This is ‘Alcohol Withdrawal and Delirium Tremens: Diagnosis and Management‘ on EM Cases.
Alcohol withdrawal is everywhere. We see over half a million patients in U.S. EDs for alcohol withdrawal every year. Despite these huge volumes of patients and the diagnosis of alcohol withdrawal seeming relatively straightforward, it’s actually missed more often than we’d like to admit, being confused with things like drug intoxication or sepsis. Or it’s not even on our radar when an older patient presents with delirium. The differential diagnosis is enormous – and no blood test on the planet will help us diagnose alcohol withdrawal. In fact, the diagnosis is entirely a clinical one. What’s even more surprising is that even if we do nail the diagnosis, observational studies show that, in general, alcohol withdrawal is poorly treated. There’s several reasons for our all too often mismanagement of these patients: few EDs have a standardized approach (or training of an approach) to the management of alcohol withdrawal, there’s unfortunately still a bit of a stigma associated with alcoholism in many EDs which may contribute a kind of indifference to these patients by ED staff, and the medications used to treat alcohol withdrawal are often dosed incorrectly. So what if alcohol withdrawal is missed or poorly treated? Well, mismanaged alcohol withdrawal can be fatal – and untreated severe withdrawal often ends up with your patient seizing, or maybe progressing to delirium tremens.
To help you become masters of alcohol withdrawal management, our guest experts on this podcast are Dr. Bjug Borgundvaag, an ED doc and researcher with a special interest in emergency alcohol related illness and the director of Schwartz-Reismann Emergency Medicine Institute, Dr. Mel Kahan, an addictions specialist for more than 20 years who’s written hundreds of papers and books on alcohol related illness, and the medical director of the substance use service at Women’s College Hospital in Toronto, and Dr. Sara Gray, an ED-intensivist at St. Michael’s Hospital, an inner city hospital that sees high volumes of alcohol related illness.
Written Summary and blog post written by Keerat Grewal, edited by Anton Helman October, 2016
Cite this podcast as: Helman, A, Borgundvaag, B, Gray, S. Alcohol Withdrawal and Delirium Tremens: Diagnosis and Management. Emergency Medicine Cases. October, 2016. https://emergencymedicinecases.com/alcohol-withdrawal-delirium-tremens/. Accessed [date].
General Approach to the Management of Patients with Alcohol Withdrawal
The ideal management of alcohol withdrawal involves 4 steps:
- Identify which patients actually have alcohol withdrawal and require treatment
- Use a standardized, symptom guided approach to assess symptom severity and guide treatment
- Ensure that patients are fully treated prior to ED discharge
- Provide a pathway to support patients who are trying to quit
Step 1: Identify which patients actually have alcohol withdrawal and require treatment
Alcohol withdrawal is a clinical diagnosis and a diagnosis of exclusion. The tremor of alcohol withdrawal is central to the diagnosis. It is important to understand the key features of alcohol withdrawal tremor. The characteristic tremor is an intention tremor: at rest there is no tremor, but when you ask the patient to extend their hands or arms you will see a fine motor tremor (typically 7-12Hz) that is constant and does not fatigue with time. Other symptoms associated with alcohol withdrawal include: gastrointestinal upset, anxiety, nausea/vomiting, diaphoresis, tachycardia, hypertension and headache.
PEARL: A tongue tremor (as in this video) is difficult to feign and is a more sensitive sign of alcoholic tremor than hand tremor
PEARL: The 3 characteristics of alcohol withdrawal hand tremor are that it is an intention tremor, it is constant and it does not fatigue.
Step 2: Use a standardized, symptom-guided approach to assess symptom severity and guide treatment
Protocols for treating alcohol withdrawal standardize care, they ensure clinicians identify the appropriate symptoms and monitor treatment. Protocols for alcohol withdrawal have been shown to improve the quality and consistency of care patients receive.
