This is Part 3 of our series on COVID-19.
Part 1 Screening, Diagnosis & Management
Part 2 Surge Capacity Strategies
Part 5 Epidemiology & Prediction Models
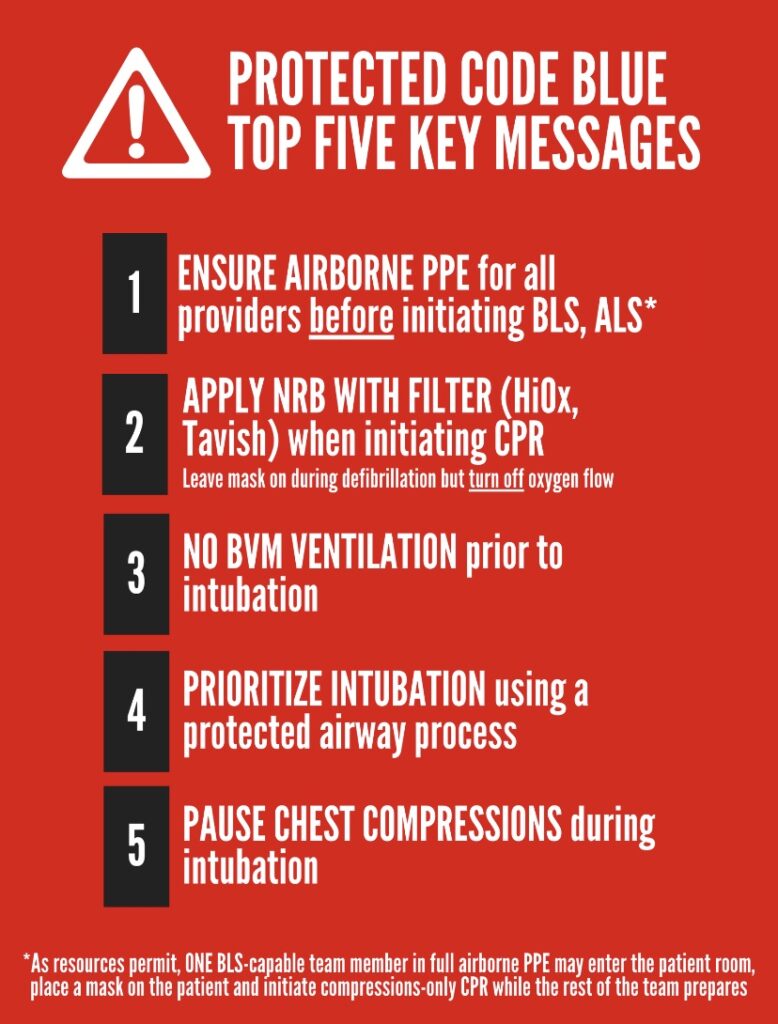
The single most important thing we can do as ED providers in this COVID pandemic is to protect ourselves, our colleagues, our patients, our families and our friends against transmission of the virus; and there is no higher risk of transmission that during the resuscitation of a sick COVID patient. In this podcast we speak with a world expert on PPE, Dr. Laurie Mazurik about protecting against transmission of the virus before, during and after your shift. Not only do we discuss the details of all PPE from head protection to footwear, but we give tips on the equally important non-PPE protection as well. We touch on PPE conservation strategies as we struggle with supplies, give you the bottom line on donning/doffing sequencing, and discuss the core principles of the protected code blue…
Podcast production, sound design & editing by Anton Helman
Written Summary and blog post by Anton Helman March, 2020
Cite this podcast as: Helman, A. Mazurik, L. Episode 139 COVID-19 Part 3 – PPE: What We Know and Conservation Strategies. Emergency Medicine Cases. March, 2020. https://emergencymedicinecases.com/covid-19-ppe. Accessed [date]
This podcast and blog post are based on Level C evidence – consensus and expert opinion. Examples of protocols, checklists and algorithms are for educational purposes only and require modification for your particular needs as well as approval by your hospital before use in clinical practice.
This podcast was recorded on March 20th, 2020 and the information within is accurate up to this date only, as the COVID pandemic evolves and new data emerges. The blog post will be updated regularly and we are working on a weekly update via the EM Cases Newsletter which will be replicated on the EM Cases website under ‘COVID-19’ in the navigation bar.
