 mg IM/IV + lorazepam 1-2 mg IV/IM) with primary outcome of time to sedation, and found ketamine was significantly more effective at both 5 minutes and 15 minutes after medication administration with no statistically significant increase in adverse effects
- Another single-centered, randomized trial of 80 patients comparing ketamine (5 mg/kg IM) and haloperidol/midazolam (5 mg for both), showed a significantly different mean time to sedation of 6 minutes for the ketamine group and 15 minutes for the haloperidol/midazolam group with no statistical difference in serious adverse events
- While there were no statistical difference in serious adverse events, there was a trend toward more adverse events in the ketamine groups
=>Ketamine may be superior to haloperidol + benzodiazepine for rapid sedation of severely agitated patients but is associated with more serious adverse events, and should be considered in selected patients in the prehospital setting when rapid sedation is perhaps more important than in the ED
- Barbic D, Andolfatto G, Grunau B, Scheuermeyer FX, Macewan B, Qian H, Wong H, Barbic SP, Honer WG. Rapid Agitation Control With Ketamine in the Emergency Department: A Blinded, Randomized Controlled Trial. Ann Emerg Med. 2021 Aug 2:S0196-0644(21)00433-9.
- Lin J, Figuerado Y, Montgomery A, Lee J, Cannis M, Norton VC, Calvo R, Sikand H. Efficacy of ketamine for initial control of acute agitation in the emergency department: A randomized study. Am J Emerg Med. 2021 Jun;44:306-311
None of the authors have any conflicts of interest to declare

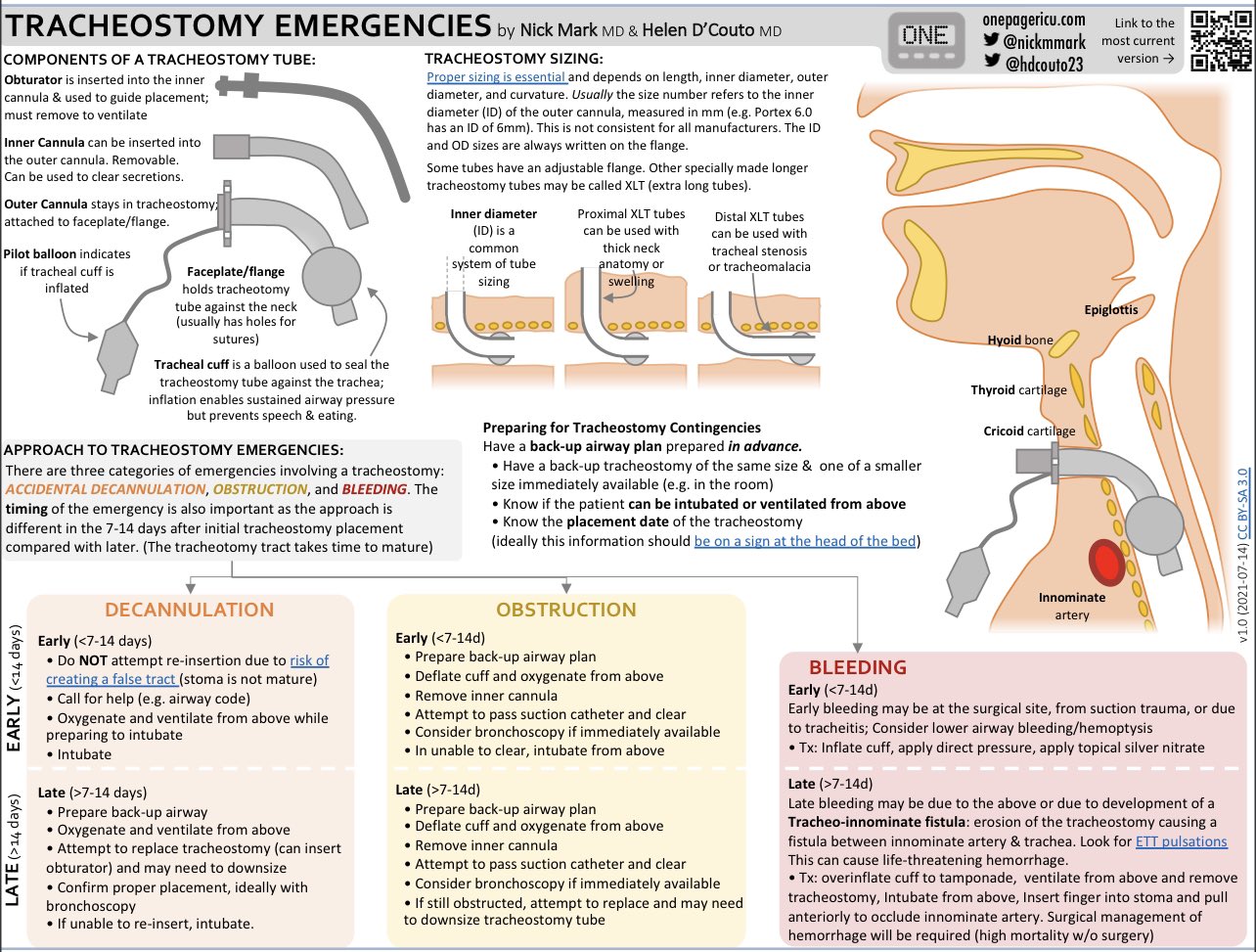



thank you. I have a question. if a patient with a trach has bleeding that has stopped and you want to rule out sentinel bleed do you have to do a ct angio? or what? also is there a time period after which it is very unlikely to be a fistula?
Don,
R/o sentinel bleed: CT angio is your go to. CT with contrast won’t be sensitive enough.
Tracheo-inomminate fistula is a “later” finding (> 1-2 weeks after placement) but can happen anytime after that so even and old trach has risk.
About Dr Carrs case
I agree on the bottom line (even though we need to cut corners, it’s good to be systematic with certain basic stuff. Always check a febrile child for petechia as Dr Carley said https://www.stemlynsblog.org/making-good-decisions-in-the-ed-rcem15/)
However I don’t think Dr Carr (or any of us who had done the same) should beat ourselves up too much in this case . Dr Carr does different things very well
