In Part Two of this two-part series on hand injuries, Dr. Matt Distefano and Dr. Arun Sayal walk us through the recognition and management of common, and some not so common, hand injuries that present to the Emergency Department. Some injuries are easy to diagnose but we often fall short when managing them in the ED, while others are hard to recognize and frequently go undiagnosed. They answer such questions as: which finger tip injuries need to go to the O.R.? What is the best management strategy for nail bed lacerations? What is the tip and slip method for reduction of PIP dislocations that are difficult to reduce? How are proximal metacarpal fractures similar to Lisfranc injuries and easy to miss? How is a Rolando fracture different to a Bennet fracture? Which volar tendon lacerations should we consider repairing in the ED? and much more…
Podcast production, sound design & editing by Anton Helman; voice editing by Braedon Paul
Written Summary and blog post by Ian Beamish and Kate Dillon, edited by Anton Helman February, 2023
Cite this podcast as: Helman, A. Distefano, M. Sayal, A Episode 179 Hand Injuries – Finger Tip Injuries, Jersey Finger, Finger Dislocations, Metacarpal Fractures, Thumb Injuries, Tendon Lacerations. Emergency Medicine Cases. February, 2023. https://emergencymedicinecases.com/hand-injuries-finger-tip-injuries-jersey-finger-pip-dislocations-metacarpal-fractures-thumb-injuries-tendon-lacerations. Accessed April 28, 2024
Finger-tip injuries – avulsions, amputations and tuft fractures
Finger tip avulsions and amputations
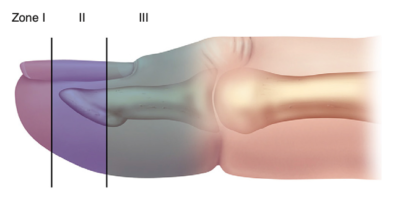
Finger tip avulsions/amputations are classified into Zone I, II, or III which each require specific management.
Zone I – No exposed bone. Management principle is ‘less if more’ and includes basic wound care, non-adherent bulky dressing (avoid dressing that are too tight that may lead to ischemia) and follow-up in 7 days. Heals by secondary intention. Complete return of sensation may take up to 18 months.
Zone II – Bone exposed and often associated with tuft fractures. Basic wound care, debridement of devitalized tissue to 1mm below the level of the soft tissue laceration, non-adherent bulky loose dressing and follow-up in 7 days. May heal by secondary intention – apply absorbable sutures only if obvious viable flap that can be closed without tension. Empiric antibiotics may be indicted in the case of a patient with comorbidities.
Zone III – between the DIP and tuft that includes the insertion of the FDP, insertion of extensor tendon, germinal matrix and nail fold, that may require distal phalanx amputation. Decision to rongeur bone and close in the ED should be guided by clinician familiarity with the procedure and hand surgeon availability, but these almost always require specialist referral.
Volar pad involvement: Finger tip amputations that involve a significant proportion of the volar pad are high risk injuries. Significant injuries of volar pad should be management by a plastic surgeon as future sensation of the finger tip is at risk.
Pitfall: a common pitfall is approximating the skin of a finger tip avulsion injury with sutures when there is a great deal of tension on the skin when closed; this does not allow for adequate healing and may cause ischemic injury; rather, healing by secondary intention is indicated for all finger tip avulsions where approximating the skin would place significant tension on the tissues.
Pearl: Use rongeurs to trim bone 1mm below level of soft tissue laceration to decrease risk of osteomyelitis that may occur with exposed bone.
Pearl: Any Zone II-III injuries with significant involvement of the volar pad will need sugery in the O.R. and possible shortening down to the DIP to preserve function
Pitfall: a common pitfall is neglecting to apply an adequate amount of petroleum jelly or antibiotic ointment and/or ointment impregnated dressings to a finger tip avulsion or amputation injury; if a dry dressing only is applied more tissue may be lost when attempts at removing the dressing occur in follow up.
It is important to educate patients that finger tip sensation typically takes 12-18 months to return after a finger tip avulsion/amputation.
Nail bed lacerations and tuft fractures – which ones need to be repaired and reduced?
A nailbed laceration should be suspected in the presence of a subungual hematoma or comminution/displacement of the distal phalanx. Remove the nail to repair the nail bed only if there is a large subungual hematoma >50% of the nail and the nail is partially avulsed and the distal phalanx is displaced.
Tuft fractures that are displaced on the dorsal surface require reduction in the ED.
The lateral x-ray is key: if there is a malalignment of the dorsal surface of the distal phalynx, that fracture requires reduction and likely nailbed repair
Pearl: Splint the nailbed either with the patient’s own nail or foil from a suture package sutured under the nail fold to ensure that the germinal matrix remains open and protected. Video for nailbed laceration repair technique using foil from a suture package: https://www.youtube.com/watch?app=desktop&v=H1sOZ9J1bEw
Seymour Fracture – a high risk pediatric finger tip injury
A Seymour fracture is a physeal fracture of the distal phalanx in children with associated nail bed injury, high risk of complications, that requires open reduction and pinning with nailbed repair. The key diagnostic clue is the nail plate lying superficial to the eponychial fold. X-rays may show widening of the physis or obvious displacement.
Mallet finger
A mallet finger involves a torn or avulsed extensor tendon. Most mallet fingers can be treated with simple extension in a DIP splint. Mallet fingers that involve a fracture or subluxation of the DIP may require surgery.