Update April 2021: An article was published listing ten scientific reasons in support of COVID airborne transmission, furthering the evidence for current protocols, including PPE and protected code blue. Full text
Protecting against COVID-19 transmission before your shift, during your shift and after your shift
Before and after your shift
Adapted from decontamination checklist by Lauren Westafer
- Avoid public transit
- Bring your own food/drink supply
- Remove jewelry, watches
- If you have long hair, tie it up in a tight bun
- Obtain clean scrubs at the hospital if possible
- Place all your work gear – stethoscope, pens, phone, clipboard etc in a freezer zip lock bag
- Use a separate pair of waterproof shoes that you leave at work
- Take an extra large freezer bag or garbage bag to place your clothes into
- Take with you disinfectant wipes (or if they have run out in your community mix 25mL of bleech in 750mL of water in a spray bottle so that you can wipe down your car steering wheel, gear shift and seat).
- After your shift, if possible, shower at the hospital leaving your scrubs there (or place them in a separate freezer bag) and change into the clothes that you kept in the freezer bag. If there is no shower at the hospital, wash your hands, arms and face with soap. Change from your hospital shoes into your home shoes. Sanitize your badge and phone and place all your gear back into a freezer bag.
- When you get home leave your work gear in the garage or shed or under an upside down bucket outside. Put your water bottle and food container directly into the dishwasher and clothes into the washing machine using hot water.
- Take a shower
Tip for interviewing and swabbing low risk COVID patients: For isolated low risk patients, consider not entering the patient room initially; rather do a phone interview. Then make an assessment plan. When obtaining swabs, stand to the side and behind the patient, and ask them to put their mask just below their nose and turn away from you if they feel they are going to sneeze or cough.
Personal protective Equipment (PPE)
Transmission of COVID-19 is approximately 3 x more likely to occur at the ED than elsewhere and certain procedures like intubation create the highest risk. You need to learn about PPE, and how to use it properly. Yours and the lives of others depends on it.
Tip 1: PPE recommendations change frequently. This is especially the case in emerging diseases, where there may be some uncertainty about the mode of transmission and in the case of COVID 19, the sheer amount of PPE being consumed is leading to global shortages. Make every effort to adapt.
Tip 2: Non-PPE Protection is equally important!
- Distance of 2 m
- Structural Barriers between you and the patient (wall, doors, etc.)
- Interview patients by phone & use telemedicine where possible
- Keep the time you are with the patient to a minimum. Avoid all unnecessary procedures
- Keeping your environment clean. Wipe keyboards, desktops, pens, etc.
- Eat in designated areas, and bring your own snacks and food
- Wear only your scrubs under PPE; no jewelry, watches, or street clothes under PPE.
- No pens, charts or clipboards should go into the room.
- You can decide if you want to take your stethoscope in but clean it with a CAVI Wipe afterwards.
- If you have a beard or mustache strongly consider shaving it or trimming it so it does not break the N95 respirator’s seal.
- Avoid aerosol generating procedures where possible; nebulizers, BVM,CPAP,BiPAP, High Flow Nasal Cannula and bronchoscopy.
How to wash your hands properly: The COVID Scrub
Tip 3: Not all PPE is equal!
Gowns
Gowns are graded in fluid resistance from: Level 1 (~no resistance to fluids), to Level 4 which is impervious. They also vary in coverage, with some covering only the front of you, like an apron with sleeves.
- Most see-through gowns are level 1 gowns and this in not adequate protection for COVID 19.
- The gown should ideally be fluid resistant, long sleeved and fully cover your back.
- A washable, (reusable) Level 2 gown is the minimum requirement for high risk procedures
March 28th update: Some see-through gowns are Level 2 gowns. Everyone should confirm this locally and read all the specs on their gown to confirm this.
Most see-through gowns are level 1 gown and this in not adequate protection for COVID 19; a washable, (reusable) Level 2 gown is the minimum requirement for high risk procedures.
Eye Protection
Eye protection comes in the form of goggle or glasses. These may be personal issue and re-used by cleaning with a solution that does not etch the surface. They protect your eyes from being touched or having secretions sprayed into them.
Face Shields
- Face shields provide superior protection to goggles or glasses, because they cover you face, part of your neck and all of your mask. There are re-useable face shields, usually personal issue, and like glasses must be cleaned with solutions that do not etch their surface.