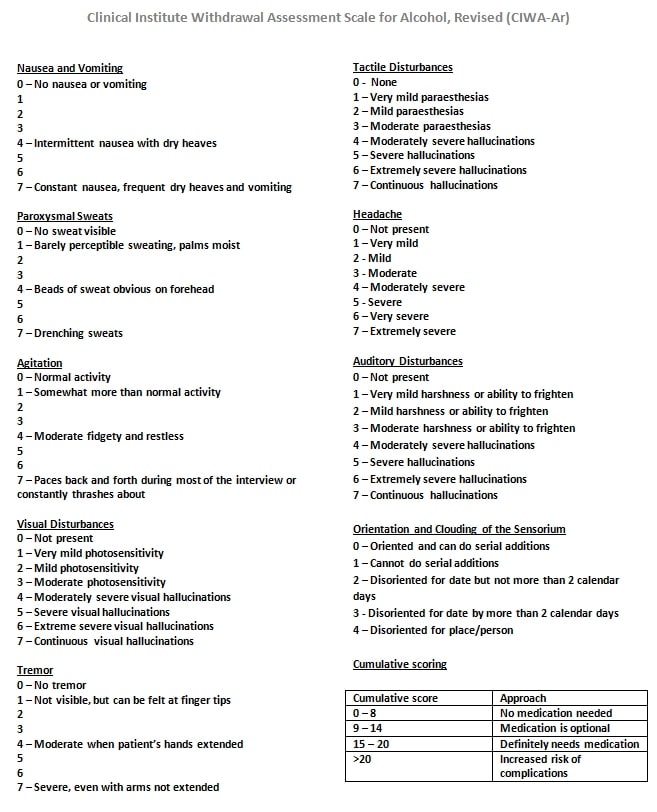
The CIWA protocol is a 10-item scale. It has been well validated in patients with alcohol withdrawal, but should not be used for patients with delirium tremens. The CIWA calls for patients to be assessed hourly and treated if the total score is 10 or greater. When 2 sequential scores are < 10 they may be considered for discharge.
CIWA on MDCalc Here
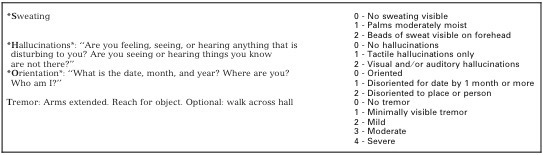
The SHOT protocol is a shorter protocol that has recently been developed by our guest experts which may be easier to implement in the ED. It is a 4-item scale (Sweating, Hallucinations, Orientation and Tremor) that correlated well with the CIWA score and takes ~ 1 minute to apply. The SHOT protocol has not yet been validated.
Step 3: Ensure that patients are fully treated prior to ED discharge
Observational studies show that patients are often either undertreated resulting in complications of alcohol withdrawal such as seizures and delirium tremens, or oversedated leading to prolonged length of stay and airway complications. If a patient has two sequential CIWA scores < 10 two hours apart, and there are no concerning risks for deterioration, consider discharging the patient from the ED. The patient’s tremor should be minimal or resolved before discharge regardless of the CIWA score.
Pitfall: Patients with a CIWA score <10 yet still have a severe alcohol withdrawal tremor are at risk of complications of alcohol withdrawal if discharged from the ED.
The CIWA-Ar is only intended to allow assessment of withdrawal severity once the diagnosis has been made. It is not a diagnostic test for withdrawal.
It is strongly discouraged that patients be provided a take-away supply or prescription for benzodiazepines. The long half-life of diazepam will protect patients from developing serious symptoms of withdrawal, and if adequately treated in the ED, no additional medications will be required.
Pitfall: Patients who are discharged from the ED with a prescription for benzodiazepines are put at increased risk for sedative overdose, drug seeking behaviour and drug dependence.
Step 4: Provide a pathway to support patients who are trying to quit
Most patients in the ED with alcohol withdrawal are there to seek help. They are in a vulnerable state and may be ready to quit drinking. This is an opportune time for them to take the first steps on the pathway to recovery. Dr. Kahan recommends counselling all ED patients who you have treated for alcohol withdrawal about the following to maximize their chances of seeking help:
- You need help for your serious alcohol problem
- You can’t do it on your own
- There are effective treatments available to you
- With treatment the way you feel, your mood, social relationships and work will be profoundly better
Provide several options to the patient, if available (i.e., AA, local treatment programs).