Mallet finger of RD3
Ensure DIP is held in extension by a finger splint and counsel patients on the need to maintain in splint 24×7.
The Rule of 6’s for timing of splint application in patients with mallet fingers: splint in extension for 6wks 24×7, then 6wks only during sleep, and it typically takes 6 months to return to normal function.
Pitfall: a common pitfall is failing to obtain an x-ray and refer a patient with a mallet finger with displaced avulsion fractures or subluxation of the distal phalanx as these typically require surgery to maintain the ROM of the DIP
Pearl: Rule of 6’s – splinted in extension for 6wks 24×7, then 6 wks. overnight and will take 6 months to return to normal function.
Jersey finger
A jersey finger involves an avulsed flexor digitorum profundus (FDP) classically of the 4th digit as a result of grabbing onto a jersey in sports.

Image Source: Case courtesy of Francis Deng, Radiopaedia.org, rID: 71785
- Examine for abnormal cascade of the fingers with extension of the affected DIP, and for DIP swelling, volar DIP tenderness
- Rule out a fracture or dislocation on x-rays
- Immobilize in a dorsal hand splint and a wrist splint to maintain the hand in the intrinsic minus position (see part one of this series for proper splint application)
- Refer to a hand surgeon for tendon repair within 7-14 days
PIP dislocations: Volar plate injuries and volar dislocations are high risk
The most common finger dislocation is at the PIP, most often dorsal. Most dorsal dislocations can be reduced with “tip + slip” method with wrist flexion. Dorsal dislocations are sometimes associated with avulsion fractures off the base of the middle phalanx on the volar aspect which indicates a volar plate injury which are high risk injuries. Volar plate injuries as well as PIP dislocations with post-reduction instability require referral to a hand surgeon. Volar dislocation may be associated with central slip injury/tear and can lead to Boutonniere’s deformity and therefore should have follow up with a hand specialist.

Boutonniere deformity
Metacarpal fractures – proxmial, shaft and neck fractures
Proximal metacarpal fractures are easy to miss due to bone overlap
Think of proximal metacarpal fracture as the Lisfranc injury of the hand. They are easy to miss due to bone overlap on the x-ray. These are usually minimally displaced and may be comminuted.
Pearl: think of proximal metacarpal fracture as the Lisfranc injury of the hand – they are easy to miss and they may have poor outcomes when missed
Pitfall: a common pitfall in assessment of a proximal metacarpal fracture is to miss an associated dislocation of adjacent MCP, so always check alignment on the lateral x-ray
Metacarpal shaft Fractures – malrotaion is easy to miss
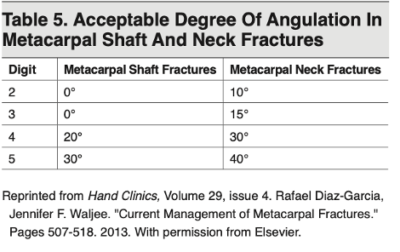
Metacarpal fractures with malrotation or scissoring, simply assessed by abnormal cascade and abnormal orientation of the finger with slow making of a fist (all fingers should point toward the scaphoid), requires surgery.
Risk of compartment syndrome if 2+ fractures due to high energy mechanism.
Metacarpal neck fractures – the Boxer’s fracture
Indications for reduction of metacarpal shaft and neck fractures
Pearl: a proximal wrist regional nerve block is a good analgesic option for reduction of metacarpal fractures as it avoids the distortion of anatomy (making the reduction of the fracture more difficult) that occurs with a hematoma block.
Pitfall: failure to assess for malrotation/scissoring both pre-reduction and post-reduction is a common pitfall.
Metacarpal fractures immobilization – immobilize metacarpal 3,4,5 fractures with a deep ulnar gutter splint and metacarpal 1,2 with a deep radial gutter.
Thumb injuries – skier’s thumb, Bennett fractures and Rolando fractures
Skier’s Thumb
Skier’s thumb is an acute avulsion or tear of the ulnar collateral ligament (UCL) of the first metacarpophalangeal joint caused by hyperabduction of the thumb, typically when a person falls while holding a pole or stick in sports. Repetitive stress can also cause chronic injury that presents as laxity of the ligament called a Gamekeeper’s Thumb.

