Topics in this EM Quick Hits podcast
Anand Swaminathan on lateral canthotomy (0:54)
Emily Austin on pediatric cannabis poisoning (7:38)
Reuben Strayer on an approach to hyperthermia (13:22)
Brit Long on diagnosis and management of malignant otitis externa (20:28)
Jesse McLaren on ECG diagnosis of occlusion MI in patients with BBB (25:42)
Peter Brindley on prone CPR (32:15)
Podcast production, editing and sound design by Anton Helman. Voice Editing by Raymond Cho.
Podcast content, written summary & blog post by Anton Helman, Emily Austin, Brit Long and Reuben Strayer
Cite this podcast as: Helman, A. Swaminathan, A. Austin, E. Strayer, R. Long, B, McLaren, J. Brindley, P. EM Quick Hits 24 – Lateral Canthotomy, Cannabis Poisoning, Hyperthermia, Malignant Otitis Externa, BBB in Occlusion MI, Prone CPR. Emergency Medicine Cases. December, 2020. https://emergencymedicinecases.com/em-quick-hits-december-2020/. Accessed [date].
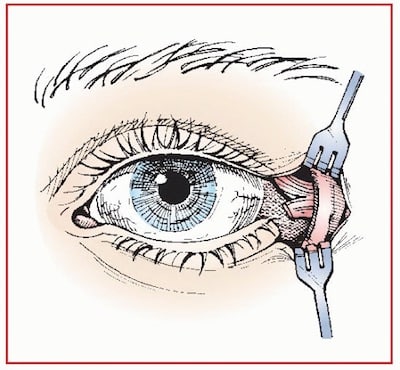
Lateral canthotomy – cantholysis
-
Time is eye; a lateral canthotomy is indicated for trauma patients with orbital compartment syndrome within 60-120 minutes of onset of ischemic features (decreased visual acuity and RAPD) as a temporizing measure to definitive surgical evacuation of the retrobulbar hematoma.
-
Clinical clues to orbital compartment syndrome include mechanical consequences (proptosis from the retrobulbar hematoma – most easily seen from the head of the bed with the patient lying supine – IOP>40mmHg and impaired extraocular movements), and ischemic consequences (decreased visual acuity, RAPD and a blown pupil)
-
Do not wait for a CT to confirm a retrobulbar hematoma; the clinical diagnosis is all you need to go ahead with the procedure
-
Gear: 2% Lidocaine with Epinephrine, 25g needle, straight clamp, iris scissors, toothed forceps
- The lateral canthotomy procedure
-
- Ensure adequate sedation and local anesthesia
- Crush and clamp the lateral canthus for 1-2 minutes with the straight clamp
- Make a 1-1.5cm cut to the lateral canthus with the iris scissors while an assistant is pulling the lower lid out of the way with toothed forceps
- Palpate the lateral canthal ligament (because the surgical field is usually very bloody, finding the lateral canthus ligament becomes a tactile procedure and has been likened to the feel of a guitar string) and cut the inferior branch of the lateral canthal ligament
- Recheck the IOP; if still elevated cut the superior branch of the lateral canthal ligament
-
Medical treatment for OCS is similar to that of acute angle closure glaucoma with mannitol, acetazolamide, pilocarpine and timolol.
Traumatic retrobulbar hemorrhage: Emergent decompression by lateral canthotomy and cantholysis paper
- Vassallo, S., Hartstein, M., Howard, D., & Stetz, J. (2002). Traumatic retrobulbar hemorrhage: Emergent decompression by lateral canthotomy and cantholysis. The Journal of Emergency Medicine, 22(3), 251-256.
- Helman, A, MacDonald, A, Chenkin, J, Simard, R, Himmel, W. Blunt Ocular Trauma Live from The EM Cases Course. Emergency Medicine Cases. February, 2018. https://emergencymedicinecases.com/ocular-trauma/
Pediatric cannabis poisoning
- Young children are exposed to cannabis most often through exploratory ingestion of cannabis edibles
- These exposures result in a different symptom profile compared to adults: children may present with vomiting, agitation, lethargy, and coma (amongst other symptoms)
- In a systematic review, admission to the ICU was not uncommon, and a small percentage of patients required intubation
- Urine drug screens for cannabinoid metabolites are not necessary if the history is clear and have false positives which may be misleading
- Your duty to report to child protection services is no different than in any other case: if you have concerns that a child is experiencing physical, sexual and/or emotional abuse and neglect
- Richards, J. R., Smith, N. E., & Moulin, A. K. (2017). Unintentional cannabis ingestion in children: A systematic review. The Journal of Pediatrics, 190, 142-152.
