In this ECG Cases blog we examine 6 patients who presented with poor R wave progression, and a mnemonic for the differential
Written by Jesse McLaren; Peer Reviewed and edited by Anton Helman. December 2020
Six patients presented with poor R wave progression. Can you get the diagnosis based on the LATE mnemonic?
Case 1: 70yo previously well with one month of fatigue, normal vitals
Case 2: 90yo previously well with one month SOBOE and bipedal edema. Old then new ECG:
Case 3: 85yo history of HTN and inferior MI with one day of SOB. Old then new ECG
Case 4: 70yo with 5 hours of chest pain. Old then new ECG
Case 5: 50yo previously well with 2 hours of chest pain. Went to clinic (first ECG) and then ED (second ECG, one hour later)
Case 6: 70yo with 2 hours chest pain radiating to arms, with nausea/diaphoresis/SOB
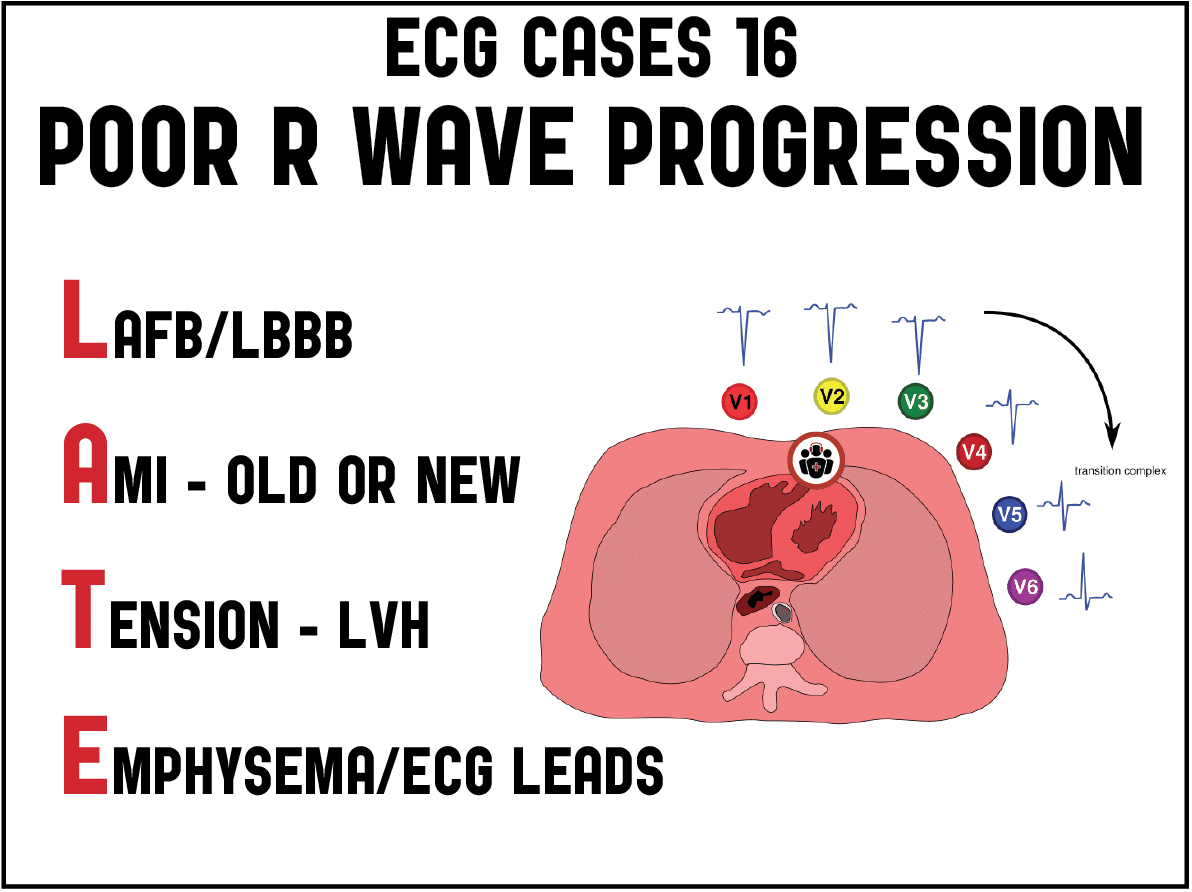
Poor R-wave progression and the LATE mnemonic
Ventricular depolarization begins in the septum, where it proceeds from left to right. Then the ventricles depolarize simultaneously, but because of the greater mass of the left ventricle the sum of electrical vectors is directed leftwards. So the right sided lead V1 has an rS wave: small positive R wave from septal depolarization and large negative S wave from left ventricular dominance. Moving across the precordium towards the left ventricle, the amplitude of the R wave increases and S wave decreases. The transition point, where R>S, is usually at V3-4. Poor wave progression has been variably defined as the failure to of the R wave to progress in amplitude (R<3mm in V3), reversal of the progression (eg R in V2>V3), or delayed transition beyond V4. There are electrical, ischemic, structural, pulmonary and technical causes of poor (or late) R wave progression—and the differential can be remembered by the mnemonic LATE:
- LAFB, LBBB: when the left anterior fascicle is blocked, conduction goes more posterior, with a later transition; when the entire left bundle is blocked septal depolarization is reversed and goes from right to left, with loss of anterior R waves
- AMI – old or new: an old anterior infarct (or pseudo-infarct patterns from other cardiomyopathies) can leave small R waves or complete Q waves, but these can also be seen in early acute ischemia.
- Tension – LVH: a large left ventricular mass can result in net diminished forces in right sided leads
