In anticipation of EM Cases Episode 109 Recognition and Management of Skin and Soft Tissue Infections with Melanie Baimel and Andrew Morris we have Dr. Morris telling us his Best Case Ever of a nurse that he worked with diagnosed with Necrotizing Fasciitis. We discuss some of the diagnostic pearls for this difficult diagnosis as well as issues around privacy when health care workers become patients at their hospital.
Podcast production, editing and sound design by Anton Helman
Blog post by Anton Helman, April 2018
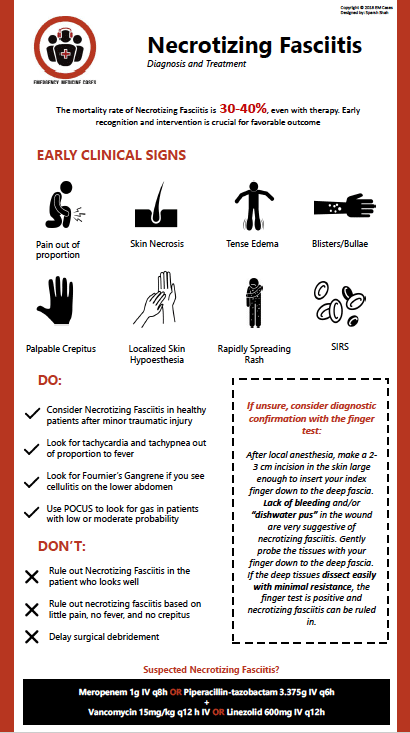
There is no set of clinical findings, lab test results and even imaging that can definitively rule out necrotizing fasciitis – an infection of the deep soft tissues that rapidly spreads along fascial planes and carries a mortality of 30-40%, even with therapy. If you have anything more than the slightest suspicion based on your clinical exam, consider early consultation with a plastic surgeon and start empiric antibiotics. While lab findings and imaging findings can be supportive of the diagnosis, negative lab and imaging studies cannot rule out necrotizing fasciitis and should never override clinical judgment. When lab tests and imaging are noncontributory, the diagnosis can only be made with surgical exploration. Necrotizing fasciitis may appear like cellulitis, but alternatively may have little if any redness. Skin findings may be scant as these skin findings represent “the tip of the iceberg” of the tissue destruction in the deep tissues. Streaking lymphangitis favours the diagnosis of cellulitis over necrotizing fasciitis.
Clues to early detection of necrotizing fasciitis
- Severe pain out of proportion to physical exam findings (however a minority of patients will report little pain and may have a laisser-faire
attitude toward their illness) - Ecchymoses or skin necrosis
- Tense edema (skin may feed hard or “wooden”)
- Bullae/blisters
- Palpable crepitus (often absent if bacteria is not gas producing)
- Localized skin hypoesthesia (due to local nerve destruction)
- Rapidly spreading rash over hours
- SIRS (may develop rapidly – monitor your patient carefully)
Necrotizing Fasciitis Pitfalls in Diagnosis
- Assuming no necrotizing fasciitis in the patient who looks well. Remember that early detection of nec fasc is the key to a favorable outcome.
- Ruling out necrotizing fasciitis based on little pain, no fever and no crepitus.
- Delay to surgical debridement – doing an extensive workup in clinically obvious cases with CT/MRI etc leading to a delay to definitive surgical treatment.
Necrotizing Fasciitis Pearls in Diagnosis
- Even though diabetes and being postoperative are often cited as risk factors, necrotizing fasciitis can occur in otherwise healthy patients after a minor traumatic injury.
- Scrutinize the vitals – most patients will have tachycardia and/or tachypnea out of proportion to fever.
- If you see what appears to be a cellulitis on the lower abdomen examine the perineum for signs of Fournier’s Gangrene.
- Use POCUS to look for gas in patients with low or moderate probability – if you see gas your suspicion for nec fasc should be significantly raised.
The finger test for diagnosis of necrotizing fasciitis
In the event that you don’t have slam dunk diagnosis of necrotizing fasciitis clinically (low pretest probability but still a suspicion) and you can’t get rapid access to surgical exploration in the OR or confirmatory imaging for whatever reason, or that the imaging is negative but you still have a suspicion for the diagnosis, consider diagnostic confirmation with the finger test. After local anesthesia, make a 2-3 cm incision in the skin large enough to insert your index finger down to the deep fascia. Lack of bleeding and/or “dishwater pus” (grey-colored fluid) in the wound are very suggestive of necrotizing fasciitis. Gently probe the tissues with your finger down to the deep fascia. If the deep tissues dissect easily with minimal resistance, the finger test is positive and necrotizing fasciitis can be ruled in.
Empiric antibiotic therapy for suspected Necrotizing Fasciitis
Meropenem1 g IV q8h OR Piperacillin-tazobactam 3.375 g IV q6h
PLUS Vancomycin 15 mg/kg q12 h IV OR Linezolid 600 mg IV q12h
References
Puvanendran R, Huey JC, Pasupathy S. Necrotizing fasciitis. Can Fam Physician. 2009;55:(10)981-7.
Castleberg E, Jenson N, Dinh VA. Diagnosis of Necrotizing Fasciitis with Bedside Ultrasound: the STAFF Exam. West J Emerg Med. 2014;15(1):111-113.
Lille ST, Sato TT, Engrav LH, Foy H, Jurkovich GJ. Necrotizing soft tissue infections: Obstacles in diagnosis. J Am Coll Surg. 1995. 182(1):7-11.
Childers BJ, Potyondy LD, Nachreiner R, et al. Necrotizing fasciitis: a fourteen-year retrospective study of 163 consecutive patients. Am Surg. 2002 Feb. 68(2):109-16.
Goh T, Goh LG, Ang CH, Wong CH. Early diagnosis of necrotizing fasciitis. Br J Surg. 2014 Jan;101(1):e119-25.
Kwak YG, Choi SH, Kim T, et al. Clinical Guidelines for the Antibiotic Treatment for Community-Acquired Skin and Soft Tissue Infection. Infect Chemother. 2017;49(4):301-325.
Other FOAMed Resources on Necrotizing Fasciitis
emDocs on misdiagnosing necrotizing fasciitis
emDocs on necrotizing fasciitis pearls and pitfalls
LiTFL bullet points review on necrotizing fasciitis





I’ve not heard of the “finger test” before. Sounds aggressive, and would surgeons be convinced by this?