There are hundreds of clinical decision rules and risk scales published in the medical literature, some more widely adopted than others. Dr. Ian Stiell, the father of clinical decision rules, shares with us his views and experiences gained from co-creating some of the most influential CDRs and risk scales to date. In discussion with Dr. Hans Rosenberg, he explains the criteria for developing a CDR, the steps to developing a valid CDR, how best to apply CDRs and risk scales to clinical practice, and the hot-off the-press new Ottawa COPD Risk Score and Ottawa Heart Failure Risk Score for helping you with disposition decisions. It turns out that in Canada, we discharge about two thirds of the acute decompensated heart failure patients that we see in the ED, while the US almost all patients with decompensated heart failure are admitted to hospital. Dr. Stiell’s new risk scores may help physicians in Canada make safer disposition decisions while help physicians in the US avoid unnecessary admissions.
COUNTERPOINT: Dr. Anand Swaminathan’s rant on the use and barriers to use of Dr. Stiell’s clinical decision rules and risk scales in the United States…
Link to The Stiell Sessions Part 2: Update in Atrial Fibrillation – The New Guidelines
Written Summary & Blogpost Prepared by Dr. Michael Kilian, edited by Dr. Anton Helman, December 2014
Cite this podcast as: Helman, A, Stiell, I, Rosenberg, H. The Stiell Sessions: Clinical Decision Rules and Risk Scales. Emergency Medicine Cases. December, 2014. https://emergencymedicinecases.com/episode-56-stiell-sessions-clinical-decision-rules-risk-scales/. Accessed [date].
Criteria For Developing a Clinical Decision Rule
In order to develop a useful clinical decision rule (CDR), a number of criteria must be met. Firstly, the condition needs to be relatively common. Rare conditions will not have the necessary volume of data to generate high quality decision rules. In addition to being a common complaint or illness, there must also be a perceived inefficiency or clinical variability in practice with regards to the workup of the patient. For example, the inefficiency can be an over-use or under-use of a particular resource (imaging, blood tests etc.) which, given a lack of evidence, physicians have different approaches to. Lastly, the clinical question that leads to the inefficiency needs to be answerable with only a handful of clinical variables.
Clinical Decision Rules vs Risk Stratification Scales
More complex conditions such as CHF and COPD have a spectrum of severity and acuity. Their management cannot be reduced to a binary question, since multiple factors need to be taken into consideration. This is in contradistinction to the Ottawa Ankle rule, in which a binary question is asked – does this patient require an x-ray or not? As a result, these complex conditions require risk stratification scales (rather than CDRs), which estimate the risk of a bad outcome. These scales can help physicians decide what the appropriate management and disposition for the patient would be.
The Development of a Clinical Decision Rule
Before CDRs can be safely applied in clinical practice they undergo a rigorous development process. The four phases of development include derivation, validation, implementation and studying the barriers to adoption. Although the rule is derived and published in the literature, it should not be used clinically until it has been prospectively validated and shown to be effective.
Applying Clinical Decision Rules & Risk Scales to Practice
Despite the rigorous development process that is involved in refining the CDRs, there are some clinicians who are hesitant to apply them in a clinical setting. Some clinicians feel that the rules may be too complex or that they take too long to apply. However, compared to the time it takes to organize and follow up on imaging results, the use of CDRs can be more time efficient for both the physician and the patient, and can improve the flow within a department. Different institutions also have different cultures or habits around investigating and treating a particular condition. This variation is also seen between different health care systems, especially when there are regional differences in the medico-legal environment or funding model. There are some clinicians who believe that their clinical experience is more accurate than clinical decision rules and might place more value on gestalt. Gestalt and experience are valuable and should be used to think critically about our patients. However, what makes emergency medicine challenging is that we rarely get feedback on the patient’s clinical course after they have visited the ED. Therefore, no matter how much clinical experience one has, the diagnostic loop is rarely closed as the patient will either follow up with their primary care provider or seen another emergency physician if the problem does not resolve.
