Topics in this EM Quick Hits podcast
Anand Swaminathan on ED management of postpartum hemorrhage (00:55)
Justin Morgenstern on phenobarbital in pediatric status epilepticus (6:41)
Michelle Klaiman on managed alcohol programs (12:16)
Andrew Petrosoniak on traumatic cardiac arrest (19:42)
Brit Long on diagnosing cholangitis (27:53)
Bourke Tillman on ED approach to ARDS Part 1 (33:56)
Podcast production, editing and sound design by Anton Helman
Podcast written summary & blog post by
Anand Swaminathan, Michelle Klaiman, Andrew Petrosoniak & Anton Helman
Cite this podcast as: Helman, A. Swaminathan, A. Klaiman, M. Morgenstern J. Long, B. Tillman, B. Petrosoniak, A. EM Quick Hits 22 – Postpartum Hemorrhage, Phenobarbital in Status Epilepticus, Managed Alcohol Programs, Traumatic Cardiac Arrest, Cholangitis, ED Approach to ARDS. Emergency Medicine Cases. September, 2020. https://emergencymedicinecases.com/em-quick-hits-september-2020/. Accessed [date].
ED Approach to Postpartum Hemorrhage
- After delivery, don’t forget about mom to focus on the baby. Look for bleeding and initiate aggressive management early.
- Postpartum hemorrhage is defined as > 500 cc of bleeding after delivery. If it looks like there’s a lot of blood, start resuscitation.
- Start with basic resuscitation – 2 large bore IVs, O2, Cardiac monitor, fluids and blood
- Once you recognize postpartum hemorrhage, rally your consultants immediately.
- Although there are a number of procedures the EP can perform to slow or stop bleeding, often, these patients will require further intervention
- Start by placing a call to obstetrics/gynecology but recognize that some patients will be amenable to interventional radiology (uterine artery embolization). If you don’t have OB/GYN, call your general surgeon.
- Uterine atony is the most common cause of postpartum hemorrhage
- Start with external uterine massage, progress to internal massage and consider packing.
- There are a number of medications that can stop bleeding in atony including oxytocin (1st line), misoprostol and methergine.
- Recognize other causes of postpartum hemorrhage if atony is not present
- Other causes include retained products of conception, trauma from delivery, uterine inversion, intrinsic bleeding disorders and DIC.
- Lew GH, Pulia MS: Emergency Childbirth, in Roberts JR, Hedges JR, Custalow CB, et al (eds): Clinical Procedures in Emergency Medicine, ed 6. Philadelphia, Saunders, 2013, Ch 56:p 1155-82.
Phenobarbital as 2nd line agent for pediatric status epilepticus
- A 2019 single center well done RCT out of South Africa showed that phenobarbital stops twice as many seizures and achieves a non-convulsive state more than twice as fast as phenytoin in children with status epilepticus, suggesting that after benzodiazepines, phenobarbital is the most appropriate second line option in status epilepticus
- Our expert suggests that propofol could be used a surrogate to phenobarbital in adults for those of us who are more familiar with the dosing and use of propofol
First10EM deep dive into the Burman trial
EM Cases Episode 133 Status Epilepticus
- Burman RJ, Ackermann S, Shapson-Coe A, Ndondo A, Buys H and Wilmshurst JM. A Comparison of Parenteral Phenobarbital vs. Parenteral Phenytoin as Second-Line Management for Pediatric Convulsive Status Epilepticus in a Resource-Limited Setting. Front. Neurol. 10:506, 2019.
- Lyttle MD, Rainford NEA, Gamble C, et al. Levetiracetam versus phenytoin for second-line treatment of paediatric convulsive status epilepticus (EcLiPSE): a multicentre, open-label, randomised trial. The Lancet. 2019.
- Dalziel SR, Borland ML, Furyk J, et al. Levetiracetam versus phenytoin for second-line treatment of convulsive status epilepticus in children (ConSEPT): an open-label, multicentre, randomised controlled trial. The Lancet. 2019.