- Kim, H. S., & Monte, A. A. (2016). Colorado cannabis legalization and its effect on emergency care. Annals of Emergency Medicine, 68(1), 71-75.
An ED approach to hyperthermia

From Emergency Medicine Updates https://emupdates.com/hot/
- Strayer, R. Emergent Management of Hyperthermia. Emergency Medicine Updates. Accessed December 4th, 2020.
Malignant otitis externa – Pearls in diagnosis and management
- Malignant otitis externa, or necrotizing otitis externa, is a rare disease associated with osteomyelitis of the skull base, which may result in cranial nerve deficit, abscess, and death.
- Consider malignant otitis externa in patients with severe pain and/or severe otorrhea with a history of diabetes, immunocompromised state or age > 65 years
- Most patients are afebrile
- Perform a careful exam for cranial nerve deficits. CN VII palsy may occur in 25% of patients
- Pseudomonas is the most common etiology, but MRSA accounts for 15% of cases; fungal species such as aspergillus and candida may be the causative agent, most commonly in AIDS
- WBC is typically normal, but ESR and CRP are usually elevated; the most important lab test is a culture of the swabbed purulent material
- Obtain CT with IV contrast as your first line imaging modality, but this may be negative in early disease. MRI imaging can detect soft tissue changes
- Consult ENT and Infectious Disease; antibiotics with pseudomonas coverage are vital
Further Reading: EMdocs Malignant Otitis Externa Diagnosis & Treatment
- Chandler JR. Malignant external otitis. 1968 Aug;78(8):1257–1294.
- Roland PS & Stroman DW. The microbiology of acute otitis external. 2002: 112(7):1166-77.
- Rubin Grandis J, Branstetter BF 4th, Yu VL. The changing face of malignant (necrotising) external otitis: clinical, radiological, and anatomic correlations. Lancet Infect Dis. 2004; 4(1):34-9.
- Weinroth SE, Schüssel D, Tuazon CU. Malignant otitis externa in AIDS patients: case report and review of the literature. Ear Nose Throat Journal. 1994;73(10):772-4, 777-8.
- Tarazi AE, Al-Tawfiq JA, Abdi RF. Fungal malignant otitis externa: pitfalls, diagnosis and treatment. Otol Neurotol.2012; 33(5):769-73.
- Chen CN, Chen YS, Yeh TH, Hsu CJ, Teng FY. Outcomes of malignant external otitis: survival vs mortality.Acta otolaryngol. 2010;130(1):89-94.
- Mani N, Sudhoff H, Rajagopal S, Moffat D, Axon PR. Cranial nerve involvement in malignant external otitis: implications for clinical outcome. 2007;117(5):907-10.
ECG diagnosis of occlusion MI in patients with RBBB or LBBB
- RBBB is a high risk feature in occlusion MI, especially if new and accompanied by LAFB. If a patient has ischemic symptoms and RBBB, compare with prior to see if this is new, and look for associated fascicular blocks and ST changes
- Anterior leads with RSR’ should have discordant ST/T changes, so concordant elevation or excessively discordant depression can be a sign of occlusion, while other leads will not have repolarization abnormalities. Finding the end of the QRS can identify ST changes.
