There are many complicated guides on airway management and protected intubation since the COVID-19 pandemic broke. This can be confusing in our rush to develop protocols and guides in our own EDs. In this podcast, part of the COVID-19 EM Cases 5-part series, we aim to simplify protected intubation so that you can adapt it to your ED rapidly. Canada’s leading airway expert, George Kovacs guides us through the general principles and important details of the protected RSI…
Podcast production, sound design & editing by Anton Helman
Written Summary and blog post by Anton Helman March, 2020
Cite this podcast as: Helman, A. Kovacs, G. Episode 140 COVID-19 Part 4 – Protected Intubation. Emergency Medicine Cases. March, 2020. https://emergencymedicinecases.com/covid-19-protected-intubation. Accessed [date]
This podcast and blog post are based on Level C evidence – consensus and expert opinion. Examples of protocols, checklists and algorithms are for educational purposes and require modification for your particular needs as well as approval by your hospital before use in clinical practice.
This podcast was recorded on March 19th, 2020 and the information within is accurate up to this date only, as the COVID pandemic evolves and new data emerges. The blog post will be updated regularly and we are working on a weekly update via the EM Cases Newsletter which will be replicated on the EM Cases website under ‘COVID-19’ in the navigation bar.
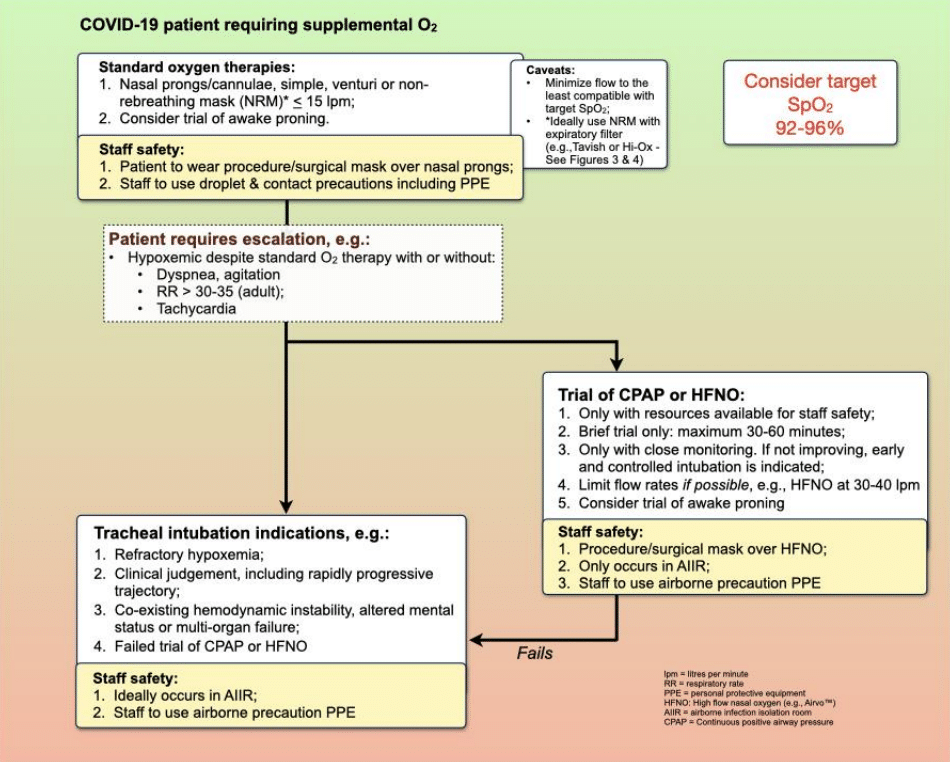
COVID-19 oxygenation algorithm and indications for intubation
Update April 2nd, 2020 Oxygenation Strategies on REBELEM
Update April 2nd, 2020 COVID Respiratory Severity Scale on MDCalc
What is different about the protected RSI compared to the standard RSI?
