Managing acutely agitated patients can cause anxiety in even the most seasoned emergency doctor. These are high risk patients and they are high risk to you and your ED staff. It’s important to understand that agitation or agitated delirium is a cardinal presentation – not a diagnosis. There is pathology lurking beneath – psychiatric, medical, traumatic and toxicological diagnoses driving these patients and we just won’t know which until we can safely calm them down. An added difficulty is that most of the literature on emergency management of the agitated patient originates from psychiatric papers studying populations that do not necessarily generalize to the ED. In this podcast, Dr. Reuben Strayer and Dr. Margaret Thompson (with a special bonus appearance by guest researcher David Barbic) offer some guiding principles on the safe and effective management of the agitated patient…
Podcast production, sound design & editing by Anton Helman, voice editing by Sucheta Sinha
Written Summary and blog post by Alex Hart and Shaun Mehta, edited by Anton Helman September, 2018
Cite this podcast as: Helman, A, Strayer, R, Thompson, M. Emergency Management of the Agitated Patient. Emergency Medicine Cases. September, 2018. https://emergencymedicinecases.com/emergency-management-agitated-patient/. Accessed [date]
Step 1: Categorize the agitation as mild, moderate or severe
Sometimes it is obvious that a patient is extremely agitated and needs to be taken down imminently in order to protect the department staff and the patient themselves. It is helpful though in cases that are less clinically obvious to have an approach to classifying a given patient’s level of agitation in order to better target sedation therapy.
Our experts recommend dividing agitated patients into the following 3 categories:
Mild: Agitated but cooperative
Moderate: Disruptive without danger
Severe: Excited delirium and/or dangerous to self and/or staff
Many scales exist, including the Sedation Assessment Tool, the Agitated Behavior Scale, the Overt Aggression Scale and the Positive and Negative Syndromes Scale. While these may be useful for research purposes, they are not practical for clinical practice. The Behaviour Activity Rating Scale (BARS) is probably the simplest scale and has good inter-rater reliability.
Excited Delirium Syndrome
Excited delirium is a life threatening medical emergency. It has several distinctive features (despite it usually being a retrospective diagnosis):
- High degree of agitation
- Diaphoretic, tachypneic and hyperthermic
- Unusual “super-human” strength
- Impervious to pain and fatigue
- Unable to maintain attention
- Incoherent
- Severe metabolic acidosis
A typical clinical scenario is an obese male in mid-30’s displaying destructive/bizarre behavior leading to call to police in setting of psycho-stimulant drug or alcohol intoxication, with prior psychiatric illness. A subset of patients eventually enter a quiescent period (for less than a minute) where they suddenly stop struggling followed by a respiratory or cardiac arrest.
It is often better to err on the side of caution and assume a state of excited delirum rather than dismissing a patients behaviour as the product of a more benign cause (e.g. alcohol intoxication).
Learn more about Excited Delirium in Episode 2: Excited Delirium
Step 2a: Non-pharmacologic de-escalatation for the mild or moderately agitated patient
Verbal de-escalation is often effective, but requires a calm and deliberate approach.
Approximately 90% of all emotional information and more than 50% of the total information in spoken English is communicated not by what one says but by body language, especially tone of voice.
- One person delegated
- Ensure a quiet environment
- Don’t spend too much time
- Monitor your own emotional and physiologic response so as to remain calm
- Maintain at least 2 arm’s lengths of distance between you and the patient with an exit door close by and in the opposite direction of the patient
- Hands should be visible and not clenched
It’s hard enough to interact with our fellow human in normal day to day interaction without provoking some form of social anxiety. So what do we do when those we are trying to speak to are threatening physical violence? Not sure where to start? Try the SAVE mnemonic:
Support – “Let’s work together…”
Acknowledge – “I see this has been hard for you.”
Validate – “I’d probably be reacting the same way if I was in your shoes.”
Emotion naming – “You seem upset.”
Step 2b: The Code White for the moderate or severely agitated patient
So you didn’t hit it off with the patient high on PCP. Don’t be hard on yourself. But also, don’t be a cowboy. Call for help. There are times when it is necessary to call that code white.