– He realises that there is in indescriptancy between ECG findings and POCUS findings (ie he does not “ satishfice” with insignificant pericardial fluid being the cause , especially with a plum IVC), but goes on for more definitive diagnosis
– He realises that this patient is sick enough with the pathology found, that he follows her to the CT (…perhaps out of curiousity as well)
– He makes reasonable differentials from the pretest probability presented
And he makes a plan that “fails well” (Graceful degradation, as Kevin Fong or Chris Hadfield maybe would put it): even if he did come up with the PTX as a ddx then it would also be caught on the CT
Would I in Dr Carrs situation have done differently ?
– auscultation with stethoscope: if I heard a “negative” (ie pneumothorax?) in the context of this pretest probability (young woman , no COPD, other ddx more relevant), it would probably not shift my post test probability a whole lot (not being confident in IRR if auscultation; not good IRR on stethoscope in general etc). A little like finding a “negative” pulse in CPR has fallen out of favour , so is it the same with stethoscope in this case I believe (scepticism about IRR and Lr+/- of the stethoscope seems to have been there ever since the beginning https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1336691/)
– POCUS of lungs: yes , my next step would maybe be just that . But I’d have to weigh my ddx of other causes (I.e PE ) and the time spent trying to look for a “zebra” in this pretest probability context . This is not like looking for petechia in children with fever . This is not as onnious or likely . The CT will find both PE and PTX so why not move on to that and not delay further ? Has to be done urgent though with the pathological findings in mind (as was done)
I am a big believer in good history taking and other bedside basic skills as the most essential for us emergency physicians, along probabilistic clinical decision making skills and knowledge of cognitive biases, forcing strategies, compassionate care etc . However in this case in this context , if CT was available now , I don’t think I’d done any different .
Thanks for the humble sharing Dr Carr and re-emphasising the important basics. Sharing narratives like this contributes to the psychological safety / making vulnerability loops so that we as a community dare talk about all sorts of clinical processes (good , bad and run of the mill)
All the best
Peter , EM resident , Stockholm