This month’s EM Cases Best Case Ever podcast features Dr. Catherine Varner, Emergency Physician at Sinai Health System and researcher at Schwartz-Reisman Emergency Medicine Institute (SREMI) discussing the key pitfalls in the diagnosis of ectopic pregnancy and ruptured ectopic pregnancy. It turns out that we’re missing the diagnosis more than we’d like to admit. Dr. Varner debunks much of the traditional teaching around ectopic pregnancy so that we can improve our diagnostic skills for this potentially life threatening diagnosis…
Podcast production, editing and sound design by Anton Helman
Written by Anton Helman April, 2018
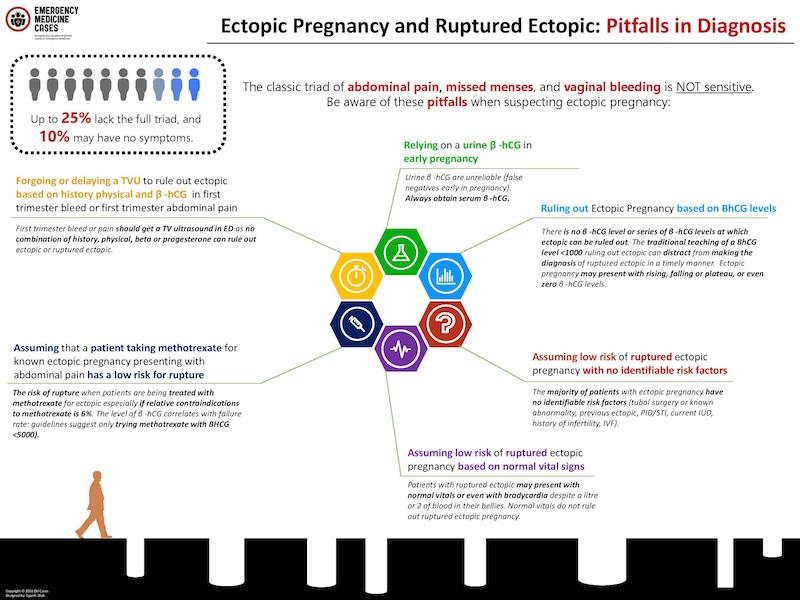
Ectopic Pregnancy and Ruptured Ectopic: Pitfalls in Diagnosis
- Ruling out ectopic pregnancy based on BhCG level. There is no BhCG level or series of BhCG levels at which ectopic can be ruled out. The traditional teaching of a BhCG level <1000 ruling out ectopic can distract from making the diagnosis of ruptured ectopic in a timely manner. Ectopic pregnancy may present with rising, falling or plateau, or even zero β -hCG levels.
- Relying on a urine BhCG in early pregnancy. Urine BhCG are unreliable (false negatives early in pregnancy). Always obtain serum BhCG.
- Assuming low risk of ectopic pregnancy in a patient with no identifiable risk factors. The majority of patients with ectopic pregnancy have no identifiable risk factors (tubal surgery or known abnormality, previous ectopic, PID/STI, current IUD, history of infertility, IVF).
- Assuming low risk of ruptured ectopic pregnancy based on normal vital signs. Patients with ruptured ectopic may present with normal vitals or even with bradycardia despite a litre or 2 of blood in their bellies. Normal vitals do not rule out ruptured ectopic pregnancy.
- Assuming that a patient taking methotrexate for known ectopic pregnancy presenting with abdominal pain has a low risk for rupture. The risk of rupture when patients are being treated with methotrexate for ectopic esp if relative contraindications to methotrexate (6% failure rate – level of BhCG correlates with failure rate – guidelines suggest only trying methotrexate with BHCG <5000).
- Forgoing or delaying a transvaginal ultrasound to rule out ectopic based on history physical and BhCG in first trimester bleed or first trimester abdominal pain. T1 bleed or pain should get a TV ultrasound in ED as no combination of history, physical, beta or progesterone that can rule out ectopic or ruptured ectopic.
Update 2021: Retrospective, cohort review of 109 patients admitted for operative management of newly diagnosed ectopic pregnancy. Use of point-of-care ultrasound (POCUS) showed shorter length of stay in ER and faster time to OR for ruptured ectopic when compared to radiology-based ultrasound alone. Abstract
References for Ectopic Pregnancy and Ruptured Ectopic Pregnancy
Murray H, Baakdah H, Bardell T, Tulandi T. Diagnosis and treatment of ectopic pregnancy. CMAJ. 2005;173(8):905-12.
Elson CJ, Salim R, Potdar N, Chetty M, Ross JA, Kirk EJ on behalf of the Royal College of Obstetricians and Gynaecologists. Diagnosis and management of ectopic pregnancy. BJOG 2016;.123:e15–e55.
Other FOAMed Resources on Ectopic Pregnancy and Ruptured Ectopic Pregnancy
emDOCs reviews ectopic pregnancy
EM Cases main episode on Vaginal Bleeding in Early Pregnancy




Supposedly paradoxical bradycardia has been reported due to blood in douglas’ pouch.
[…] Dr. Catherine Varner’s Best Case Ever reviewing 6 pitfalls in diagnosis of ectopic pregnancy […]