- Bibbed face shields may be available. They have a small drape that hangs down to cover your neck,
- If you are thinking about combining a face shield with goggles or glasses, think twice, as this combination often fogs, leading to you touching the equipment to adjust it.
Reusable face shields provide superior protection to goggles or glasses.
Hair Cover or Bouffant
These not in the current guidelines by WHO but frontline staff expressed concerns that their hair, sides of face and neck exposed to a patient’s cough. A Bouffant seems to capture some of the spray.
Neck protection and hoods
Hoods are not currently recommended and are hard to find. They provide additional head and neck cover.
Two things you can do to provide neck protection
- Tie your gown as high on your neck as possible
- After doffing, clean your neck with hand sanitizer or soap and water (and take a shower if there may have been a significant breach during the procedure)
Footwear
- Boot or shoe covers are not currently recommended by WHO. You will see them used in China in high viral load areas i.e. COVID 19 wards, ICU, etc.
- Rubber shoes are not currently recommended by WHO. Wear closed shoes, and always leave them at work.
Gloves
Nitrile gloves come in 2 lengths extended and regular. Reserve the extended if for some reason the others don’t cover the cuff of your gown. Should you wear 1 pair or 2 pairs? Well that depends if you have to wear PPE all shift, you may end up washing your hands so much that your skin breaks down. Some people may choose to wear two pairs, disposing of the outer pair between patients and washing the under pair the same way they would their hands. Check with your IPAC to decide what’s best for you.
Masks
- Surgical masks were designed to protect the patient from you and have a simulated workplace protection factor (SWPF) of 2. They are loose fitting. These are to be given to the patient to prevent them from spreading the virus. They are also felt to be adequate respiratory protection for droplet spread diseases like COVID 19, except if aerosols are generated.
- N95 respirators are fitted, have a SWPF of ~ 10, and provide airborne protection, stopping particles as small as ~0.3 microns. Although COVID 19 is droplet spread (~10 microns), aerosol generating procedures such as BVM, BiPAP, CPAP, HFNC, Bronchoscopy and Intubation, will create smaller droplet nuclei, which are suspended in the air for a period of time. This puts you at greater risk of inhaling and contracting the virus.
- Powered Air Purifying Respirators provide the highest level of respiratory protection (SWPF 1000+) and are not currently recommended and extremely difficult to obtain in Canada.
PPE conservation strategies
There is a global PPE Shortage and strategies are being developed to preserve, use longer and re-use PPE. For example, staff are asked to use a single mask or N95 respirator for as long as possible, changing it only if it gets wet or contaminated. There are tests looking at the use of UV light or microwaving to sterilize a mask or N95 but there are no clear indications at this time that is safe to do. There have been suggestions that if someone runs out of respiratory protection, they should use a bandana. However, we can definitely do better. Scientists and mask/respirator experts need to collaborate to provide a better option. Using washable re-usable gowns, face shields and glasses or goggles are also part of the conservation strategy.
Manufacturers retooling to make PPE: e.g. Bauer Hockey Equipment to make Face shields for Health Care Providers: https://globalnews.ca/news/6734828/coronavirus-bauer-face-shields/
Using industrial protective equipment: cleanable and re-usable face shields from big box hardware stores
DIY Masks: Cambridge University analysis of materials to filter viruses
Quilted materials may be best as they are breathable and the mesh of fibres is better than one layer.