Indications for calling a code white
- Severe agitation
- Immediate physical threat to you and/or your staff
- Requiring multiple people to restrain
Pitfall: A common pitfall is to call a code white as a threat to an uncooperative patient. Calling a code white in and of itself can ramp up an already tense situation. For the moderately agitated patient who is not in imminent danger to themselves or to your staff, consider calling a concealed code white direct to security rather than using an overhead page. Never use code white it as a threat.
EDs should ideally have a protocol for code white. Establishing roles for EMS, police, security, nursing, crisis workers, technicians and social workers in advance, preferably in simulation training, can help make code white safe and effective. Consider pre-mixed medications for sedation. Consider a plan for cardiorespiratory monitoring +/- airway management.
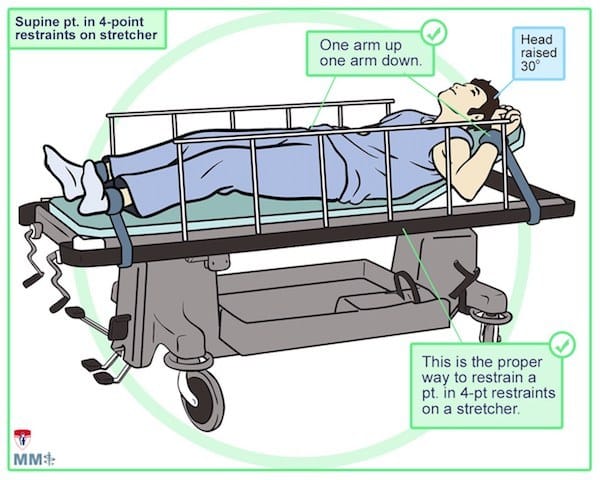
Step 3: Safe and effective physical restraints in the emergency management of agitated patients
There is ongoing debate as to whether or not physical restraints should be used at all in the management of the agitated patient in the ED. If you are going to use physical restraints the goal should be to use them as a last resort, only as a bridge to adequate chemical sedation, which should take no longer than 5-15 minutes with appropriate dosages of calming medications. Prolonged use of physical restraints may result in active resistance of restraint by the patient which may lead to electrolyte abnormalities, arrhythmias, and put the patient at further risk for rhabdomyolysis.
One option is not to use physical restraints, and rather have the patient held down by security for the few minutes it takes for the claiming medications to take effect. The other option is to first place the physical restraints on the patient, immediately followed by IM calming medications and releasing the restraints as soon as the patient is calm. Physical restraint should always be followed by immediate chemical sedation.
When used properly, physical restraints can be quite safe as was demonstrated in this 2003 study by Zun. However, improper use can be lethal as shown in this 2012 study of 26 deaths presumed to be the direct result of improper physical restraints.
Restraints are not benign. Don’t restrain and walk away. Ensure the following:
Ideally, 6 trained staff with personal protective equipment (gloves, gowns, face-mask) are needed to apply physical restraints effectively: 1 for each extremity, 1 for the head and 1 to give medications and help apply restraints
Pearl: Avoid covering the agitated patient’s mouth and/or nose with a gloved hand. This can lead to asphyxia, metabolic acidosis and death. To prevent the patient spitting on staff, instead, use an oxygen mask. This may also serve to improve any oxygenation issues the patient may have.
Listen to Dr. Strayer’s Best Case Ever for more on this pearl.
Do’s and Don’t of Physical Restraints
Do
- Use 4 or 5 point restraints
- Use medical grade restraints
- Supine position whenever possible
- Restrain one arm above the head and the other below the waist
- Elevate the head of the bed about 30 degrees
- Tie restraints to the bed-frame (not the rails)
Don’t
- Restrain in prone position (increases risk of airway complications)
- Restrain to the bed rails (increases risk of injury)
- Use two point restraints (increases risk of injury)
- Tie knots that are difficult to undo
- Put a pillow under the patient’s head (suffocation risk)
Particular care should be given to ensuring a clear airway is maintained, as the airway can be put at risk if the patient is turned prone with pressure on the neck or shoulder to try to guard against spitting or biting.
Your responsibility does not end with the patient. Keep your team safe.