Guiding general principles of protected intubation
- The emphasis is on provider safety: rapidly securing the airway but slowing down to prepare yourself, your team and your patient with strict adherence to PPE donning/doffing
- With these safety measures we may not be able to optimize the patient prior to intubation as we normally would, and have to accept this.
- We need to pay particular attention to the details of how to prepare for, how to pre-oxygenate, and the sequencing of RSI
- There is no high level evidence for these modifications – at best the evidence is Level C – consensus/expert opinion
- Slow down so that you and your team’s safety is preserved – take the time to prepare yourself, your team and your gear before you enter the room
- We need to think about how PPE might effect our performance and come up with solutions or modifications
- Training properly is paramount to ensure the safety of ED providers and patients
Do’s and Don’ts of protected intubation
Do’s
- Do ensure viral filters on all masks (e.g. Tavish, HiOx NRB)
- Do accept lower oxygenation goals at lower flows
- Do have all necessary equipment at arm’s reach
- Do paralyze the patient before intubation to avoid coughing and subsequent aerosilization of particles and wait 45-90 seconds after pushing the paralytic
- Do understand that all patients will be apnea intolerant
- Do slow down to ensure you and your team are safe
- Do employ the most experienced available airway provider
- Do limit personnel in room to 3 if possible
- Do employ positive pressure ventilation and sustained waveform CO2 only after the cuff is inflated.
- Do ensure all connections are secure
- Do keep the patient sitting up for as long as possible before intubation and intubate at about 25-45 degrees head up position
- Do turn off the oxygen flow to NP/NRB before removing them from the patient to minimize aerosolization
- If a supraglottic airway is required, do ensure it is the adequate size, at the adequate depth, and the cuff is fully inflated (if your model has an inflatable cuff).
- Do wait ≥15 mins after intubation to take portable CXR
- Do use 2 hand vice grip/2 person jaw thrust for BVM
- Do have a dissociative dose of ketamine ready to give slowly during pre-oxygenation as per delayed sequence intubation for uncooperative patients
- Do consider HFNC with mask overtop for COVID pts in respiratory failure when ventilators and/or ICU beds are in short supply
- Clamp the ETT before disconnecting the BVM and connecting the ventilator
- Adapt your airway management/RSI algorithm and equipment to your ED
- Do have a trained observer watch you don and doff PPE
- Do have a shower and put on new greens after doffing PPE
- Do simulated protected intubations in your ED – train, train, train, practice, practice, practice!
Don’ts
- Don’t delay intubation if in doubt
- Don’t rush donning/doffing or aerolization prevention measures
- Don’t use BiPAP whenever possible
- Don’t use nebulizers
- Don’t employ positive pressure ventilation before the cuff is inflated
- Don’t auscultate to confirm tube placement
- Don’t bag the patient unless absolutely necessary
- Don’t employ positive pressure ventilation whenever possible
Indications for early intubation of the COVID-19 patient
Significant hypoxemia refractory to non-rebreathing mask at flows < 15 lpm in conjunction with one or more of the following:
-
- Clinical signs of the patient tiring:
- Dyspnea;
- Tachypnea with RR > 30-35 (adult);
- Tachycardia;
- Agitation;
- Accessory muscle use; paradoxical chest/abdomen movement
- Worsening PaO2/FiO2; Increasing PaCO2;
- Rapidly progressive disease trajectory or other clinical judgement.
- Clinical signs of the patient tiring:
Other standard indications for tracheal indication, e.g., failure to protect the airway or obstructing airway pathology, hemodynamic instability, sepsis, multi-organ failure.
Protected intubation preparation: Personel, Pre-brief, Equipment, Medications and Checklists
Protected intubation personnel – all in PPE (except runner and safety officer)
Inside room: MD1, RN1, RT
Outside room: MD2, RN2, RN3 (runner), Safety officer
Pre-brief for protected intubation
- Role assignment
- Equipment and medication packs check (see below)
- Turn on speaker phone
- Plan for pre-oxygenation, Plan A, re-oxygenation after 1st attempt, PLAN B and C and cardiac arrest management modifications
Suggested equipment for protected intubation
Note that these equipment packs should be modified for your specific needs and approved by your hospital before use.