Skier’s thumb – rupture of the ulnar collateral ligament

Skier’s thumb showing a subtle avulsion fracture at the 1st MCP
Assessing for thumb UCL instability on physical exam is essential in making this diagnosis:
UCL injury grading:
- Grade 1 = stretch, non-operative
- Grade 2 = partial tear, non-operative
- Grade 3 = complete tear, least painful, associated with Stener lesion, usually operative
Stener Lesion: adductor aponeurosis slips in between the torn end of the UCL and the MCP

Image Source: Case courtesy of Frank Gaillard, Radiopaedia.org, rID: 7641
Pearl: ensure slight adduction of thumb when placing the thumb spica splint for skier’s thumb to reduce stress on the UCL
Bennet Fracture
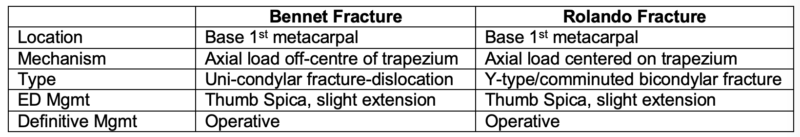
A Bennet fracture is an intra-articular fracture of the 1st metacarpal fracture caused by an axial force applied to the thumb in flexion, that requires surgical fixation when displaced.

Image Source: Case courtesy of Leonardo Lustosa, Radiopaedia.org, rID: 98585 Case courtesy of Mohammad Osama Hussein Yonso, Radiopaedia.org, rID: 98747

Image Source: Case courtesy of Leonardo Lustosa, Radiopaedia.org, rID: 98585 Case courtesy of Mohammad Osama Hussein Yonso, Radiopaedia.org, rID: 98747

Image Source: Case courtesy of Leonardo Lustosa, Radiopaedia.org, rID: 98585 Case courtesy of Bruno Di Muzio, Radiopaedia.org, rID: 56755
Rolando Fracture
Rolando fracture is a three-part or comminuted intra-articular fracture-dislocation of the base of the proximal first metacarpal. It can be thought of as a comminuted Bennet Fracture that splits the bone like an axe splitting wood. Like the Bennet fracture, a Rolando fracture is caused by an axial force applied to the thumb in flexion. Rolando fractures are unstable fractures that require surgical fixation.

Image Source: Case courtesy of Leonardo Lustosa, Radiopaedia.org, rID: 98585 Case courtesy of Bruno Di Muzio, Radiopaedia.org, rID: 56755
Pearl: assess for compartment syndrome in the thenar eminence in patients with both Bennet and Rolando fractures as they are high energy mechanisms and tend to bleed
Tendon lacerations of the hand
Explore every wound thoroughly for foreign bodies. This may entail extending the wound with sharp dissection to ensure you can see the tendon through its full excursion.
Pitfall: not inspecting underlying tendons through full range of motion to ensure you catch partial tears that may be hidden when the hand is in rest position
Danger zones for tendon lacerations
- Dorsum of the hand where tendons lie close to the surface of the skin
- Palm of the hand, proximal to the MCP, where superficial and deep palmar arches present high risk of vascular injury
Expert recommendations
- Consider ED repair of flexor tendon lacerations distal to DIP when both stumps are visible
- Consider ED repair of extensor tendon lacerations whenever both stumps are visible and there is not significant loss of surrounding tissue
- Use a taper needle, not a cutting needle, when suturing tendons
- Use a strong absorbable braided suture that lasts 8 weeks
- The Kessler, or modified Kessler technique for tendon repairs is the preferred method (see video below)
Pearl: Consider taking a photo of the tendon laceration pre/post repair on the patient’s phone for them to show the specialist at follow-up. You could save them from opening the wound again to inspect your work.
Pearl: All tendon lacerations should be splinted from the fingertips to the elbow to ensure the proximal stump does not retract
Drs. Helman, Distefano and Sayal have no conflicts of interest to declare
Now test your knowledge with a quiz.





Leave A Comment