Tips to make sure the department is kept safe in a dangerous situation:
- Never turn your back on the individual
- Don’t walk ahead of the individual and ensure adequate personal space
- Provide continuous observation and record behaviour changes in patient notes
- Wear personal duress alarm if available
- Never block off exits and ensure you have a safe escape route
Step 4: Calming medications in the emergency management of the agitated patient
The goal of calming medications is to enable rapid stabilization of the critically ill patient and to enable the expeditious search for potential life threatening diagnoses.
What is the best route of administration for calming medications?
Most departments have oral (po/sl), intramuscular (IM), intravenous (IV), and intranasal (IN) options for medication administration. The choice of route depends on how agitated your patient is. For cooperative patients, offer a po/sl medication first. For uncooperative moderate and severely agitated patients, the safest option is to start with IM.
Pitfall: A common pitfall is to attempt an IV start on a severely agitated patient. Protect your nursing staff. Do not attempt IVs in agitated, thrashing patients. It is much safer to calm them with an IM medication first, and then attempt to start an IV once the patient is calm.
Calming medication options include ketamine, benzodiazepines and antipsychotics
Several regimens exist. Our experts suggest the following based on optimal route, pharmacologic mechanism of action, and patient/staff safety.
Whenever possible, tailor the therapy to the underlying diagnosis (psychotic psychiatric disorder vs alcohol withdrawal vs drug intoxication etc).
|
Level of Agitation |
1st Choice Drug, Dose, Route |
Alternative or Adjunct Drug |
|
Mild |
Lorazepam 1-2 mg SL |
po antipsychotic that has previously been effective for that particular patient |
|
Moderate |
Midazolam 2-5 mg IM |
Haloperidol 5-10 mg IM |
|
Severe |
Ketamine 5 mg/kg IM |
Haloperidol 10mg IM AND Midazolam 10mg IM |
Benzodiazepines are safe and effective calming medications in the young adult
Midazolam is the best IM option. Maximum effect is in 10 minutes, and lasts up to 2 hours. In alcohol intoxicated patients, beware of respiratory depression with benzodiazepines. All alcohol intoxicated patients who are receiving benzodiazepines for agitated should be placed on a cardiac monitor, ideally with end-tidal CO2 monitoring for earliest detection of respiratory depression.
Pearl: Place alcohol intoxicated patients who are receiving benzodiazepines for moderate agitated on end tidal CO2 monitoring for early detection of respiratory depression.
Diazepam is poorly absorbed by the IM route and lorazepam is erratically and slowly absorbed; additionally, lorazepam requires refrigeration, which can impose acquisition delays. When a benzodiazepine is required urgently–for any indication–our experts recommend midazolam, which is quickly and reliably absorbed IM. The “M” in IM stands for Midazolam.
Update 2020: A prospective randomized double blind trial involving 115 acutely agitated patients demonstrated that dropiderol is superior to lorazepam or ziprasidone (10 or 20mg) in the treatment of acute agitation and resulted in fewer episodes of respiratory depression. Abstract
Update 2021: Randomized, single institution study of 93 patients compared ketamine (4 mg/kg IM or 1mg/kg IV) and haloperidol/lorazepam (haloperidol 5-10 mg IM/IV + lorazepam 1-2 mg IV/IM) with regards to “time to sedation”, and found ketamine was significantly more effective at both 5 minutes and 15 minutes after medication administration (no statistically significant increase in adverse effects). Abstract
Update 2021: Single-centered, randomized trial of 80 patients comparing ketamine (5 mg/kg IM) and haloperidol/midazolam (5 mg for both), showing a significantly different mean “time to sedation” of 6 minutes for the ketamine group and 15 minutes for the haloperidol/midazolam group (no statistical difference in serious adverse events). Abstract
Haloperidol should be considered an adjunct to benzodiazepines in moderate and severe agitation and may be appropriate as monotherapy in moderately agitated intoxicated patients that cannot be placed on a monitor when resources are limited.
Be aware that haloperidol has a longer half life than midazolam, and can cause your patient to linger in the ED for many hours more than necessary. The mean time to sedation is 25-28 minutes and is therefore not recommended as monotherapy when immediate sedation is required for the severely agitated patient.
What about the safety of haldol?
