In this ECG Cases – Missed Ischemia – Never Trust the ECG Computer Interpretation, we review ECGs from 7 patients presenting to the ED with chest pain, all of whom had a computer interpretation as “normal.” And guess what…they all show acute ischemia! Can you see what the computer couldn’t?
Written by Jesse McLaren; Edited by Anton Helman. September 2019
ECG Cases 1: Missed Ischemia – Never Trust the ECG Computer Interpretation
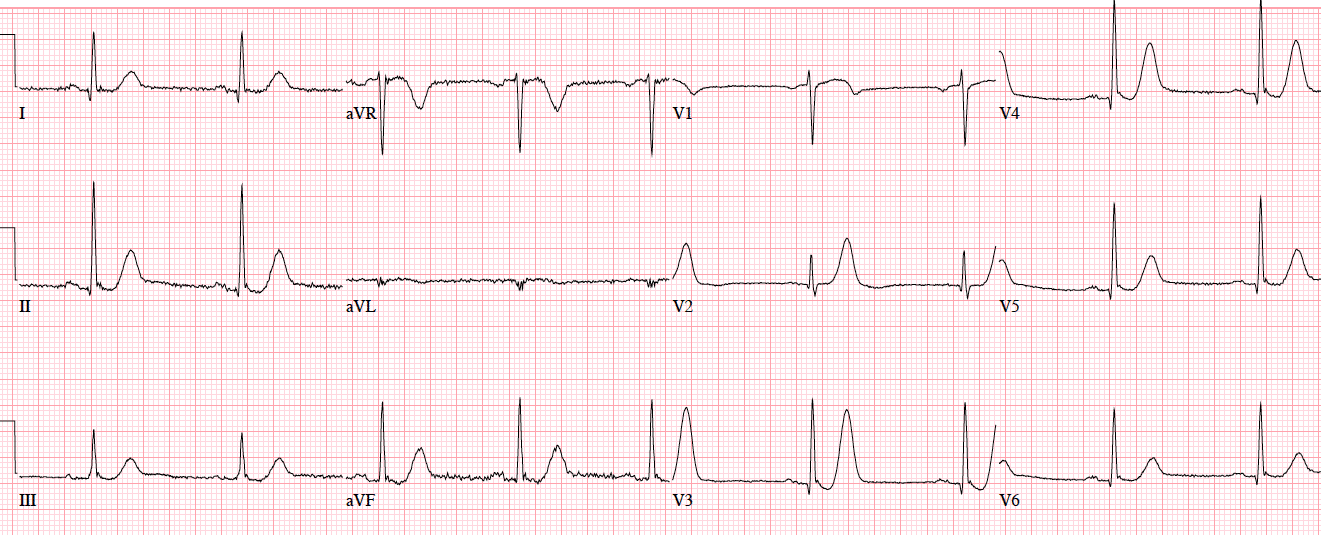
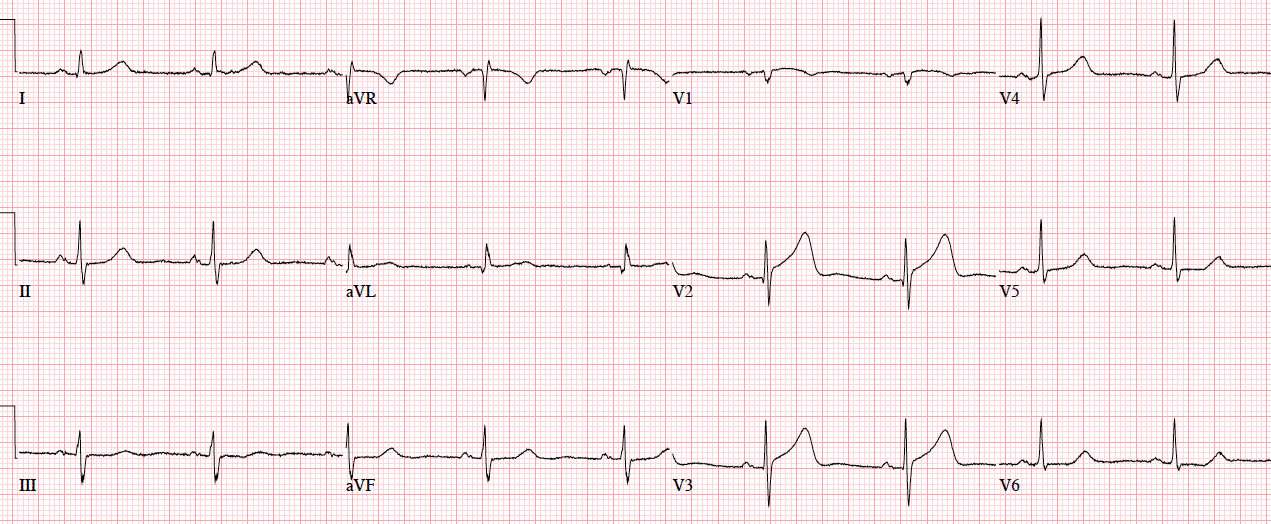
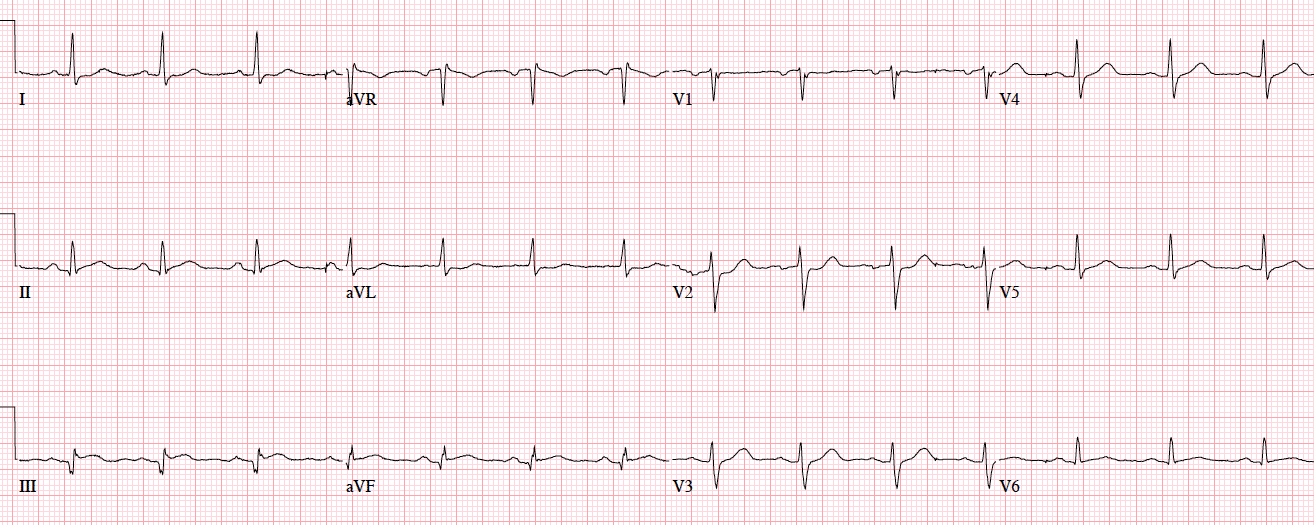
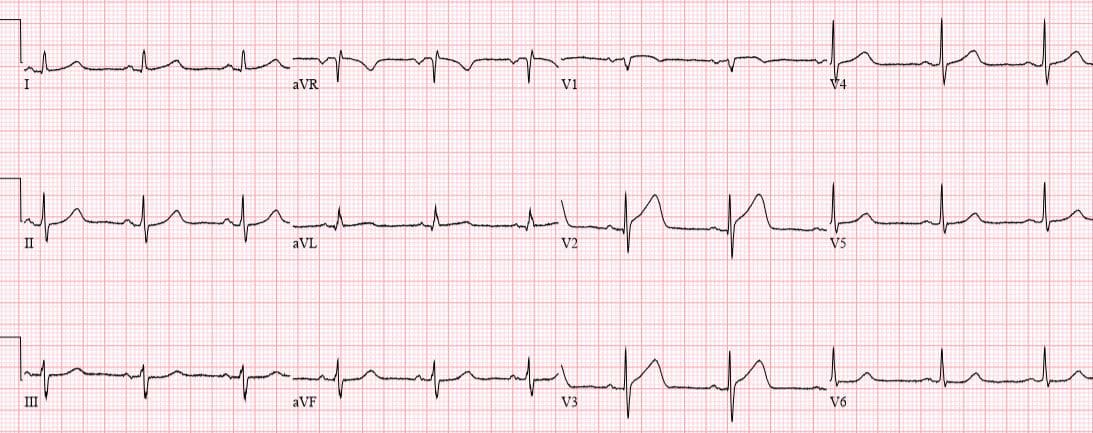
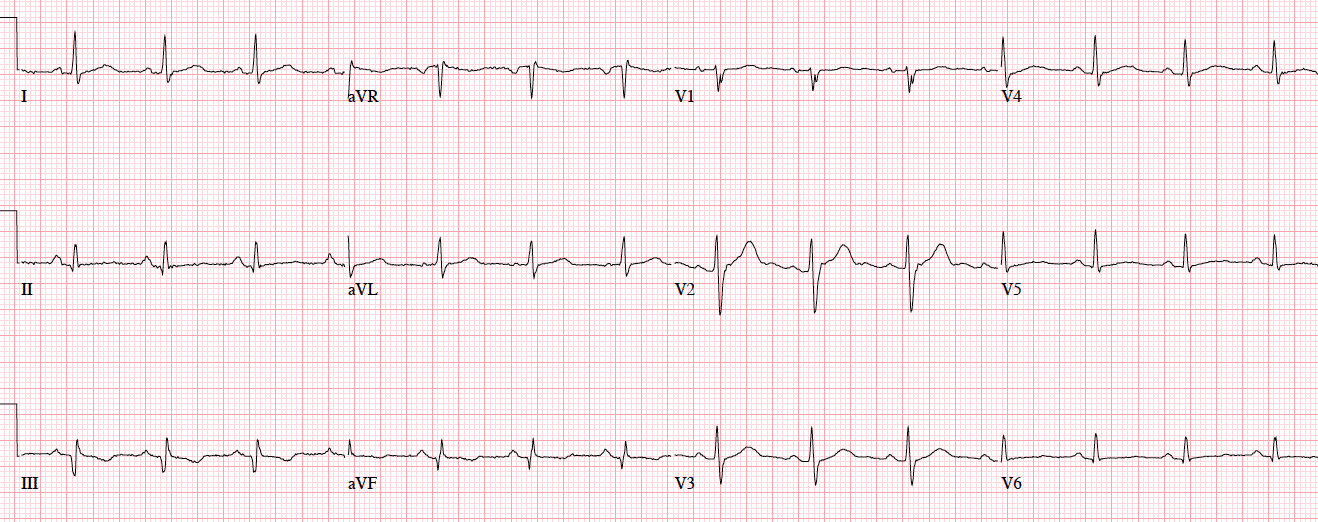
Patient 1. 65yo with hours of chest pain. No prior ECG
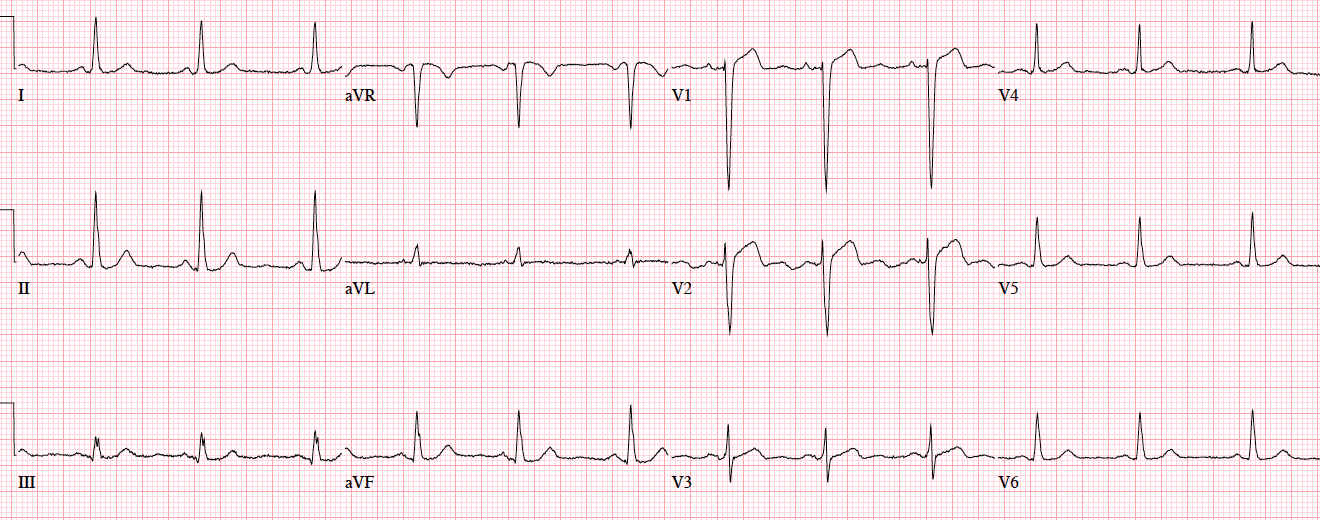
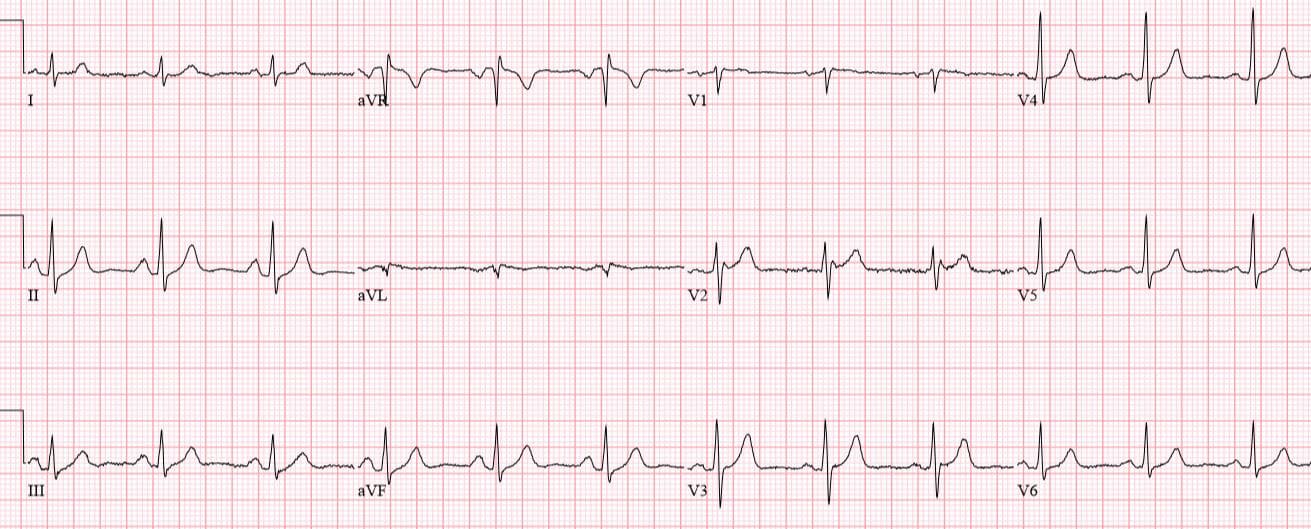