When considering whether to apply a clinical decision rule, it is important to consider several factors. Most importantly, you must evaluate whether the rule you want to use applies to your patient. To answer this question it’s important to know the inclusion and exclusion criteria that were used to develop this rule (inclusion and exclusion criteria are provided below along with their respective CDRs). Secondly, you must consider what information the rule will give you. There are both one-way rules and two-way rules. The PERC rule is an example of a one-way rule. It is designed to rule out a pulmonary embolism in your patient. If the PERC rule is positive it simply means you cannot confidently rule out a PE, but a positive result should not guide your clinical decision-making. The Ottawa Ankle Rule is an example of a two-way rule. Applying it will either direct you to order an x-ray or not order an x-ray.
Below you will find common CDRs and risk stratification tools developed by the research group in Ottawa. We encourage you to become familiar with the inclusion and exclusion criteria. Next time you see a patient, ask yourself whether the rule you are about to apply has been studied in the same population.
All of the following Risk Scales and Clinical Decision Rules with their inclusion and exclusion criteria will be available on the Agile MD app along with all the other EM Cases summaries for easy quick reference at the bedside.
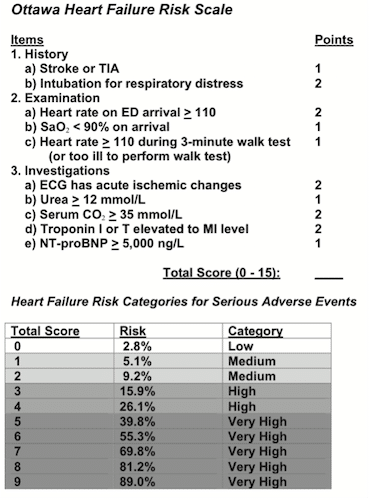
The Ottawa Heart Failure Risk Scale – Validated & Updated November 2014 & March 2017
Application: This is a risk stratification tool which provides physicians with a risk estimate of short-term serious adverse events for patients presenting to the ED with acute shortness of breath secondary to heart failure. It can help the physician make an evidence-based decision regarding admission or discharge of the patient.
The score above was developed in the derivation phase. During the validation phase the score was reduced to 5 variables. Although the risk stratification for the variables is not yet published our experts have shared the variables with you here.
Validated CHF variables (unpublished as of December 2014):
- IV Nitrate use
- Troponin elevated at 5x upper reference
- Elevated PCO2
- Elevated Urea or Cr
- Failing a walk test
- O2110 at rest
- Too sick to walk
- Unable to walk for 3min after standing
Inclusion Criteria:
- Age ≥ 50
- Presenting with acute SOB secondary to an exacerbation of chronic heart failure or new-onset heart failure
- The diagnosis of heart failure was defined as:
- Appropriate symptoms (shortness of breath or fatigue)
- Clinical signs of fluid retention (pulmonary or peripheral
- Presence of an underlying abnormality of cardiac structure or function
- If there was doubt about etiology, a beneficial response to treatment (ie, diuresis) was included.
Exclusion Criteria: (Patients too unwell to be discharged)
- Resting O2 sat <85% on room air or after being on the usual home O2 setting for 20min.
- HR ≥ 120bpm/min on arrival
- SBP <90
- Confusion, disorientation or dementia
- Ischemic chest pain requiring nitrates on arrival
- Acute ST-segment elevation on ECG on arrival
- Death from chronic illness expected within weeks
- Arrival from nursing home or chronic care facility
Stiell, Ian G et al. “A risk scoring system to identify emergency department patients with heart failure at high risk for serious adverse events.” Academic Emergency Medicine 20.1 (2013): 17-26. Full pdf
Update 2017 Validation of CHF rule Abstract
Interpretation of the 2017 study with Justin Morgenstern on First10EM
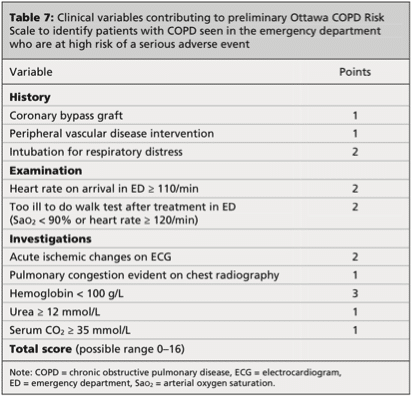
The Ottawa COPD Risk Scale
Clinical variables in the Ottawa COPD Risk Scale
Risk categories for patient in acute COPD exacerbation
Application: This is a risk stratification tool which provides physicians with a risk estimate of short-term serious adverse events for patients presenting to the ED with a COPD exacerbation. It can help the physician make an evidence-based decision regarding admission or discharge of the patient.