While traditional teaching has been to avoid Haloperidol in some at risk patients because of fears of prolongation of the QT interval
resulting in Torsades de Pointes and concerns over lowering the seizure threshold, there is no good evidence in the literature that in real practice this risk exists according to our experts. Although we know that haloperidol prolongs the QTc, this effect is very unlikely to be clinically consequential at the doses typically used for emergency agitation. However caution is advised in patients who are already on multiple QTc-prolonging agents. Consider obtaining a baseline ECG first in these higher risk patients, when possible. It is also very unlikely that patients will suffer extrapyramidal symptoms from one dose of haloperidol in the ED, so this potential side effect should not dissuade the use of haloperidol in the severely agitated patient.
Ketamine 5mg/kg IM may be the first line medication for excited delirium and the severely agitated patient
Ketamine is an NMDA-receptor antagonist, providing rapid sedation and analgesia. Of the available options, time to sedation is the fastest, usually less than 5 minutes with appropriate dosing, and it has a predictable dose-response relationship. While the weak sympathomimetic properties of ketamine may increase heart rate and BP in the calm patient, these effects of ketamine are not of concern in the severely agitated patient who is in sympathomimetic overdrive already. Rather, ketamine will have a predictably calming effect and may lower the heart rate and blood pressure. Current evidence for the effectiveness and safety of ketamine in calming the severely agitated patient is promising, yet not definitive. A large single center RCT is currently underway in Vancouver comparing Ketamine 5mg/kg IM vs Midazolam + Haldol IM. Two IM injections of ketamine may be required depending on the weight of your patient and whether or not your ED carries the highly concentrated formulation or not.
Future options for calming medications in the agitated patient may include nebulized loxapine and dexmedetomidine IM, but strong evidence is pending.
Pharmacologic options in the older agitated patient
Elderly patients are at increased risk of respiratory depression and delirium from benzodiazepines. Our experts recommend avoiding benzodiazepines whenever possible, the exception being alcohol/sedative-hypnotic withdrawal. Haldol 0.5mg IM is a reasonable first line medication for the agitated older patient. Consider atypical antipsychotics such as risperidone, quetiapine or olanzapine starting at the lowest dose and titrating slowing to effect.
|
Avoid benzodiazepines |
|
Use antipsychotics (consider atypicals) |
|
Start low, go slow |
Step 5: Treat immediate life threats and persue underlying diagnosis in the emergency management of the agitated patient as soon as calming medications take effect
Agitation, agitated delirium and excited delirium are not diagnoses, but rather cardinal presentations of a variety of life-threatening underlying diagnoses.
Mild to moderately agitated patients
Collect as much corroborating history as possible from police, family and any social supports. A head-to-toe physical exam with the patient completely disrobed is essential so as not to miss obvious pathology that is concealed by clothing. Cast a wide differential diagnosis including space occupying CNS lesions, toxiciologic, psychiatric, traumatic and metabolic causes with appropriate laboratory and imaging testing as required.
Severely agitated patients
In the severely agitated patient the history and physical exam are more limited, so it is important to be organized in your approach.
A) First few minutes
1. Place the patient in a resuscitation room and apply cardiorespiratory monitoring, capnography and oximetry
2. Place 1-2 large bore IV lines
3. Assess for and start to treat:
Hypoxia – place supplemental O2
Hyperthermia – obtain rectal temperature and initiate cooling measures
Hypoglycemia – obtain capillary glucose and administer D50W
Hypovolemia – most severely agitated patients will be volume depleted and acidotic; initiate crystalloid 1L bolus on speculation
B) Next few minutes
Hyperkalemia and acidemia – send a blood gas with lytes and consider calcium gluconate, insulin with glucose and sodium bicarb
CNS lesions – CT head
Monitoring – ideally vitals q5min for the first 30 mins
C) Next hour
Consider primary diagnoses such as: sepsis, neuroleptic malignant syndrome, thyrotoxicosis, meningitis/encephalitis
Rule out consequences of agitation: rhabdomyolysis, traumatic injuries
Airway considerations in the emergency management of the severely agitated patient
The primary airway issues in the severely agitated patient are often inadequate preparation and preoxygenation secondary to patient combativeness. For this reason, our experts recommend avoiding rapid-sequence intubation (RSI) and instead perform a delayed-sequence intubation (DSI). Initiate a dissociative dose of ketamine, adequately preoxygenate your patient, and then, if necessary, administer the paralytic and perform endotracheal intubation. Moderate hyperventilation prior to intubation to at least the patient’s resting elevated respiratory rate may improve acidemia and avoid a precipitous rapid drop in blood pressure after intubation. Maintain high ventilatory rates after intubation.