- Emphysema, ECG lead placement: high lead placement may produce small R waves, either because the leads themselves are placed too high on the chest (or the leads are switched, eg V1 and V3), or because hyperinflation from emphysema lowers the diaphragm and heart.
Because of multiple causes, including normal variation, the presence of poor R wave progression in isolation on a baseline ECG is not a helpful finding in predicting prior anterior MI.[1] But for those diagnosed with anterior MI, poor R wave progression correlates with larger infarct size and lower LV function [2]. In addition, the sudden development of poor R wave progression can be a sign of acute coronary occlusion. As explained in Critical Decisions in Emergency Medicine and Acute Care Electrocardiography, “the presence of Q waves at the time of presentation in acute MI may be due to prior MI or due to early formation during acute MI. In acute anterior MI, Q waves are frequently due to ischemia and injury of the conducting system, as opposed to (irreversible) infarction, and appear within 1 hour of onset of symptoms in 50% of cases, and rapidly resolve with reperfusion…With anterior MI, there is similar loss of R wave voltage in the precordial leads, seen as a Q wave equivalent. Patients with diminished total R wave voltage have significantly reduced LV dysfunction and a worse prognosis.” Whereas STEMI criteria only focus on ST-segments in isolation, signs of occlusion MI (OMI) include acute Q waves or new loss of R waves (or new tall R waves from posterior MI). Examining the QRS complex before the ST segment and T waves also generates a reference point to determine disproportionate ST changes or hyperacute T waves.
Back to the cases
Case 1: lead misplacement
- Heart rate/rhythm: NSR
- Electrical conduction: normal
- Axis: normal
- R wave size/progression: normal R wave progression except for V3
- Tension: no hypertrophy
- ST/T: no changes other than entire complex inverted in V3
Impression: lead V3 misplaced, labeled as “anterior infarct” by computer. Repeat ECG normal and normal labs, patient discharged
Case 2: cardiac amyloid
- H: new Afib
- E: otherwise normal intervals
- A: left axis from inferior infarct
- R: poor R wave progression with anterior Q waves and transition shifting from V4 to V6, and loss of R waves in limb leads
- T: no hypertrophy
- S: no hyperacute T waves, mild lateral TWI
Impression: extensive non-acute infarct pattern, corresponding with one month of CHF symptoms. Global hypokinesis on echo with EF 25%. Cardiac MR diagnosed amyloid, which classically presents with Afib, low voltage and pseudo-infarct pattern.