Inclusion Criteria:
- Age≥ 50 years
- Presenting with COPD exacerbation, defined as:
- Increase in at least 2 of 3 specified symptoms (breathlessness, sputum volume, sputum purulence)
- COPD has been previously diagnosed or diagnosed in the ED on the basis of a 1 year history of chronic dyspnea or cough with sputum production.
- ≥ 15 pack year smoking history
- Prior or current evidence of airflow obstruction
Exclusion Criteria: (Patients too unwell to be discharged)
- Resting O2 Sat <85%
- Heart Rate ≥ 130bpm/min
- SBP
- Confusion, disorientation or severe dementia
- Ischemic chest pain requiring treatment on arrival
- Acute ST elevation on ECG on arrival
- Arrival from nursing home or chronic care facility
- Death from chronic illness expected within weeks
Stiell, Ian G et al. “Clinical characteristics associated with adverse events in patients with exacerbation of chronic obstructive pulmonary disease: a prospective cohort study.” Canadian Medical Association Journal (2014): cmaj. 130968. Full pdf
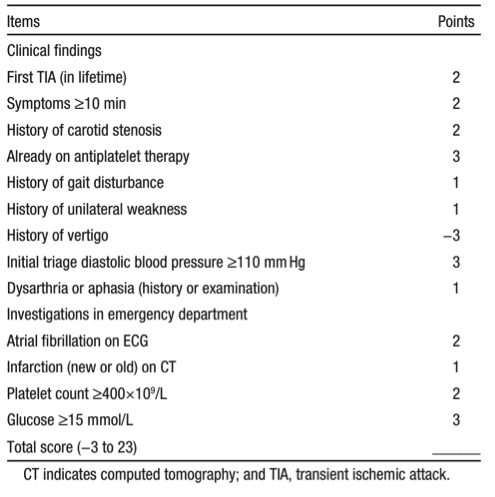
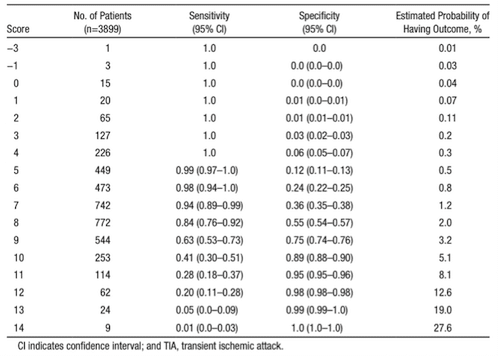
The Ottawa TIA Risk Score
Clinical Variables
Probability of TIA based on score
Application: This is a risk stratification tool, which provides physicians with an estimate of the risk that a patient presenting to the ED with TIA will suffer a stroke within 7 days.
Inclusion Criteria:
- Age > 18
- Diagnosed with a TIA in the ED by either the ED physician or neurologist
Exclusion Criteria:
- Patients who were diagnosed with a confirmed stroke (neurological deficit present >24 hours)
- Decreased LOC (GCS <15)
- Documented other cause for deficit which was not a TIA
- Presented >7 days following onset of most recent TIA and treated with TPA for an acute stroke.
Perry, Jeffrey J et al. “A Prospective Cohort Study of Patients with Transient Ischemic Attack to Identify High-Risk Clinical Characteristics.” Stroke; a journal of cerebral circulation 45.1 (2014): 92–100. Abstract
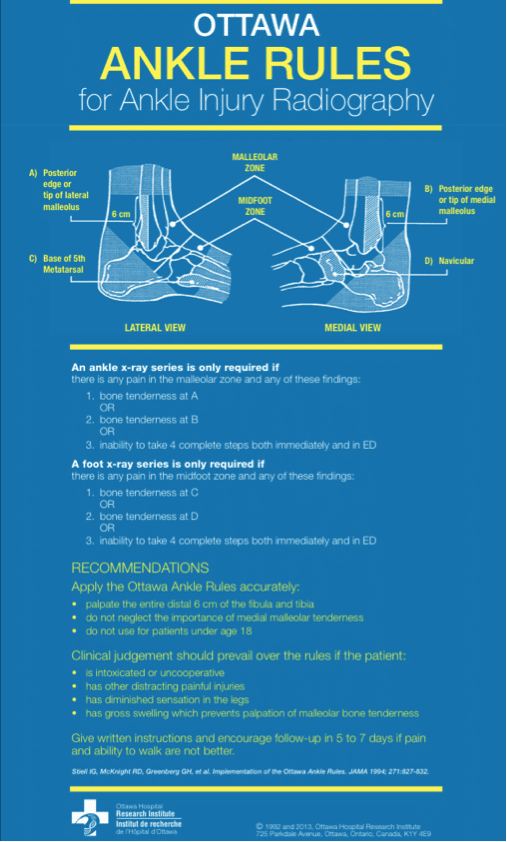
The Ottawa Ankle Rules
Application: A two-way rule to help the physician determine whether a patient with an ankle or foot injury requires an x-ray.