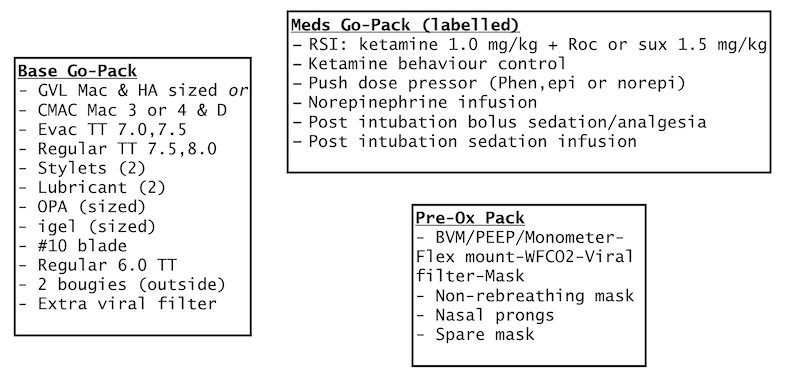
Example of protected intubation equipment packs which should be modified for your needs
- Closed system suctions x 2
- BVM with viral filter and PEEP valve (spare mask)
- Tracheal tubes: (Evac, standard or Parker Flextip), stylets, 10- cc syringe
- Primary device Macintosh-VL with bougie
- Secondary device Hyperangulated-VL with prepared tube stylet to appropriate shape
- SGA that supports flexible endoscopic intubation, ideally with an esophageal drainage port (igel)
- Cricothyrotomy: Bougie, #10 scalpel blade, 5.5 and 6.0 TT
- Tube clamp (to clamp ETT when transferring from manual resps to ventilator)
- Ventilator
EMcrit COVID Intubation Packs and Pre-oxygenation with Apneic CPAP video https://youtu.be/C78VTEAHhWU
Update 2021: Multi-center ED and ICU randomized control trial assessing “first pass” intubation success rate with either bougie first (n=566) or endotracheal tube (ETT) and stylet (n=546). No difference between both groups in first pass success rate across mix of providers (residents, ED attendings, and ICU). Abstract
Medications for protected intubation to be drawn up outside room
- Norepinephrine infusion (0.1 mcg/kg/min infusion started 16 mcg/ml mix)
- Bolus dose rescue pressor (Epinephrine 5-20 mcg; Phenylephrine 50-200 mcg; Norepi 8-16 mcg= 0.5-1 ml of 16 mcg/ml infusion mix in 3cc syringe)
- Consider glycopyrolate 0.2 mg IV (to help minimize ketamine-related secretions)
- Ketamine 0.2-1mg/kg, Rocuronium 1.5 mg/kg
- Fentanyl infusion Dosing: 0-100 mcg/hr; Typical starting dose 25-50mcg/hr