- Use the Smith-modified Sgarbossa criteria (concordant STE/STD, or excessively discordant STE/S >25% or STD/R>30%) to identify occlusion MI in the patient with ischemic symptoms and LBBB (whether new or old)
- Treat the patient: those with refractory ischemia and hemodynamic instability from suspected occlusion MI require cath lab activation regardless of the ECG
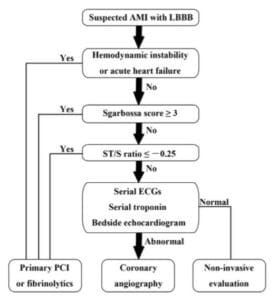
Smith-modified Sgarbossa Criteria for occlusion MI in the setting of LBBB
Further Reading and interpretation skills practice:
ECG Cases 12: RBBB and Occlusion MI
ECG Cases 11: LBBB and Occlusion MI
- Neumann JT, Sorensen NA, Rubsamen N, et al. Right bundle branch block in patients with suspected myocardial infarction. Eur Heart J Acute Cardiovasc Care 2019 Mar;8(2):161-166
- Smith SW, Dodd KW, Henry TD et al. Diagnosis of ST-elevation myocardial infarction in the presence of left bundle branch block with the ST-elevation to S-wave ration in a modified Sgarbossa rule. Ann Emerg Med 2012 Dec;60(6):766-776
- Meyers HP, Limkakeng AT, Jaffa EJ, et al. Validation of the modified Sgarbossa criteria for acute coronary occlusion in the setting of left bundle branch block: a retrospective case-control study. Am Heart J 2015 Dec;170(6):1255-64
- Ibanez B, James S, Agewall S. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J 2017 Jan;39(2):1119-177
Prone CPR early studies: Should prone chest compressions be performed in the first 2-3 minutes of CPR in a patient who is found to be in cardiac arrest in the prone position?
- Prone cardiac arrests may be increasingly encountered with ARDS and COVID pneumonia patients being proned as part of their management
- The 2010 AHA guidelines recommend “when patients cannot be placed in the supine position, it may be reasonable for rescuers to provide CPR in the prone position, particularly in hospitalized patients with an advanced airway”.
- The UK Resuscitation Council recommends starting chest compressions without changing the position for adult patients who arrest during neurosurgery
- A literature review of 24 studies in 2020 found 4 peer-reviewed studies looking at prone cardiopulmonary resuscitation:
- An ICU feasibility study of blood pressure during supine versus prone compressions – SBP improved 48 mmHg–72 mmHg, MAP from 32 mmHg to 46 mmHg from supine to prone
- A study of cadavers and healthy volunteers on BP and tidal volumes generated by prone compressions – prone CPR resulted in SBP 79.4 ± 20.3 mmHg, and DBP 16.7 ± 10.3 mmHg vs supine CPR produced increase in SBP of 55.4 ± 20.3/13.0 ± 6.7 mmHg to (79 ± 20/17 ± 10) (P = 0.028)
- A prone compression quality manikin study – 3376 chest compressions: 1168 (34.6%) effective (4–5 cm compression), 1370 (40.6%) partially effective (2–4 cm), 838 (24.6%) ineffective (<2 cm depth). 22/36 (61%) nurses able to deliver effective compressions (mean of 53% compressions were effective). Wide variations in compression effectiveness.
- A retrospective descriptive study of chest CT scans of 100 patients to identify ideal prone compression hand position – largest LV cross-sectional area is 0–2 vertebral segments below inferior angle of the scapulae in 86% of proned patients
- Recommended compression location: 0-2 vertebral segments below the the inferior angle of the scapulae (see image)
- There is currently a lack of moderate to high-level evidence for prone chest compressions in adult cardiac arrest; patient-oriented outcomes compared to supine chest compressions have not been adequately studied.
- On a case-by-case basis, it is currently not unreasonable to start chest compressions in the prone position of a patient who is found to be in cardiac arrest in the prone position, however further studies are required before it can be recommended or dissuaded for all prone cardiac arrest patients

Suggested location of hand position for chest compressions in the prone patient 0-2 vertebral segments below the the inferior angle of the scapula
- Douma MJ, MacKenzie E, Loch T, Tan MC, Anderson D, Picard C, Milovanovic L, O’Dochartaigh D, Brindley PG. Prone cardiopulmonary resuscitation: A scoping and expanded grey literature review for the COVID-19 pandemic. Resuscitation. 2020 Oct;155:103-111.
-
D.M. Cave, R.J. Gazmuri, C.W. Otto, et al. Part 7: CPR techniques and devices: 2010 American heart association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation, 122 (2010), pp. S720-728.
-
C. Carroll, R. Davies, C. Gwinnutt, I. Kamaly-Asl, J. Soar. Management of cardiac arrest during neurosurgery in adults. (2014).
-
M.-J. Kwon, E.-H. Kim, I.-K. Song, J.-H. Lee, E.-H. Kim, J.-T. Kim. Optimizing prone cardiopulmonary resuscitation: identifying the vertebral level correlating with the largest left ventricle cross-sectional area via computed tomography scan. Anesth Analg, 124 (2017), pp. 520-523,
None of the authors have any conflicts of interest to declare




Superb knowledge gained thanks