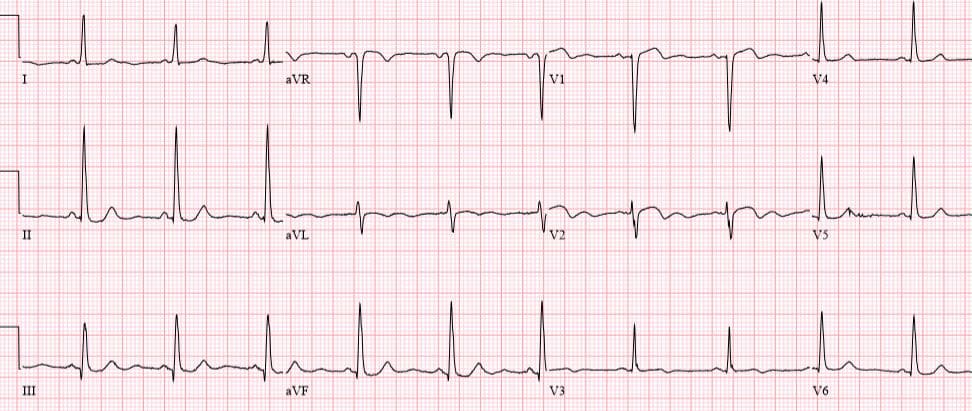
Patient 2: 50yo with 3hrs of mid-sternal squeezing chest pain with diaphoresis. No prior ECG
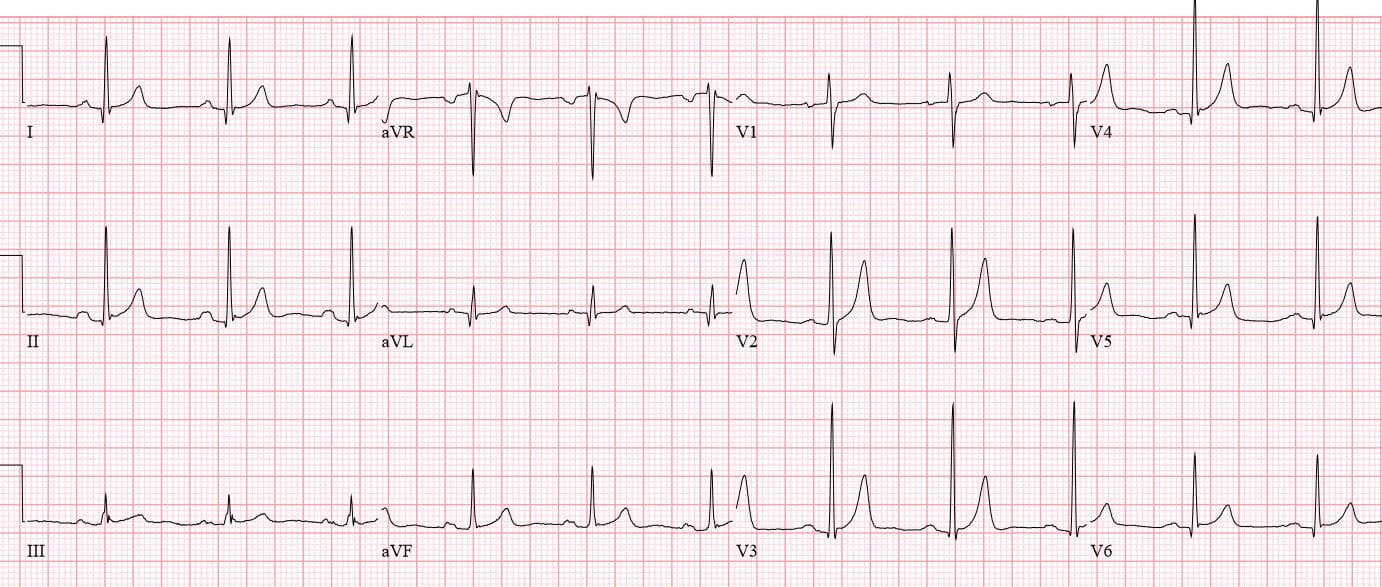
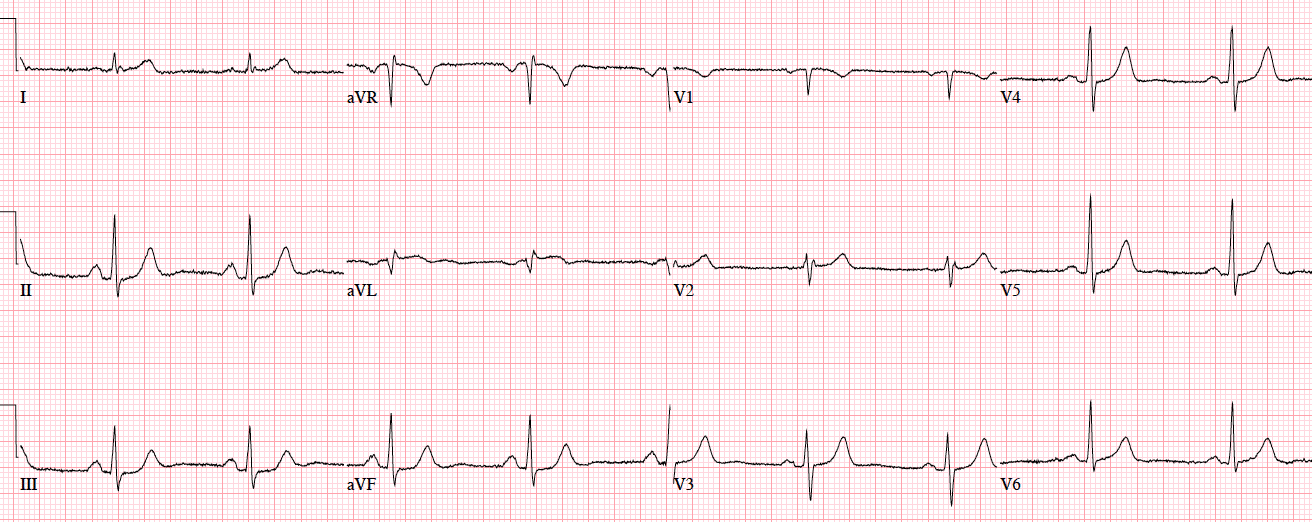
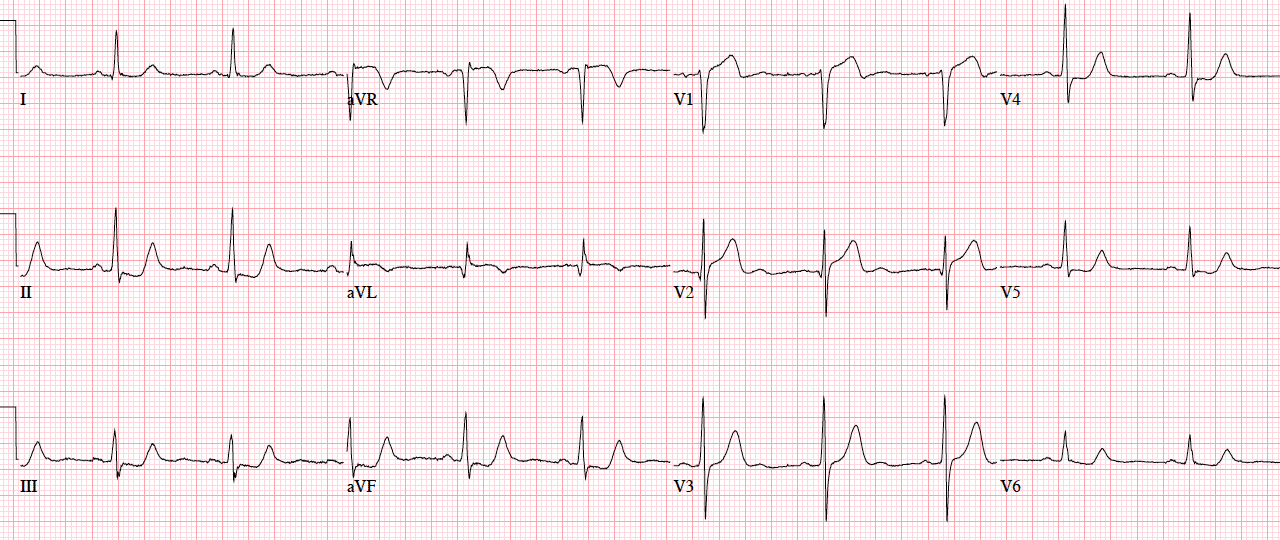
Patient 3. 70yo with 90 minutes exertional chest pain and nausea. No prior ECG
Patient 4: 70yo with one hour of exertional chest pain radiating to the arm. Old then new ECG
Patient 5: 70yo with 6hrs on/off chest tightness radiating to the arm now constant. Old then new ECG
Patient 6: 75yo one day chest pain radiating to bilateral shoulders. Old then new ECG
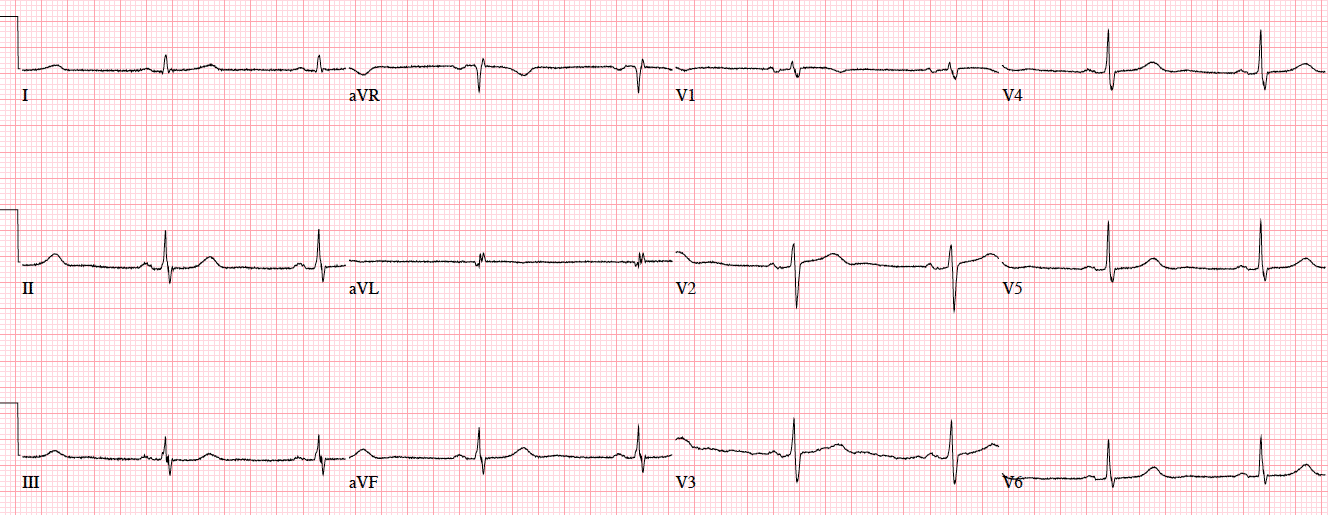
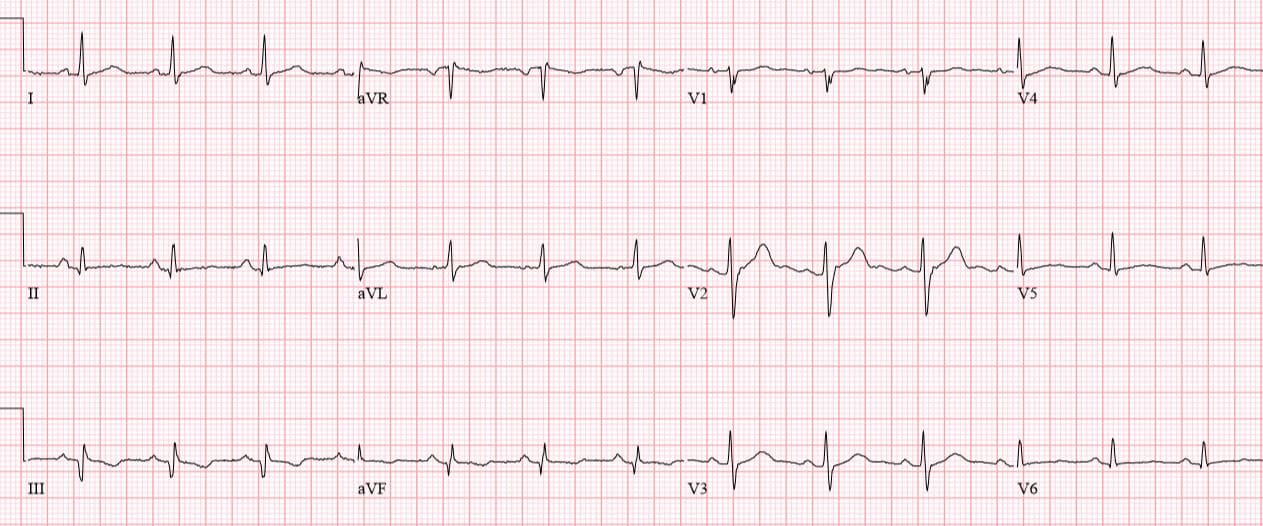
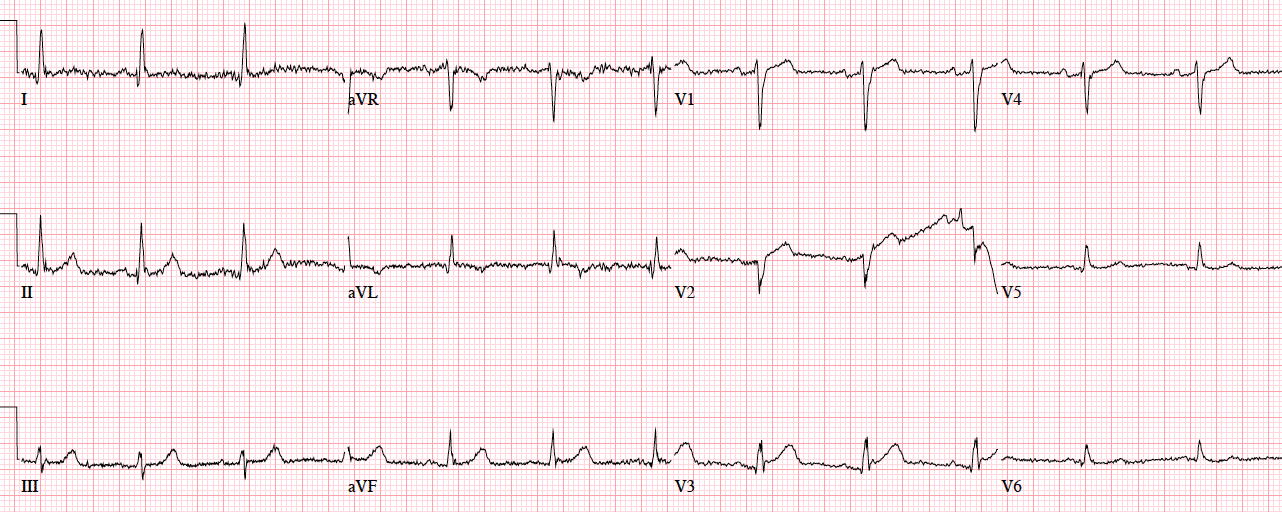