Checklists for protected intubation
Example of Protected intubation checklists for MD, RT, RN, Safety Officer
Example of Protected intubation checklist one-pager
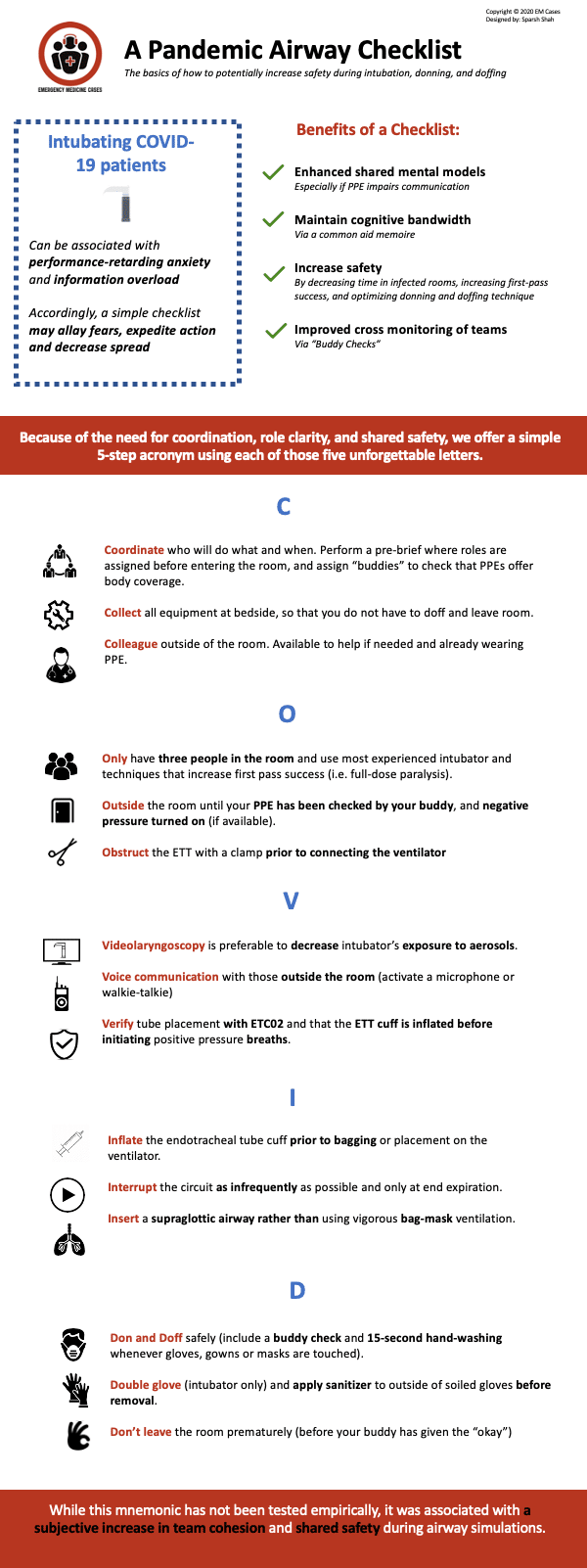
Adapted from “A pandemic airway checklist: the basics of how to potentially increase safety during intubation, donning, and doffing” by Brindley, P, Mosier, J and Hick, C.
Passive Pre-oxygenation *NO BAGGING
Update April 5th, 2020 Preoxygenation video with George Kovacs
*Use the lowest flow necessary to achieve an oxygen saturation of 90%
*Have a dissociative dose of ketamine ready to give slowly during pre-oxygenation as per delayed sequence intubation for uncooperative patients.
- Nasal prongs (NP) 5L max
- Non-rebreathing Mask (NRB) 15L max (Tavish or HiOx see image)
- BVM + PEEP valve + viral filter + flex mount + waverform CO2 at 15L O2, 10cm PEEP
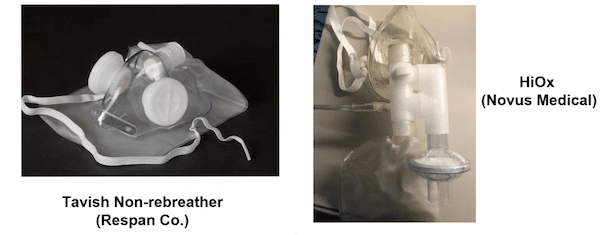
NRB options for protected RSI and respiratory management
Update March 29th: We know that BVM can aerosolize virus particles, especially when bagging (which is generally not recommended in the COVID era), however BVM is recommended as an option for pre-oxygenation and re-oxygenation after a failed first attempt. A key aspect of the technique to minimize the chances of aerosolization is the type of grip. The “CE” grip is the one handed grip which is not recommended and the “VE” 2-handed grip (with aggressive jaw thrust and the thenar eminences almost touching) is recommended (see image).