If a paralytic is used, our experts suggest avoiding succinylcholine because of potential side effects such as hyperkalemia, hyperthermia and acidemia.
Take Home Points on The Emergency Management of Agitated Delirium
- There are 5 steps to the emergency management of the agitated patient:
- Categorize the agitation as mild, moderate or severe,
- Employ de-escalation techniques in the mild-moderate agitated patient and/or call a code white in the moderate-severe agitated patient,
- Physically restrain the moderate-severe agitated patient safely with either limbs held down by security personnel or by physical restraints
- Administer calming medications as soon as possible
- Treat immediate life threats and pursue the underlying diagnosis
- Agitation or agitated delirium is a cardinal presentation, not a diagnosis. There is pathology lurking beneath. Cast a wide differential diagnosis.
- If physical restraints are used, they should be used as a last resort for the the shortest possible time, only until calming medications have taken effect and according to safe procedural protocol.
- Severely agitated patients require immediate attention to potential life threats and a thorough assessment and work-up including a head to toe physical exam and consideration for disease specific laboratory and imaging testing. A step-wise approach should start with identification and treatment of hypoxemia, hyperthermia, hypoglycemia and hypovolemia.
- Most agitated patients in the ED are moderately agitated and first line medications include midazolam 2-5mg IM and haloperidol 5-10mg IM. Medications should be tailored to the suspected underlying cause.
- Benzodiazepines should be avoided in older patients whenever possible. Instead consider antipsychotic medications, start low and go slow.
- For the rarer very severe agitated Ketamine 5mg/kg is considered first line for calming of the severely agitated patient by our experts, however evidence is not definitive.
- Delayed sequence intubation with specific peri-intubation management of severe acidosis is recommended in the airway management of severely agitated patients.
For more on managing difficult patients on EM Cases:
Episode 51 Effective Patient Communication – Managing Difficult Patients
References
- Nazarian DJ, Broder JS, Thiessen MEW, et al. Clinical Policy: Critical Issues in the Diagnosis and Management of the Adult Psychiatric Patient in the Emergency Department. Ann Emerg Med. 2017;69(4):480-498.
- Coburn, V. & Mycyk, M. (2009). Physical and Chemical Restraints. Emergency Medicine Clinics of North America. 27, 655-667.
- Rossi, J. Swan, M. & Isaacs, E. (2010). The Violent or Agitation Patient. Emergency Medicine Clinics North America. 28, 235-256.
- New A, Tucci VT, Rios J. A Modern-Day Fight Club? The Stabilization and Management of Acutely Agitated Patients in the Emergency Department. Psychiatr Clin North Am. 2017 Sep;40(3):397-410.
- Nice.org.uk. (2018). Violence and aggression: short-term management in mental health, health and community settings | Guidance and guidelines | NICE. [online] Available at: https://www.nice.org.uk/guidance/ng10.
- Wilson MP, Pepper D, Currier GW, Holloman GH Jr, Feifel D. The psychopharmacology of agitation: consensus statement of the American Association for emergency psychiatry project Beta psychopharmacology workgroup. West J Emerg Med. 2012 Feb;13(1):26-34.
- Swift, RH, Harrigan, EP, Cappelleri, JC, et al, Validation of the behavioural activity rating scale (BARS): a novel measure of activity in agitated patients. Journal of Psychiatric Research, 2002. 36: p. 87‐95.
- Zeller SL, Citrome L. Managing Agitation Associated with Schizophrenia and Bipolar Disorder in the Emergency Setting. West J Emerg Med. 2016;17(2):165-72.
- Richmond JS, Berlin JS, Fishkind AB, et al. Verbal De-escalation of the Agitated Patient: Consensus Statement of the American Association for Emergency Psychiatry Project BETA De-escalation Workgroup. West J Emerg Med. 2012 Feb;13(1):17-25.