Patient 7: 55yo history RCA stent with 30 minutes chest pain radiating to the arm. Old then new ECG
ECGs read as ‘normal’ by the computer
Automated interpretation has high rates of error for detecting ischemia, up to 42% for STEMI.[1] But what about those ECGs read as “normal”? A 2017 study concluded that “triage ECGs identified by the computer as normal are unlikely to have clinical significance that would change triage care. Eliminating physician review of triage ECGs with a computer interpretation of normal may be a safe way to improve patient care by decreasing physician interruptions.” [2]
But this was based on only 4 months of triage ECGs collected at a single centre with a low incidence of STEMI. A critical response explained both the shortcomings of the study, and a different approach to “normal” ECGs:
“Using non-blinded expert review rather than outcome as a reference standard precludes any meaningful conclusion about triage ECGs…A sample size of 855 has no chance of generating a meaningful conclusion about the reliability of computer ‘Normal.’…Physicians should take steps to develop their skills in detecting subtle signs of myocardial ischemia, and computerized interpretation algorithms should state ‘No abnormalities detected’ rather than ‘Normal ECG.’ ” [3]
Back to the cases
Patient 1. ischemic ST morphology
NSR, normal conduction/axis/R wave, no hypertrophy. Mild ST elevation in V1-2 which could be normal, but the morphology is not: ST is convex in V2 and straight in V3. Plus there’s an inverted U wave in V2, another marker of LAD occlusion. When trop returned positive an