Left: “CE” one handed grip not recommended. Right” 2 handed “VE” grip with thenar eminences almost touching is recommended for BVM in the protected RSI
Update April 1st, 2020 George Kovacs video on 2 handed VE grip VIDEO
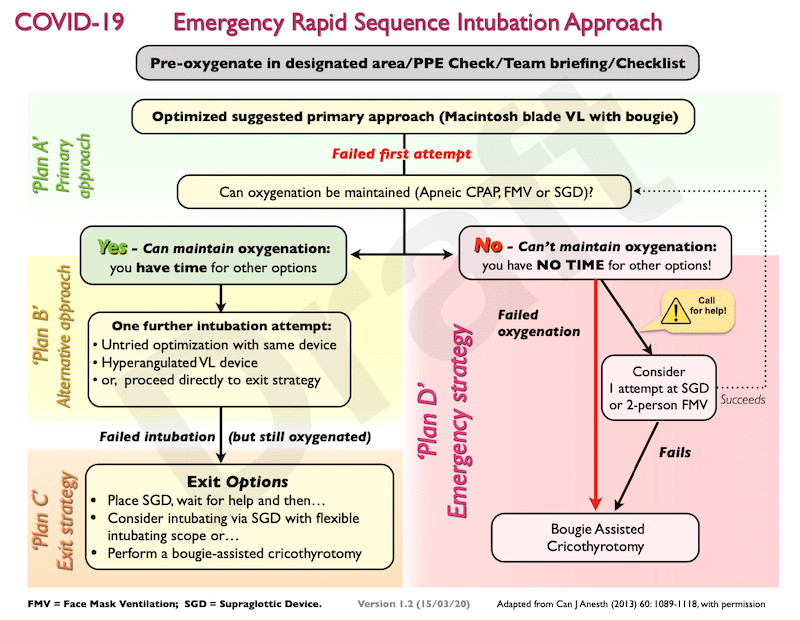
The protected intubation
Primary intubation device: Macintosh video laryngoscopy with bougie
Optimized Macintosh video laryngoscopy with bougie: video https://vimeo.com/382021758
Examples of Macintosh VL include:
-
-
- Storz C-MAC® S with single-use Macintosh 3 or 4 blades;
- GlideScope ® Spectrum™ with single use [Macintosh-shaped] DVM 3 or 4 blades;
- McGrath Mac with single-use Mac size 3 or 4 blades.
-
If no Macintosh device is available, use hyperangulated video laryngoscopy.
*Using a conventional out-of-package (straight to coudé tip) bougie is not recommended as an adjunct with hyperangulated video laryngoscopy. In experienced hands, a ‘customized’ distally bent bougie, a purposeful made malleable or steerable bougie may be used with hyperangulated video laryngoscopy.
Optimized hyperangulated video laryngoscopy: video https://vimeo.com/404091445
Examples of hyprangulaed VL include:
-
-
- Storz C-MAC® S with single-use D-blade;
- GlideScope ® Spectrum™ with single use LoPro S3 or S4 blade;
- McGrath™ Mac with X blade.
-
Re-oxygenation options after failed 1st attempt in protected intubation
- Apneic CPAP: 5LNP, BVM – 10cm PEEP, 15Lpm https://vimeo.com/400368564. (see image below)
- Note that you won’t see an ETCO2 trace unless you gently provide pressure support. Anytime you squeeze the bag there is some risk to aerosolization. The risk of controlled ventilation (6-10 breaths over 1 minute) must be balanced against worsening hypoxemia that results in cardiac arrest.
- Controlled manual ventilations (gentle pressure support): 6-10 over 1 minute, ≤15 pressure
- Place an oral airway and apply your filtered BVM system with 10cm PEEP, 15 LO2 with manual breaths (6-10 over 1 minute). Having a pressure manometer attached to the MDI port to avoid pressures >15 is ideal.