- Glezer A, Brendel RW. Beyond emergencies: the use of physical restraints in medical and psychiatric settings. Harv Rev Psychiatry. 2010 Nov-Dec;18(6):353-8.
- Downey LV, Zun LS, Gonzales SJ, Frequency of alternative to restraints and seclusion and uses of agitation reduction techniques in the emergency department. Gen Hosp Psychiatry, 2007. 29(6): p. 470‐4.
- Martin B, Restraint use in acute and critical care settings: changing practice. AACN Clin Issues, 2002. 13(2): p. 294‐306.
- Centers for Medicare and Medicaid Services. State Operations Manual. Department of Health and Human Services; 2008. Available at: https://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R37SOMA.pdf.
- Zun LS. A prospective study of the complication rate of use of patient restraint in the emergency department. J Emerg Med. 2003 Feb. 24(2):119-24.
- Coburn VA, Mycyk MB. Physical and chemical restraints. Emerg Med Clin North Am. 2009 Nov. 27(4):655-67, ix.
- Zun LS. A prospective study of the complication rate of use of patient restraint in the emergency department. J Emerg Med. 2003 Feb. 24(2):119-24.
- Annas GJ. The last resort–the use of physical restraints in medical emergencies. N Engl J Med. 1999 Oct 28. 341(18):1408-12.
- Currier GW, Simpson GM, Risperidone liquid concentrate and oral lorazepam versus intramuscular haloperidol and intramuscular lorazepam for treatment of psychotic agitation. J Clin Psychiatry, 2001. 62(3): p. 153‐7.
- Currier GW, Chou JC, Feifel D, Acute treatment of psychotic agitation: a randomized comparison of oral treatment with risperidone and lorazepam versus intramuscular treatment with haloperidol and lorazepam. J Clin Psychiatry, 2004. 65(3): p. 386‐94.
- Nobay F, Simon BC, Levitt MA, Dresden GM. A prospective, double-blind, randomized trial of midazolam versus haloperidol versus lorazepam in the chemical restraint of violent and severely agitated patients. Acad Emerg Med. 2004;11(7):744-9.
- Richards JR, Derlet RW, Duncan DR, Chemical restraint for the agitated patient in the emergency department: lorazepam versus droperidol. J Emerg Med, 1998. 16(4): p. 567‐73.
- Martel M, Sterzinger A, Miner J, et al, Management of acute undifferentiated agitation in the emergency department: a randomized double‐blind trial of droperidol, ziprasidone, and midazolam. Acad Emerg Med, 2005. 12(12): p. 1167‐72.
- Isenberg DL, Jacobs D. Prehospital Agitation and Sedation Trial (PhAST): A Randomized Control Trial of Intramuscular Haloperidol versus Intramuscular Midazolam for the Sedation of the Agitated or Violent Patient in the Prehospital Environment. Prehosp Disaster Med. 2015 Oct;30(5):491-5.
- Kroczak S et al. Chemical Agents for the Sedation of Agitated Patient in the ED: A Systematic Review. Am J Emerg Med. 2016. (34); 2426-2431.
- Gottlieb M, Long B, Koyfman A. Approach to the Agitated Emergency Department Patient. J Emerg Med. 2018;54(4):447-457.
- Zun LS. Evidence-Based Review of Pharmacotherapy for Acute Agitation. Part 1: Onset of Efficacy. J Emerg Med. 2018;54(3):364-374.
- Gottlieb M, Schiebout J. What Is the Efficacy of Droperidol for the Management of Acute Psychosis-Induced Agitation?. Ann Emerg Med. 2018;71(1):141-143.
- Battaglia J, Moss S, Rush J, et al. Haloperidol, lorazepam, or both for psychotic agitation? A multicenter, prospective, double-blind, emergency department study. Am J Emerg Med. 1997 Jul;15(4):335-40.
- Bieniek SA, Ownby RL, Penalver A, Dominguez RA. A double-blind study of lorazepam versus the combination of haloperidol and lorazepam in managing agitation. 1998 Jan-Feb;18(1):57-62.