Timing of Alcohol Withdrawal and Delirium Tremens
Symptoms from alcohol withdrawal usually start within 6-8 hours after the blood alcohol level decreases, peak at 72 hours, and diminish by days 5 to 7 of abstinence. Delirium Tremens can occur anytime from 3 to 12 days after abstinence.
Patients who are severely dependent on alcohol become tolerant to alcohol and their nervous systems have been reset to compensate for the sedating effects of alcohol. The likelihood of developing withdrawal is dependent on the usual amount consumed and the duration of consumption. Therefore, patients who consume large amounts of alcohol on a regular basis are more likely to develop withdrawal requiring pharmacologic management compared to those who binge sporadically.
Investigations for Patients with Alcohol Withdrawal
Ethanol Level in patients with alcohol withdrawal
A serum ethanol level should be considered only if the history is inconsistent or you are unsure of the diagnosis. Even then, there is no single ethanol level at which withdrawal is impossible. Chronic alcohol users may experience alcohol withdrawal at serum ethanol levels that are intoxicating to the naïve drinker.
Blood work in patients with alcohol withdrawal
In mild cases of withdrawal, blood work is rarely helpful and is unlikely to change management. However, in patients with severe alcohol withdrawal, especially patients with delirium tremens, blood work can help rule out other causes of delirium, screen for alcoholic ketoacidosis and electrolyte abnormalities.
ECG in patients with alcohol withdrawal
There is some evidence to suggest that patients in severe alcohol withdrawal are at risk for prolonged QT which may be at least partially a result of the associated electrolyte abnormality such as hypomagnesemia. Consider a baseline ECG in patients who require admission for alcohol withdrawal.
Urine Drug Screen in alcohol withdrawal
A urine drug screen rarely changes management if there are no signs of co-ingestions. In a patient suspected to be in alcohol withdrawal who has delirium, or you suspect a concurrent toxidrome, a urine drug screen may be helpful.
Differential Diagnosis of Alcohol Withdrawal and Delirium Tremens
First, some patients with alcohol intoxication can have some of the signs of alcohol withdrawal (tachycardia, elevated BP, diaphoresis, agitation), so assuming that they are in withdrawal and giving them high doses of benzodiazepines can lead to complications of oversedation. Be sure to examine for tremor carefully. If they don’t have a true withdrawal tremor then they are probably drunk and not in withdrawal.
Pitfall: Some patients with alcohol intoxication can have some of the signs of alcohol withdrawal (tachycardia, elevated BP, diaphoresis, agitation), and assuming that they are in withdrawal and giving them high doses of benzodiazepines can lead to complications of oversedation.
Next, it is important to complete a neurological exam and look for any signs of head injury in patients with alcohol intoxication or withdrawal. Patients with a history of alcohol abuse are at a higher risk for head injury and intracranial hemorrhage as many of them have coagulopathies related to liver disease and fragile intracranial bridging veins from cerebral atrophy. Have a low threshold to obtain a CT head to rule out a bleed if there are signs or suspicion of a head injury.
In patients who are suffering from delirium, keep a broad differential diagnosis including infection, other toxidromes (sympathomimetics, anticholinergics, toxic alcohols), serotonin syndrome, NMS, hypertensive crisis, acute pain and thyrotoxicosis.
Pharmacologic Treatment of Patients with Alcohol Withdrawal
Benzodiazepines for Alcohol Withdrawal
The first line medication for treating patients with alcohol withdrawal is benzodiazepines. The drug of choice is diazepam because it has a long half-life of ~100 hours, and carries a decreased risk of developing serious withdrawal symptoms once the patient is discharged. Diazepam also has a faster onset of action than lorazepam. It is important to remember that diazepam should be avoided in patients with overt liver failure or a history of liver failure.
The half life of lorazepam is ~8-12 hours, which puts patients at risk of developing withdrawal symptoms once the patient is discharged and the lorazepam has worn off. However, lorazepam should be considered if there is evidence of significant liver dysfunction. If patients are encephalopathic or pre-encephalopathic lower the dose and titrate medications slowly.