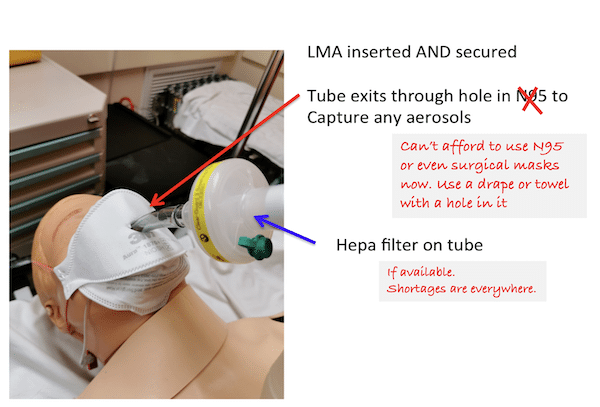
- Supraglottic airway (2nd generation SGA e.g.EMS igel recommended)
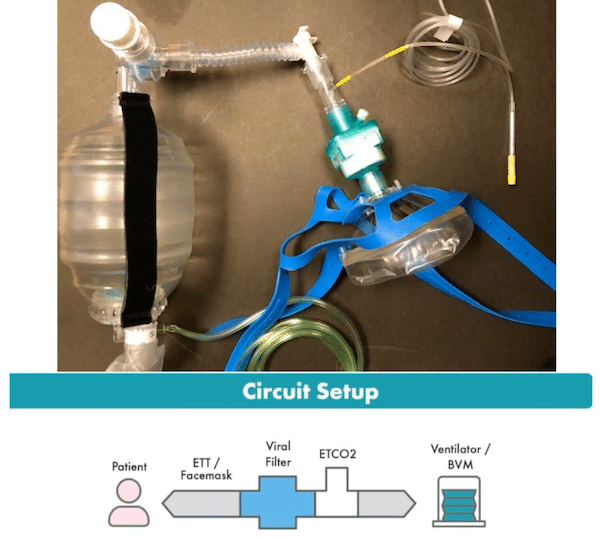
BVM with PEEP valve, ETCO2, viral filter, straps for apneic CPAP care of George Kovacs
Plan B options in protected intubation
- Hyperangulated blade VL (if Macintosh VL used in 1st attempt)
- Supraglottic airway (SGA)/LMA – igel preferred
Plan C in protected intubation
Scalpel/Bougie Cricothyrotomy – If you can’t maintain oxygenation by either apneic CPAP, controlled ventilation or an SGA, employ your ‘emergency’ double setup strategy and perform a cricothyrotomy.
Modifications to scalpel/bougie cricothyrotomy
- Do not proceed with ventilations through the mouth/nose
- Cover the patient’s mouth and nose with a mask when they are placed on the ventilator
Initial vent settings after protected intubation
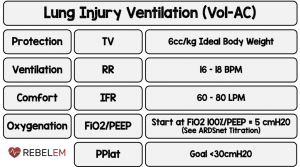
Via Salim Rezaie REBEL EM
Update April 9th, 2020 – some experts are recommending initial vent setting RR of 25 breaths per minute.
Update April 9th, 2020 – consider ongoing paralysis and/or proning (by trained team) if having difficulty oxygenation despite increasing FiO2
Update May 1st, 2020 updated AIME protected airway guideline
High Flow Nasal Cannula (HFNC) in COVID-19 protected airway management
- HFNC is thought to increase the risk of viral spread through aerosolization, but, in combination with a mask placed overtop, is thought to be safer than CPAP/BiPAP
- The WHO and Surviving Sepsis Guidelines on COVID-19 do recognize HFNC as an option for respiratory failure associated with COVID-19
- HFNC has/is being used in China, Italy and United States.
Updated AIME protected airway guideline May 1st, 2020
Example of protected intubation MD, RT, RN and Safety officer checklists
COVID Safety Airway Course – instructor’s manual, guide, videos
Airway Interventions & Management in Emergencies (AIME) COVID-19 Materials
References
- Consensus statement: Safe airway Society principles of airway management and tracheal intubation specific to the COVID-19 adult patient group. Medical Journal of Australia pre-print (open access). Available at: https://www.mja.com.au/journal/2020/212/10/consensus-statement-safe-airway-society-principles-airway-management-and
- Royal College of Anaesthetists COVID-19 Airway Management Principles https://icmanaesthesiacovid-19.org
- David J Brewster, Nicholas C Chrimes, Thy BT Do, et al. Consensus statement: Safe Airway Society principles of airway management and tracheal intubation specific to the COVID-19 adult patient group. The Medical Journal of Australia. 2020.