Re-using N95 masks: putting an N95 in a conventional oven at 70C (158F) for 30 minutes should be effective in killing SARS CoV2 and does not degrade the mask itself (see chart below)
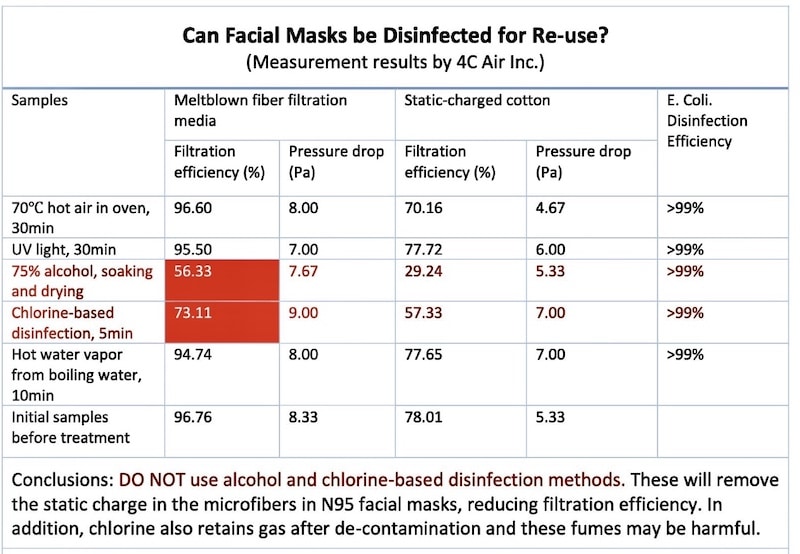
From Stanford’s “Addressing COVID-19 Face Mask Shortages” https://m.box.com/shared_item/https%3A%2F%2Fstanfordmedicine.box.com%2Fv%2Fcovid19-PPE-1-1
Update April 6th, 2020 CDC PPE Decontamination Reuse Strategies
PPE donning/doffing sequence
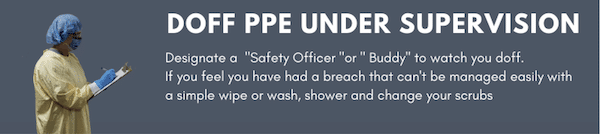
This takes practice, and is best done under the supervision of a designated buddy or safety officer who uses a checklist to insure you do this properly without a breach in protection.
The only hard rules to remember for PPE donning/doffing:
1. Mask/N95 should always be FIRST ON & LAST OFF.
2. Take your dirtiest PPE off first.
From ECUUS
Don’t forget to do a seal check on your N95.
Where do you DOFF PPE?
If you have a room with an anteroom, you doff in the ante room unless your gown or gloves are heavily soiled. Remove heavily soiled gowns or gloves in the patient’s room standing at least 2 m from them. Then take your mask/N95 off in the anteroom.
If you don’t have an ante room, take everything off except your N95/Mask (and hair cover if you have one) off in the room (at least 2 m/ 6ft from the patient). Take your N95/Mask off outside the patient’s room as it is your most important defence against respiratory infection when you are exposed to the patient.
Sometimes though, the room is so small you can’t possibly be 2 m away from the patient, so may have to doff outside the room and clean that area where you doffed, afterwards.
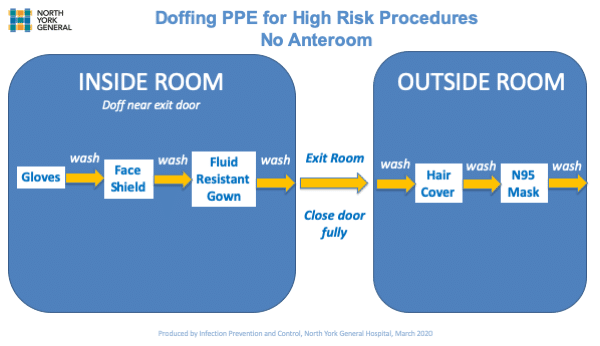
PPE doffing if no anteroom example
The risk of transmission is related to the viral load and duration of exposure
Viral loads are highest in the very ill patients and exposure risk is highest if aerosols are generated through:
- Triggered coughing i.e. intubation without paralytics or suction
- BiPAP, CPAP
- High flow oxygen systems such as high flow nasal cannula
- Nebulizers
- Bag mask ventilation with a poor seal
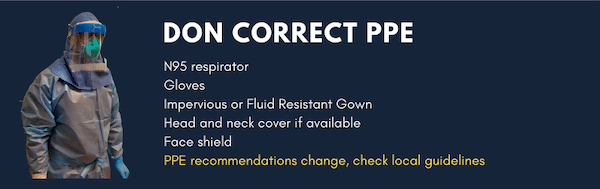
PPE for high risk procedures that generate aerosols
The highest risk to staff is intubation.
It was estimated that 9% of staff involved in intubating SARS patients at one Toronto hospital contracted SARS. None died. It is expected that within the patient care setting, SARS-CoV-2 will spread to health care workers the same way as SARS did in 2003.
From ECUUS
The current recommendation in Canada for performing an aerosol generating procedure is: N95, eye or face protection, gown and gloves.
No head or neck protection is recommended at present. From doing informal glo-germ tests (blow a small amount of florescent powder at someone in PPE before they doff from ~ 1 m away,) we found contamination of neck, ears and hair. In the Middle East where they intubate the much more lethal corona virus MERS, part of their protocol after removing PPE it to always wash their face and neck.