hour later, repeat ECG below showed further convex ST in V1-2 and terminal T wave inversion, and cath lab was activated: 100% mid LAD occlusion
Patient 2: ischemic T wave morphology
NSR, normal conduction/axis/R wave, no hypertrophy. No ST segment elevation or depression, but there is terminal T-wave inversion in aVL and reciprocal down-up T waves in III/III/aVF, and inverted U wave in V2-3. The physician was concerned about these and asked for a repeat ECG:
Now there is ST elevation in V1-2 and aVL, a deeper Q wave in aVL and new Q wave in V2, and ST depression inferolaterally. Code STEMI called: 95% proximal LAD occlusion
Patient 3. subtle LAD occlusion
NSR, normal conduction/axis, no hypertrophy.There is 1-2mm concave ST elevation in V2-3 which could be normal, but there are a number ischemic changes: reverse R wave progression from V2 to V3, Q wave in V2, terminal QRS distortion (no S wave or J wave) in V2, hyperacute T waves (relative to their preceding QRS) in V2-3, and inferior reciprocal changes. When trop came back positive an hour later, a repeat ECG was done:
Now there is a full QS wave in V2. Code STEMI called: 100% mid-LAD occlusion.
Patient 4: subtle LAD occlusion
NSR, normal conduction/axis/R wave progression, no hypertrophy. Compared to the old ECG there is no ST elevation, but there are three other signs of occlusion: hyperacute T waves (now bigger than the R wave in V2 and as big as the R wave in V3), a deeper Q wave in V3, and terminal QRS distortion in V3. Physician asked for a repeat ECG
Patient 5: ST/T changes compared to prior
There’s mild concave ST elevation in lead V2-3 which doesn’t meet STEMI criteria. But this is new compared to previous, along with hyperacute T waves in V2-3 and mild ST depression laterally. When trop came back positive an hour later, repeat ECG below showed straightening of the ST segments, and the cath lab was activated: 100% distal LAD occlusion.
Patient 6: subtle circumflex occlusion
There’s barely 1mm of ST elevation in aVL only (no STEMI criteria), but this is large compared to its small QRS complex, and there’s mild reciprocal ST depression inferiorly, and pseudonormalized ST segment in V3. Concerned about the patient’s symptoms and the new ischemic changes, the physician activated the cath lab: circumflex occlusion.
Patient 7: subtle RCA occlusion.