Managed Alcohol Programs
- Managed alcohol programs (MAP), typically housed in homeless shelters, allow residents to drink alcohol in a monitored setting with a maximum hourly and daily limit – typically, one drink per hour, for a maximum of 15 drinks per day (average 6 per day)
- MAP is a form of harm reduction, and has been shown to improve overall health, reduce binge drinking and public intoxication, minimize the use of non-palatable forms of alcohol (e.g. hand-sanitizer, mouthwash), reduce ED visits, and is cost effective.
- During the COVID-19 Pandemic, patients who experience homelessness remained in the ED for several days waiting their COVID results, many who were at risk of leaving against medical advice due to the unwillingness to undergo alcohol detoxification
- The ED MAP, created during COVID, gave patients the option to remain in the ED without the need for forced detoxification
- MAP can be expanded to help a greater group of patients with severe alcohol use disorders who would normally not remain in hospital to complete their medical investigations or treatment due their fear of alcohol withdrawal.
- MAP should ideally use white wine or beer to avoid the use of red liquids that may mask a GI bleed.
Example MD order:
White wine, provide 4.5 oz between 0730-2230 PRN every 60-90 minutes maximum 15 units/day
Example MD order to minimize nursing contact for people under investigation for COVID-19:
White wine, provide 2-3 doses of 4.5 oz q3-4 hours between 0730-2230 PRN. Maximum 15 units/day
1 unit (serving) = 4.5 oz of wine at 11.5% (or equivalent)
- Canadian Institute for Substance Use Research. The Canadian Managed Alcohol Program Study (CMAPS). Victoria: University of Victoria; 2018. https://www.uvic.ca/research/centres/cisur/projects/map/index.php (accessed 29 January 2019).
- Alcohol harm in Canada: Examining hospitalizations entirely caused by alcohol and strategies to reduce alcohol harm. Ottawa: Canadian Institute for Health Information; 2017.
- Hammond, Gagne, Pauly & Stockwell, 2016. A Cost Benefit Analysis of a Canadian Managed Alcohol Program. CARBC
- Pauly BB, Gray E, Perkin K, et al. Finding safety: A pilot study of managed alcohol program participants’ perceptions of housing and quality of life. Harm Reduction Journal 2016; 13(1): 15.
Traumatic cardiac arrest
- Make sure cardiac ultrasound is part of your primary survey; there is a lot of value here and countless resources can be saved along with keeping your team safe if there is no cardiac activity; the evidence does not support continuing resuscitation
- Use shockable rhythm and witnessed arrest as at least supporting data points to help decide whether to continue resuscitation
- And de-prioritize CPR in favor of other more effective interventions
- For blunt cardiac arrests with cardiac motion, consider intubation, bilateral finger thoracostomies, blood products +/- pelvic binders if no severe head injuries
- Pre-arrest and intra-arrest prognostic factors associated with survival following traumatic out-of-hospital cardiac arrest – A systematic review and meta-analysis. Tran A, et al. Resuscitation. Vol 153, 119-135
- Western Trauma Association Critical Decisions in Trauma: Resuscitative thoracotomy. Burlew et al. J Trauma Acute Care Surg. 2012; 73: 1359-1364.
- Emergency Department Thoracotomy. Seamon et al. J Trauma. 79(1):159-173.
Cholangitis: Beyond Charcot’s Triad and Raynaud’s Pentad
- The sensitivity of Charcot’s Triad (jaundice, fever and right upper quadrant abdominal pain) is only about 25% and 5-7% for Raynaud’s Pentad (Charcot’s triad plus shock and altered mental status)
- Patients with cholangitis present similarly to cholecystitis but are usually sicker, appearing toxic, often with rigors and more often with jaundice
- Think about cholangitis in the older patient with sepsis and an occult source
- Bilirubin is usually significantly elevated
- Alkaline phosphatase (ALP) is elevated in >90% of patients
- CT is more accurate than ultrasound for the diagnosis of cholangitis with sensitivity and specificity >90% for CBD obstruction (ultrasound can miss cholangitis as the classic finding of ≥7mm CBD diameter is not always present, and patients with previous cholecystectomy often have dilated CBD at baseline; ultrasound sensitivity for CBD stones is only 25-60%)
- Tokyo Guidelines Diagnostic Criteria includes fever and/or rigors, WBC <4 or >10 x1,000/μL and/or CRP ≥1 mg/dL, total bilirubin ≥2 mg/dL, ALP, γGTP, AST, ALT levels >1.5 x STD, biliary dilatation on imaging, evidence of stricture, stone or stent on imaging with a sensitivity of 90% and sensitivity of 80% for diagnosis of cholangitis
- Ely R,Long B, Koyfman A. The Emergency Medicine-Focused Review of Cholangitis. J Emerg Med. 2018 Jan;54(1):64-72.