Use oral benzodiazepines in stable patients with mild withdrawal who are not vomiting. Use IV benzodiazepines allowing faster onset and easier titration in patients with severe withdrawal as these patients are at a higher risk of seizure.
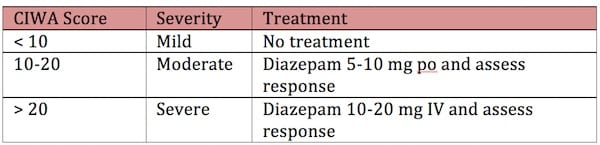
Dosing of Benzodiazepines in Alcohol Withdrawal
Dose benzodiazepines according to the severity of the alcohol withdrawal:
Another protocol to consider for patients with severe withdrawal is to give a first dose of diazepam 10mg IV, and repeat in 5 minutes if the response is not adequate. Then double the dose to 20 mg and continue with 20mg, 30mg, 30mg, 40mg, 40mg every 5 minutes as needed.
Example diazepam dosing guide for severe withdrawal (care of First 10EM)
Phenobarbital for Treatment of Alcohol Withdrawal
There is no evidence that phenobarbital is superior to benzodiazepines for preventing complications of alcohol withdrawal. There is debate regarding the equivalency of phenobarbital and benzodiazepines. Our experts do not recommend using phenobarbital alone for treatment of alcohol withdrawal, but consider its use as an adjunct with benzodiazepines after the patient has received the equivalent of 200mg of diazepam and is still in severe withdrawal.
Thiamine
Often patients with alcohol withdrawal receive 100 mg of thiamine in the ED although the evidence for any benefit is weak. If there is concern of Wernicke’s encephalopathy (nystagmus, ataxia, confusion), higher doses of thiamine are recommended (i.e. 500 mg IV q8h).
Fluids
Patients withdrawing from alcohol are almost always hypovolemic, many of these patients are also hypoglycemic. These patients should receive glucose-containing fluids. Glucose and thiamine compete for the same co-factor, therefore, there is a theoretical risk that giving glucose in a thiamine deficient patient can precipitate Wernicke’s encephalopathy. However, there is no evidence that one dose of glucose in a thiamine-deficient patient will precipitate Wernicke’s. If you give glucose, give it at the same time or after thiamine – but urgent glucose should not be delayed for thiamine administration.
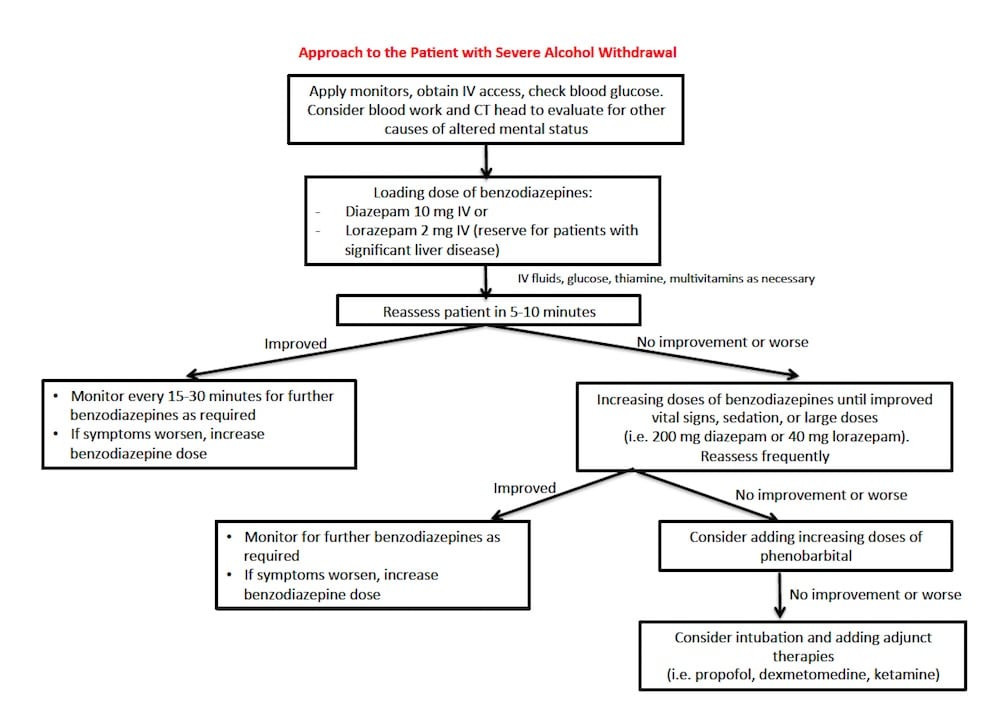
Management of Severe Alcohol Withdrawal
In the agitated and disorientated patient with alcohol withdrawal, avoid antipsychotics such as Haldol because these drugs can prolong the QT interval and reduce the seizure threshold.