NSR, normal conduction/axis, R wave, no hypertrophy. There’s an old Q wave from the prior MI. But there is now mild ST elevation in III/AVF with reciprocal ST depression in aVL (which is very sensitive for inferior MI), the inverted T waves in III/aVF are now upright (pseudonormalization), and there is relative ST depression (pseudonormalization) in V2–all concerning for posterolateral ischemia. Cath lab activated: 100% occlusion at the stent. First trop negative, peak 8,000.
Take home points for Missed Ischemia Never Trust the ECT Computer Interpretation
Never trust the ECG computer interpretation, even if it says “normal,” because:
- ischemic morphology: the computer focuses on ST segment elevation, and can miss ischemic ST-T wave morphology—including straight or convex ST segments, terminal T wave inversion, down-up T waves, hyperacute T waves, deWinter T waves, and inverted U waves
- dynamic change: the computer interprets each ECG in isolation, and can’t compare to prior or repeat ECGs (which is critical in a dynamic process like coronary occlusion)—so it can miss subtle changes, including pseudonormalization of ST segments or T waves
- STEMI criteria: computer interpretation is based on STEMI criteria, which has limited sensitivity for identifying acute coronary occlusion—so it can miss subtle ST elevation (which may be significant in small amplitude QRS complexes), ST depression in aVL (which is very sensitive for inferior MI), and subtle signs of LAD occlusion like terminal QRS distortion.
This blog will explore all these signs in more detail, and more.
References for Missed Ischemia Never Trust The ECG Computer Interpretation
- Schläpfer J, Wellens HJ. Computer-Interpreted Electrocardiograms: Benefits and Limitations. J Am Coll Cardiol. 2017;70(9):1183-1192.
- Hughes KE, Lewis SM, Katz L, Jones J. Safety of Computer Interpretation of Normal Triage Electrocardiograms. Acad Emerg Med. 2017;24(1):120-124.
- Litell JM, Meyers HP, Smith SW. Emergency physicians should be shown all triage ECGs, even those with a computer interpretation of “Normal”. J Electrocardiol. 2019;54:79-81.








Hi Anton,
WOW, is all I can say for this first ECG tutorial.
Brilliant addition.
Sean.
EXCELLENT series of subtle but super important ECGs and interpretation by Dr. McLaren. These cases would each be headliners on Dr. Smith’s ECG Blog. So glad there are others out there putting out this level of content. Thank you Dr. McLaren
Thanks to Dr. Smith’s ECG blog (and Dr. Meyers’ OMI manifesto) for leading the way, so that others can follow!
Nice post! That said — the point I emphasize is that the “fault” should not lie with the computer (which only does what it is programmed to do — and which cannot compare tracings, and which can’t take a history …). Instead, the fault lies with the interpreter who looks at the computerized ECG interpretation BEFORE he/she makes their own independent interpretation of what the ECG shows IN CONTEXT with the clinical situation. There ARE things that the computer does well (ie, measure intervals, axis, rates — and speed up ambulatory interpretation by experts given “stacks” of tracings to overread). What the computer does NOT do well is pick up subtle (and sometimes not so subtle) acute ischemia or infarction — and in my experience it is equally unreliable in detection of ANY rhythm other than sinus. But all emergency providers should KNOW this before they pick up the ECG. Seeing these cases as shown by Drs. McLaren and Helman serves well to remind emergency providers that it is their RESPONSIBILITY to independently interpret each ECG they are given BEFORE ever looking at what the computer said. Otherwise — I’ll offer a different opinion on ECG #1 — in that while I’d remain very open to the definite possibility of an acute cardiac event in this 65yo with “hours” of chest pain because of more-than-the-usual amount of ST elevation in V1 + ST coving in V2 + ST segment straightening in V3 — there IS on this ECG, criteria for LVH (ie, very deep S wave in lead V1 + an ST segment “shape” in V1,V2 perfectly consistent with LV “strain” when you have deep anterior S waves) — so in my opinion, while this 1st ECG in Patient #1 is suspicious (and this patient needs careful additional evaluation), this ECG is NOT by itself “diagnostic” of acute ischemia. The 2nd ECG on this Patient #1 of course became diagnostic. (Initial ECGs from the other 6 patients should all suggest acute ischemia to experienced interpreters.) Finally — Computerized programs vary in their “abilities” (accuracy) — so if the computerized interpretation for each of the 7 initial tracings from these 7 patients simply said “normal” without any other relevant comment — then, one might search for a different company’s computerized program to use in their institution. Again — Our THANKS to Drs. McLaren and Helman for these 7 illustrative ECG case studies that confirm the need for independent interpretation of all ECGs seen by emergency providers.
Great points, thanks!
Great write
Believe only in intervals and rates
To err is human
To repeatedly err is machines and computers
What a fantastic addition to the already excellent blog (or should I start saying platform with the progressive expansion of the site?)! Huge thanks to Dr Jesse McLaren and Dr Anton Helman. Looking forward to the future posts with anticipation!
Highly informative and the take home concisely delivered. Thanks to Dr Anton Helman and Dr Jesse.
thanks for a great article by Dr. Jesse McLaren