Case 3: LVH with LAD occlusion, STEMI(-) OMI(+)
- H: sinus tach
- E: normal conduction
- A: normal axis
- R: new loss of anterior R waves V1-4, transition shifted from V4 to V5; regained inferior R waves after old inferior MI
- T: LVH
- S: new anterior ST elevation, and lateral T wave inversion more symmetric and deeper than baseline
Impression: LVH can produce chronic poor R wave progression and lateral T wave inversion, but here the poor R wave progression is from acute loss of R waves accompanied by new ST elevation and greater T wave inversion. So this is LVH plus occlusion MI. Cath lab activated: 95% LAD occlusion, Trop I rose from 1,800 to 9,000.
Discharge ECG had reappearance of R waves and reperfusion T wave inversion in anterior leads, and return of baseline lateral T wave inversion:
Follow up ECG months later had greater recovery of R waves and resolution of T wave inversion, but R waves less than baseline and with reverse progression From V2-3
Case 4: LAD occlusion, STEMI(-) OMI(+)
- H: sinus brady
- E: old LAFB and U waves (best seen in inferior leads)
- A: left
- R: new loss of R wave progression, including anterior Q waves and transition point at V6
- T: no hypertroaphy
- S: minimal ST elevation aVR/V1-2, hyperacute T waves V1-4, and lateral ST depression
Impression: LAD occlusion. Stat cardiology: “not STEMI”, then activated cath lab when initial trop I returned at 150, repeat ECG unchanged. Cath: 99% proximal LAD occlusion, peak trop 50,000.
Discharge ECG: ongoing loss of anterior R waves, reperfusion T wave inversion:
Case 5: LAD occlusion, STEMI(-), OMI(+)
- H: sinus tach
- E: normal conduction
- A: left
- R: poor R wave progression with loss of R waves across the precordium, and inferior loss of R waves with fragmented QRS complexes
- T: no hypertrophy
- S: initial ECG had mild ST elevation V2-3 and hyperacute T waves V2-5, which resolved on the second ECG
Impression: loss of R waves could be old but definitely not “normal” as computer labels it, but the hyperacute T waves indicate acute coronary occlusion (T/QRS in V4 >> 0.36), and further confirmed by their dynamic change. Pain improved with ASA and nitro, first trop 75, repeat ECG:
Anterior and inferior T wave inversion representing reperfusion of wraparound LAD occlusion (but can’t be Wellens because of loss of R waves). Admitted as “NSTEMI”. Cath next day: 99% mid LAD occlusion, peak trop I of 20,000, EF 47%. Discharged diagnosis “STEMI”, discharge ECG showed deeper anterior reperfusion T wave inversion, and normalization of inferior T waves.
Case 6: LAD occlusion, STEMI(-) OMI(+)
- H: NSR
- E: normal conduction
- A: normal axis
- R: reverse R wave progression V2-3 with small Q wave in V2
- T: no hypertrophy
- S: hyperacute T wave V2-3 (as big as the entire QRS complex), with reciprocal down-up T wave in III
Impression: concerning symptoms with multiple signs of subtle of LAD occlusion, labeled “normal” by the computer and signed off by the physician. When the first trop I came back at 100, repeat ECG:
Now full QS wave in V2. Cath lab activated: 100% LAD occlusion, peak trop 8,000. Discharge ECG: reperfusion T wave inversion:
Follow up ECG months later had recovery of R wave but still reverse progression V2-3
Take home points for poor R-wave progression and the LATE mnemonic
- The differential for poor R wave progression is LATE: LAFB/LABB, AMI (old or new), Tension (LVH), Emphysema/ECG lead misplacement
- Acute loss of R wave progression can be a sign of occlusion MI, especially when combined with other features like new Q waves, ST elevation, hyperacute T waves, and reciprocal change
References for ECG Cases 16: poor R-wave progression – LATE mnemonic
- Gami AS, Holly TA, Rosenthal JE, et al. Electrocardiographic poor R-wave progression: analysis of multiple criteria reveals little usefulness. Am Heart J 2004;148(1):80-85.
- Kurisu S, Iwasaki T, Watanabe N, et al. Poor R-wave progression and myocardial infarct size after anterior myocardial infarction in the coronary intervention era. IJC Heart & Vasc 2015;7:106-109
- Brady WJ and Truwit JD, eds. Critical Decisions in Emergency Medicine and Acute Care Electrocardiography. Wiley-Blackwell, 2009. 218-219























Very important and useful. Thanks