Consider intubation in patients who have airway concerns or who have refractory seizures, and may require adjunctive treatments. There are several adjunct medications that can be considered for refractory cases of severe alcohol withdrawal that are not responding to large doses of benzodiazepines. These are usually started in ICU patients. In the intubated patient, consider propofol, phenobarbital, dexmedetomidine and ketamine.

Care of RebelEM
Suggested ICU Admission Criteria for Alcohol Withdrawal
- Underlying medical or surgical condition that requires ICU-level care
- Requires second line therapy to control withdrawal (benzodiazepine resistant withdrawal)
- Hyperthermia
- Recurrent seizures
- Severe altered mental status
Suggested Algorithm for Management of Severe Alcohol Withdrawal
For more on alcohol withdrawal and delirium tremens on EM Cases:
Best Case Ever 50 – Delirium Tremens with Sara Gray
Drs Gray, Kahan, Borgundvaag, Grewal and Helman have no conflicts of interest to declare
References
- Miller F, Whitcup S, Sacks M, Lynch PE. Unrecognized drug dependence and withdrawal in the elderly. Drug Alcohol Depend. 1985;15(1-2):177-9.
- Stehman CR, Mycyk MB. A rational approach to the treatment of alcohol withdrawal in the ED. Am J Emerg Med. 2013;31(4):734-42.
- Gray S, Borgundvaag B, Sirvastava A, Randall I, Kahan M. Feasibility and reliability of the SHOT: A short scale for measuring pretreatment severity of alcohol withdrawal in the emergency department. Acad Emerg Med. 2010 Oct;17(10):1048-54.
- Lorentzen K, Lauritsen AØ, Bendtsen AO. Use of propofol infusion in alcohol withdrawal-induced refractory delirium tremens. Dan Med J. 2014;61(5):A4807.
- Schuckit MA. Recognition and management of withdrawal delirium (delirium tremens). N Engl J Med. 2014 November 371;22:2109-2113.
- Amato L, Minozzi S, Vecchi S, Davoli M. Benzodiazepines for alcohol withdrawal. Cochrane Database Syst Rev. 2010;3:CD005063.
- Gold JA, Rimal B, Nolan A, et al. A strategy of escalating doses of benzodiazepines and phenobarbital administration reduces the need for mechanical ventilation in delirium tremens. Crit Care Med. 2007;35(3):724-730.
- Tolonen J, Rossinen J, Alho H, Harjola VP. Dexmedetomidine in addition to benzodiazepine-based sedation in patients with alcohol withdrawal delirium. Eur J Emerg Med. 2013 Dec;20(6):425-7.
- Mueller SW;, Preslaski CR, Kiser TH, et al. A randomized, double-blind, placebo-controlled dose range study of dexmedetomidine as adjunctive therapy for alcohol withdrawal. Crit Care Med. 2014;42(5):1131-9.
- Michaelsen IH et al. Phenobarbital versus diazepam for delirium tremens: a retrospective study. Dan Med Bull. 2010; 57 (8) A4169.
- Lizotte RJ et al. Evaluating the effects of dexmedetomidine compared to propofol as adjunctive therapy in patients with alcohol withdrawal. Clin Pharmacol. 2014;6:171-177.