- Hui D, Frisbee-Hume S, Wilson A, et al. Effect of Lorazepam With Haloperidol vs Haloperidol Alone on Agitated Delirium in Patients With Advanced Cancer Receiving Palliative Care: A Randomized Clinical Trial. 2017 Sep 19;318(11):1047-1056.
- Le Cong M, Humble I. A Ketamine Protocol and Intubation Rates for Psychiatric Air Medical Retrieval. Air Med J. 2015 Nov-Dec;34(6):357-9.
- Cole JB, Moore JC, Nystrom PC, et al. A prospective study of ketamine versus haloperidol for severe prehospital agitation. Clin Toxicol (Phila). 2016 Aug;54(7):556-62.
- Riddell J, Tran A, Bengiamin R, Hendey GW, Armenian P. Ketamine as a first-line treatment for severely agitated emergency department patients. Am J Emerg Med. 2017 Jul;35(7):1000-1004.
- Isbister GK, Calver LA, Downes MA, Page CB. Ketamine as Rescue Treatment for Difficult-to-Sedate Severe Acute Behavioral Disturbance in the Emergency Department. Ann Emerg Med. 2016;67(5):581-587.e1.
- Vrana B. Use of Intranasal Ketamine for the Severely Agitated or Violent ED Patient. J Emerg Nurs. 2016;42(3):198-9.
- Lahti AC, Koffel B, LaPorte D, Tamminga CA. Subanesthetic doses of ketamine stimulate psychosis in schizophrenia. 1995 Aug;13(1):9-19.
- Peisah C, Chan DK, McKay R, Kurrle SE, Reutens SG. Practical guidelines for the acute emergency sedation of the severely agitated older patient. Intern Med J. 2011 Sep;41(9):651-7.
- Aftab A, Shah AA. Behavioral Emergencies: Special Considerations in the Geriatric Psychiatric Patient. Psychiatr Clin North Am. 2017 Sep;40(3):449-462.
- Kruse WH. Problems and pitfalls in the use of benzodiazepines in the elderly. Drug Saf. 1990 Sep-Oct;5(5):328-44.
- Bogunovic OJ, Greenfield SF. Practical geriatrics: Use of benzodiazepines among elderly patients. Psychiatr Serv. 2004 Mar;55(3):233-5.
FOAMed Resources on The Agitated Patient
- http://emupdates.com/2016/09/03/emergency-management-of-the-agitated-patient/
- http://emupdates.com/2017/11/02/jon-cole-on-ketamine-for-agitation/
- https://lifeinthefastlane.com/behavioural-emergencies/
- http://www.emdocs.net/emdocs-cases-ed-approach-agitation/
- http://www.emdocs.net/the-art-of-the-ed-takedown/
- http://www.emdocs.net/ketamine-agitated-violent-patient/
- https://canadiem.org/the-agitated-patient-in-the-ed-part-2/
- https://emcrit.org/emcrit/human-bondage-chemical-takedown/
- http://rebelem.com/chemical-sedation-of-the-agitated-patient/
- http://stemlynsblog.org/acute-behavioural-disturbance/
Drs. Helman, Strayer and Thompson have no conflicts of interest to declare
Now test your knowledge with a quiz.




If dexmetomidine were to be used some day in which patients would you speculate it would be best used?
Dose?
droperidol has the best evidence, but unfortunately is not widely available. as far as i know dexmedetomidine evidence is sparse with case reports only https://www.ncbi.nlm.nih.gov/pubmed/27842924 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3017407/ https://www.ajemjournal.com/article/S0735-6757(16)30813-0/pdf https://www.annemergmed.com/article/S0196-0644(16)30463-2/abstract and the dose varies. i wouldn’t recommend it at present.
We owe you a great debt dr.Anton , we are always learning a good stuff and informative website ..
0.5mg im of Haloperidol in elderly? Can you, please, say more about haldol use in elderly patients, initial dose and escalation procedure?
There are a few studies showing that olanzapine might be superior to haloperidol with regards to producing the desired level of calmness. Any thoughts on when olanzapine might be considered over haloperidol?
They are very similar. Olanzapine is probably a little faster acting than haldol and does not have the QT concerns. The downsides are a) it’s more expensive b) it’s not stocked in many departments. but these are small downsides; it would be reasonable to replace haldol with olanzapine for agitation.