Wear head and neck cover as available and wash your face and neck afterwards. If you have a breach that is not easily solved this way, take a shower.
Be prepared for personal protection recommendations to change or vary between various regions or countries. Supply chain issues are occurring. Learn about the different types of PPE and be ready to find new ways to reduce your risk. Collectively adapt to whatever comes your way.
Basic protected intubation and code blue principles
- Avoid all aerosol generating procedures whenever possible
- Keep both the number of people and the duration of exposure to a minimum
- Wear the correct PPE and doff under supervision
- Use clear plans and checklists where possible
- Think A-B-C not CAB in cardiac arrest. Secure the airway to protect the team first.
To keep you and your team safe you must train, train train; practice, practice practice – please use the following free resources to develop a rapid training course for safe resuscitation of COVID-19 patients in your ED
EM Deliberate Practice Free Airway Safety Training Course Materials
Curriculum pdf
Instructor’s Notes pdf
Site Director Logistics pdf
Scheduler pfd
Next in the COVID-19 podcast series Anton interviews George Kovacs on Airway, Resuscitation and The Protected Code Blue
References
- David J Brewster, Nicholas C Chrimes, Thy BT Do, et al. Consensus statement: Safe Airway Society principles of airway management and tracheal intubation specific to the COVID-19 adult patient group. The Medical Journal of Australia. 2020.
- The Safe Airway Society principles of airway management and tracheal intubation specific to the COVID-19 adult patient group
- Weber RT, Phan LT, Fritzen-pedicini C, Jones RM. Environmental and Personal Protective Equipment Contamination during Simulated Healthcare Activities. Ann Work Expo Health. 2019;63(7):784-796.
- Macintyre CR, Seale H, Dung TC, et al. A cluster randomised trial of cloth masks compared with medical masks in healthcare workers. BMJ Open. 2015;5(4):e006577.
- Luo M, Cao S, Wei L, et al. Precautions for Intubating Patients with COVID-19. Anesthesiology 2020;1.
- Wax RS, Christian MD. Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019-nCoV) patients. Can J Anesth 2020;
- Caputo KM, Byrick R, Chapman MG, Orser BJ, Orser BA. Intubation of SARS patients: infection and perspectives of healthcare workers. Can J Anaesth 2006;53(2):122–9.
- Viscusi DJ, Bergman MS, Eimer BC, Shaffer RE. Evaluation of five decontamination methods for filtering facepiece respirators. Ann Occup Hyg. 2009;53(8):815-27.
Drs. Helman and Mazurik have no conflicts of interest to declare





People can be instructed how to self swab particularly a nasal swab where a study from China found high viral load .
There are maximal PPE available in industry as in the Welding PPE with respirators – look scary but for looking after Ventilated patients who require close contact procedures would protect .
The are also industrial raincoats with hoods 3mm thick which could be sprayed with the dilute bleach 25ml bleach /700 ml water but do outside with care .
Then there is the possibility of finding rooms with windows that can be opened and that can be fitted with Viral (Hepa Filters ) for aerosol procedures .
Vitamin D from the sun increases immune power hence the sanitoriums for TB in Arizona so in the pro drome fresh air and sun in a garden or courtyard is worth trials
There ought be glow germ tests also .
Thank you for your devotion skill and courage .
Drs. Helman and Mazurik,
This was a fantastic post. Very timely and practical, many thanks.
Could you comment on the lack of recommendations regarding neck covering during intubation?
The Canadian recommendations by Wax et al. from the Canadian Journal of Anesthesia in February 2020 (https://doi.org/10.1007/s12630-020-01591-x) clearly recommend hoods.
Moreover the Canadian Anesthesiologists’ Society position statement from March 2020 also recommend neck covering during intubation (https://www.cas.ca/CASAssets/Documents/News/Updated-March-25-COVID-19_CAS_Airway_Vsn_4.pdf).
These Canadian statements are mirrored internationally by arguably the body who has seen largest number of these cases until recently: the Chinese Society of Anesthesiologists (published in the Chinese Medical Sciences Journal in February 2020; doi:10.24920/003724).
There are no recommendations yet from an emergency medicine body, however I wonder whether we should endorse the safest guidelines from our anesthesia colleagues while we are providing anesthesia and critical care to these patients.