- VanderWeide LA et al. Evaluation of early dexmedetomidine addition to the standard of care for severe alcohol withdrawal in the ICU: a retrospective controlled cohort study. J Intensive Care Med 2016; 31(3): 198 – 204).
- Donnino MW, Vega J, Miller J, Walsh M. Myths and misconceptions of Wernicke’s encephalopathy: what every emergency physician should know. Ann Emerg Med. 2007;50(6):715-21.
- Hendey GW, Dery RA, Barnes RL, et al. A prospective, randomized, trial of phenobarbital versus benzodiazepines for acute alcohol withdrawal. Am J Emerg Med. 2011;29(4):382- 385.
- Rosenson J, Clements C, Simon B, et al. Phenobarbital for acute alcohol withdrawal: a prospective randomized double-blind placebo-controlled study. J Emerg Med. 2013;44(3):592- 598.
Additional FOAMed Resources on Alcohol Withdrawal and Delirium Tremens
Justin Morgenstern on delirium tremens management on First10EM
Evidence-based look at dexmedetomidine as adjunct on ALiEM
EMdocs reviews the pearls and pitfalls of management
Salim Rezaei reviews the literature on adjuntive medications
Prolonged QT associated with alcohol withdrawal on Dr. Smith’s ECG blog




Great tips n practice changers.. Excellent as always
Dear EM Cases, have you read the article posted by Dr. Josh Farkas on Pulmcrit (https://emcrit.org/pulmcrit/phenobarbital-oks/) reviewing and advocating phenobarbital as 1st line agent for alcohol withdrawal? To say there is insufficient evidence for phenobarbital is an understatement. I would love to hear your take on Dr. Farkas’ article and references on a separate episode if possible, it is very well written and convincing. Thank you for your time and attention
Agree that it is very well written and convincing, however the evidence is still not robust enough to recommend phenobarb as first line. He is quoting a retrospective study where phenobarb was used as 2nd line – which we agree with – phenobarb is a great 2nd line medication. Benzodiazepines, IF used in adequate doses, with correct timing, as per CIWA very rarely fails. Benzos are generally safer (especially valium is safer than phenobarb in cirrhotic patients) and much more familiar to emergency providers. I think it is not unreasonable to start with phenobarb, however our efforts should concentrate on early accurate identification of withdrawal, rapid adequate treatment, prevention, education and anticraving medications rather than first line medication choice for severe withdrawal.
Dr. Helmen
Thank you so much for your article. Very thorough and helpful for anyone from a seasoned clinician, patient, or parent.
I used to work at a psychiatric ed where the first line was phenobarbitals. The nurses were not used to benzoes and If i ordered benzoes I would just get calls all night about ordering phenobarbitals.
I myself did not.have any adverse events with patients and did not personally see any big difference (besides it was maybe a bit harder to taper off phenobarbitals and if the patient needed other sedating agents for whichever reason it was an issue)
I know they did have an adverse event with overdosing a patient with suspected delirium tremens who they had to intubate , but I’m not convincedit would have been any other way had he been loaded with benzoes)
Bottom line: if your setup and department is up for it, then phenobarbitals can probably be just as safe as benzoes – however besides some people being strong advocates for it (like the professor Sigurd Benjaminsen, at the region I worked) I am unfamiliar with the evidence
Side note: I have heard some people from the ILAE favoring phenobarbitals as a second line agent in status epilepticus – especially if alcohol history
Dr. Helman, thank you for the reply! I take and appreciate your point on early identification of red flag signs and symptoms.
I am wondering if anyone knows of an alcohol to benzodiazepine equivalency chart. I do not feel that providers can conceptualize how much benzodiazepine is needed to match the intake of liquor that someone is ingesting. For example, when we treat diacetylmorphine withdrawal, we refer to MME’s which can help providers understand how much opioid someone is using. I see alcohol withdrawal often undertreated and I am looking for any suggestions to help providers feel more comfortable in the use of benzodiazepines at higher doses.
Hi Dr.Helman, is there any evidence use of Haloperidol to lower the seizure threshold?
Yes, in very high doses without any benzodiazepines on board. Best to combine Haloperidol with benzodiazepines for young agitated patients.