- Justin Morgenstern, “COVID airway management: SAS consensus statement”, First10EM blog, March 19, 2020. Available at: https://first10em.com/covid-airway-management-sas-consensus-statement/.
- The Safe Airway Society principles of airway management and tracheal intubation specific to the COVID-19 adult patient group
- The WHO guidance on the clinical management of severe acute respiratory infection when novel coronavirus (nCoV) infection is suspected
- The Canadian Anesthesiologists’ Society COVID-19 recommendations during airway manipulation
- Weber RT, Phan LT, Fritzen-pedicini C, Jones RM. Environmental and Personal Protective Equipment Contamination during Simulated Healthcare Activities. Ann Work Expo Health. 2019;63(7):784-796.
- Macintyre CR, Seale H, Dung TC, et al. A cluster randomised trial of cloth masks compared with medical masks in healthcare workers. BMJ Open. 2015;5(4):e006577.
- Murthy S, Gomersall CD, Fowler RA. Care for Critically Ill Patients With COVID-19. Jama 2020;18–9.
- Luo M, Cao S, Wei L, et al. Precautions for Intubating Patients with COVID-19. Anesthesiology 2020;1.
- Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 2020;395(10223):507–13.
- Wax RS, Christian MD. Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019-nCoV) patients. Can J Anesth 2020;
- Caputo KM, Byrick R, Chapman MG, Orser BJ, Orser BA. Intubation of SARS patients: infection and perspectives of healthcare workers. Can J Anaesth 2006;53(2):122–9.
- Weingart SD, Trueger NS, Wong N, Scofi J, Singh N, Rudolph SS. Delayed sequence intubation: a prospective observational study. Ann Emerg Med 2015;65(4):349–55.
- Driver BE, Prekker ME, Klein LR, et al. Effect of Use of a Bougie vs Endotracheal Tube and Stylet on First-Attempt Intubation Success Among Patients With Difficult Airways Undergoing Emergency Intubation. JAMA 2018;319(21):2179.
Drs. Helman and Kovacs have no conflicts of interest to declare




Excellent and very useful
Amazing episode
Very informative and reassuring
Thank you so much
thoughts on inflating cuff with lidocaine instead of air to reduce cough reflex?
Tarinder (rural ED doc in BC)
The patient should be paralyzed so no cough reflex.
Great talk. Any advice on the patient who is deemed the “anticipated difficult airway” in whom you would generally carry on with an awake intubation? In the context of COVID19 or suspected COVID19?
Some experts are recommending approaching every COVID patient as an “anticipated difficult airway”, and having a Plan A, B, C that includes VL, SGA, Cric will cover any eventuality. For me, if VL fails my plan B is 2nd generation SGA followed by call to anesthesia for fiberoptic intubation through the SGA. Interested in others’ thoughts.
Great question re anticipated difficult airway. Simple answer is that an awake intubation is relatively contraindicated. We have fallen back to a ‘double set up’ approach. However if you feel it absolutely needs to be considered this should be done under guidance of an anesthesiologist trained to do a protected awake approach. Quite frankly I don’t know of anyone doing this.
1)With tolerating/expecting more hypoxia should we expect we might encounter bradycardia more often during intubation and also think about having atropine on hand or even pretreat?
2) an anesthesia colleague thought that you should choose rocuronium over succinylcholine for intubation due to theoretical risk of fasiculations causing aerosolization. Any thoughts ?
Btw very much appreciate the podcast and information provided!
Thanks for a great show, as ever.
Re preoxygenation, isn’t the bag valve/PEEP-mount-etco2-viral filter-mask set-up going to offer lots of resistance to thh awake patient taking spontaneous breaths?
I understand 15l/min O2 via standard NRBM is aerosol-generating, and in any case many patients will be significantly hypoxic despite being on this before the decision is made to intubate them.
Is ventilator-assisted preoxygenation a superior means for preoxygenating the spontaneously breathing patient? (So long as a good deal came be obtained on a standard NIV mask). What are your thoughts?