Best wishes,
Miguel
Great question by Miguel:
I share the desire to have a hood and recommend you use them if you have them. Without a doubt they give superior neck and head coverage and there is minimal risk of self contamination when you doff, especially if you practice and use a spotter or safety officer who watches you.
BUT what if you can’t get them or are told you don’t need them and this is backed up by your own IPAC, WHO and CDC.
https://apps.who.int/iris/bitstream/handle/10665/331498/WHO-2019-nCoV-IPCPPE_use-2020.2-eng.pdf
https://www.cdc.gov/coronavirus/2019-ncov/hcp/respirator-use-faq.html
I reached out to someone in the Middle East and asked what they wore when they intubated MERS patients.
The PPE used: N95, hooded body suits or hoods and gowns, Face Shield, Level 2 or higher Gown, and gloves.
PLUS post doffing they WASHED their face and neck with soap and water. Apparently no one got MERS.
Washing with soap & water or sanitizing your face and neck after doffing your PPE is virtually never (if ever) talked about, but maybe it should be part of the regimen.
So, bottom line if your are going to intubate or do something that will generate aerosols:
IF you have a hood: use it.
IF you don’t: Wear a bouffant, a * face shield with a bib (if available) , tie your Level 2 (or higher) gown up high on you neck and of course wear N95 & gloves.
* Face shield is considered superior to glasses or goggles as it covers the mask/N95 and face
AFTER you doff under supervision, (with or without a hood), sanitize your hands and then wash or sanitize your face and neck. If you are still concerned, shower and change your greens.
Should we advocate for obtaining hoods?
It never hurts to ask, but the global PPE shortages are posing significant challenges.
What we should be doing is recording and tracking what people wear when they intubate, to see if the incidence of transmission is less in those who wear hoods.
Hope that answers your question (which is a great one!) and gives those without hoods (most of us) some ideas on how to increase head and neck protection.
Hey Ian,
I was shocked how much someone coughed on me when I did a mid turbinate swab. Since then I stand beside and somewhat behind them, tell them what I am going to do and tell them to pull up their mask and turn away from me if they are going to cough or sneeze. I also 100% AGREE that almost every one of these patients can do this themselves with minimal instruction (stick it up your nose and then put it in the test tube thing). We can watch on the other side of a glass door or through a camera to make sure they do it right.
I follow the ACEP forums and there is ALL KINDS OF ACTIVITY about alternate PPE. There are serious concerns about running out in different regions. Rain Coats come up over and over, as a substitute for tyveks body suits or gowns. The challenge is they are HOT. I am not sure if you have every been in a waterproof CBRN or hazmat suit, but you cannot tolerate it very long maybe and hour or so. The use of dilute bleach to decontaminate hazmat suits is also used. I haven’t hear of the other things you mentioned, but will look into it. Thanks for your comment!
Just want to say thanks for all the great content
…take care
Hi Dr Mazurik,
Thank you for all the great info in this post–really appreciated. I was listening to the CAEP Town Hall yesterday, and it’s my understanding that you had mentioned that coughing is aerosol-generating. I was wondering if you could please elaborate on that and what it could mean in terms of our PPE needs, given many of our rule-out COVID patients in the ED present with cough but neither we, nor they, are wearing PPE for aerosol considerations.
Thank you for your time and care, and please stay well and safe!
Sarah-Taissir
Thank you for this information. My hospital has created a “red zone” where we capture all respiratory patients (many undifferentiated) and separate those from the “green zone” . Obviously when we enter “red zone” rooms we don full PPE. Can you comment on what PPE healthcare workers in the “red zone” should wear while outside patient rooms (charting, walking in hallway, etc)?
Many thanks
Best to go by your IPAC protocols as they vary by region and local PPE supplies. At our ED we are advised to wear: surgical mask, visor, bouffant, level 2 gown in ALL PATIENT AREAS to be replaced by maximum PPE (including N95) for any aerosolizing procedures.
I am getting a lot of push back when questioning our administrators on the gowns we are using as they appear to be level 1 gowns. They are of the firm belief that they are sufficient for caring for patients being swabbed and given the amount of coughing and sneezing I do not believe this to be the case.
Can anyone provide some high quality evidence to push back on this?
I looked at our yellow see through gowns and there were no specs (apart from made in China).
Is there a way to tell which gowns are Level 1 and which are Level 2?
Fantastic job by everyone and many many thanks.
Robert Hutton