- Yokoe M, Takada T, Mayumi T, et al. Accuracy of the Tokyo Guidelines for the diagnosis of acute cholangitis and cholecystitis taking into consideration the clinical practice pattern in Japan. J Hepatobiliary Pancreat Sci 2011;18:250–7.
- Kiriyama S, Takada T, Strasberg SM, et al. New diagnostic criteria and severity assessment of acute cholangitis in revised Tokyo guidelines. J Hepatobiliary Pancreat Sci 2012;19:548–56.
- Kiriyama S, Takada T, Strasberg SM, Solomkin JS, Mayumi T, Pitt HA, et al. TG13 guidelines for diagnosis and severity grading of acute cholangitis (with videos). J Hepatobiliary Pancreat Sci 2013;20:24–34.
- Kiriyama S,Kozaka K, Takada T. Tokyo Guidelines 2018: diagnostic criteria and severity grading of acute cholangitis (with videos). J Hepatobiliary Pancreat Sci. 2018 Jan;25(1):17-30.
- Kinney TP. Management of ascending cholangitis. Gastrointest Endosc Clin N Am.2007 Apr;17(2):289-306, vi.
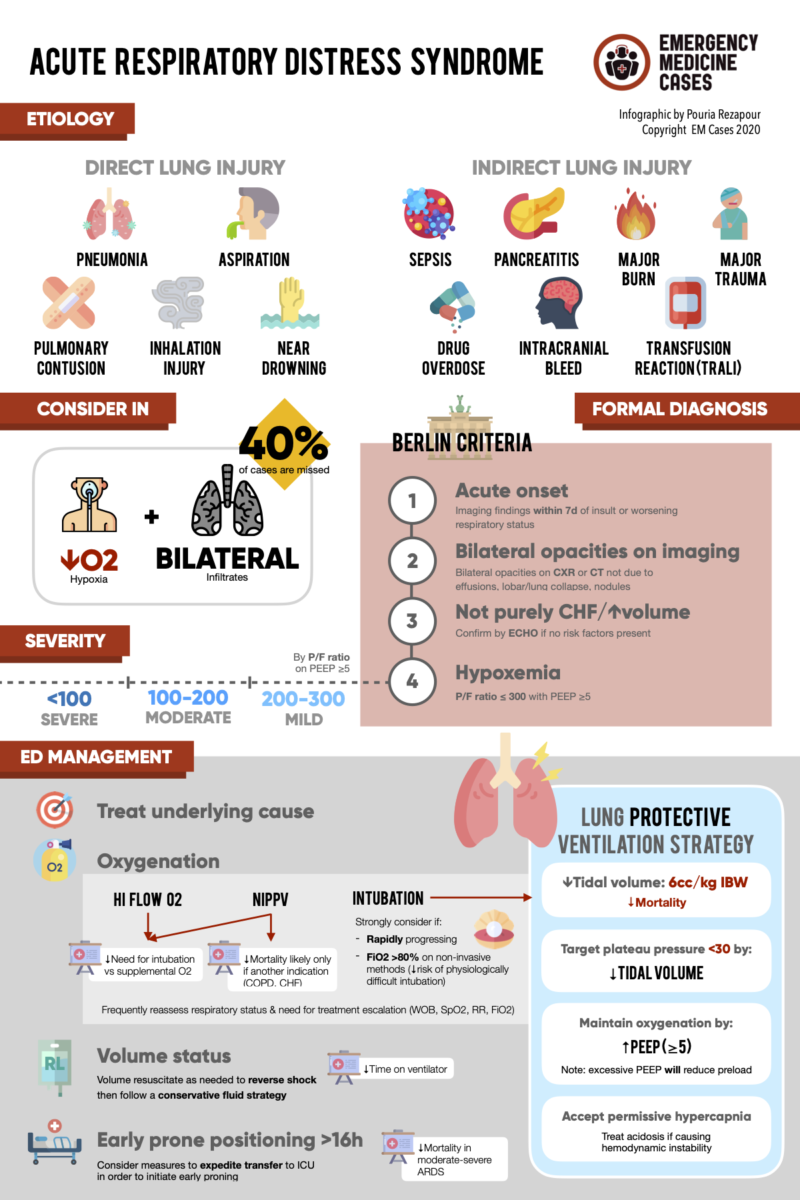
ED approach to ARDS Part 1
- ARDS is often overlooked in the ED, but if recognized early can significantly impact the patient’s hospital course
- Consider ARDS in all patients with respiratory failure and bilateral lung infiltrates
- While the cornerstone of treatment of ARDS is to treat the underlying cause, there are specific oxygenation strategies, fluid strategies, positioning options and paralytic options that are relevant to ED practice
- Based on a recent review of oxygenation strategies in respiratory failure, for non-invasive oxygenation our expert recommends face mask for patients with underlying COPD or CHF and High Flow Nasal Cannula (HFNC) for all other patients
- There are no hard indications for invasive ventilation as it is a clinical decision, however, it should be considered in patients requiring >80% inspired oxygen via a high flow delivery device
- ARDS ventilator settings
- Decrease Tidal Volume with a goal of 6mL/kg ideal body weight
- Optimize oxygenation with PEEP with the goals of improved oxygenation while minimizing potential decreases in BP and plateau pressure <30cm of water
- Optimize ventilation with the goal of avoiding clinically significant acidosis while using permissive hypercapnia
- PROSEVA trial showed that in intubated patients with moderate-severe ARDS early prone positioning for at least 16 hrs portended a survival benefit and case series suggest that early proning in the ED may help prevent the need for invasive ventilation
- The use of a paralytic agent in ventilated patients with ARDS has not shown to improve outcomes; but do consider paralytics for patients in whom you cannot achieve a Tidal Volume of 6mL/kg with appropriate analgesia and sedation, and as a rescue therapy after other therapies have failed
- Brower RG, Matthay MA, Morris A, et al. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000;342(18):1301-8.
- Ranieri VM, Rubenfeld GD, Thompson BT, et al. Acute respiratory distress syndrome: the Berlin Definition. JAMA. 2012;307(23):2526-33.
- Villar J, Ferrando C, Martínez D, et al. Dexamethasone treatment for the acute respiratory distress syndrome: a multicentre, randomised controlled trial. Lancet Respir Med. 2020;8(3):267-276.
- Vianello A, Arcaro G, Molena B, et al. High-flow nasal cannula oxygen therapy to treat patients with hypoxemic acute respiratory failure consequent to SARS-CoV-2 infection. Thorax. 2020.
- Ferreyro BL, Angriman F, Munshi L, et al. Association of Noninvasive Oxygenation Strategies With All-Cause Mortality in Adults With Acute Hypoxemic Respiratory Failure: A Systematic Review and Meta-analysis. JAMA. 2020;324(1):57-67.
- Brower RG, Lanken PN, Macintyre N, et al. Higher versus lower positive end-expiratory pressures in patients with the acute respiratory distress syndrome. N Engl J Med. 2004;351(4):327-36.
- Shelhamer M, Wesson PD, Solari IL, et al. Prone Positioning in Moderate to Severe Acute Respiratory Distress Syndrome due to COVID-19: A Cohort Study and Analysis of Physiology. Res Sq. 2020.
- Chandra S, Goel S, Dawra R. Early Neuromuscular Blockade in Children with Pediatric Acute Respiratory Distress Syndrome. J Pediatr Intensive Care. 2020;9(3):201-206.
None of the authors have any conflicts of interest to declare





Leave A Comment