Sensitivity for malleolar fractures: 100%
Sensitivity for midfoot fractures: 100%
Inclusion Criteria:
- Adult patient *note that the Ottawa Ankle rules have been validated in Pediatrics
- Any mechanism of blunt ankle injury (including twisting, falls and direct blows)
Exclusion Criteria:
- Age <18
- Pregnant
- Isolated skin injury
- Injury older than 10 days
- Returning for reassessment of same injury
- Referred from outpatient clinic with existing radiographs
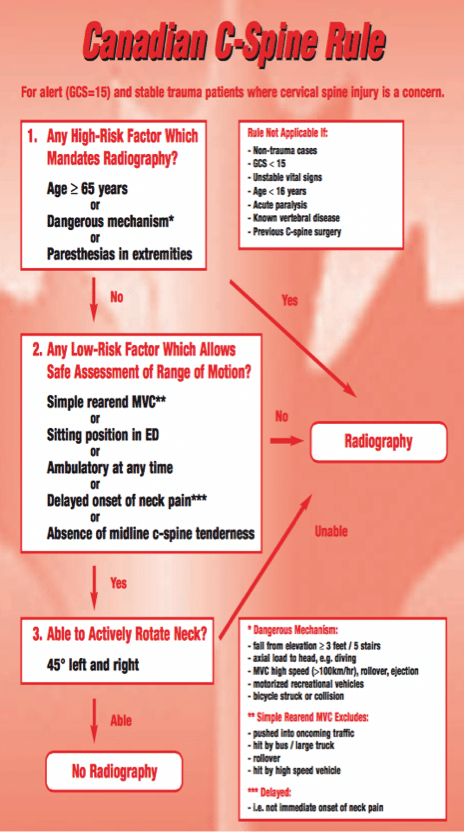
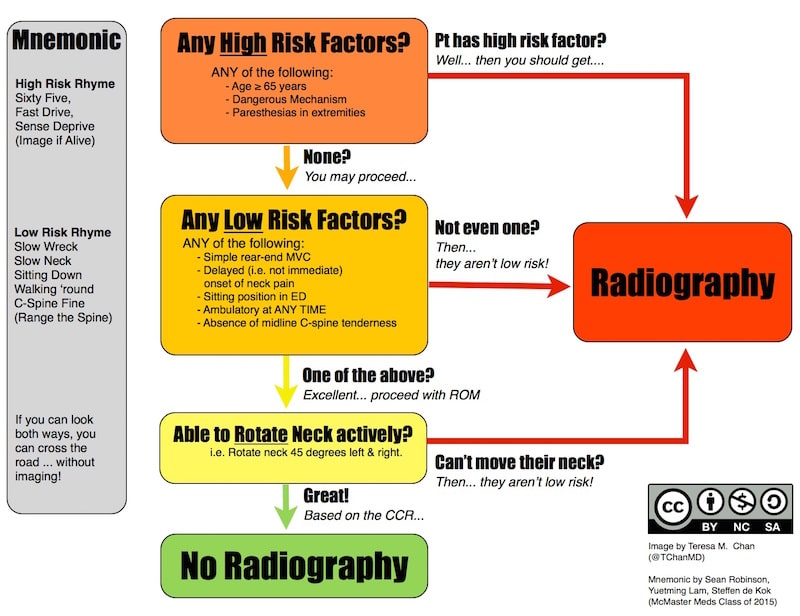
Canadian C-Spine Rule
Application: A two-way rule to help the physician determine whether a patient with blunt head or neck trauma requires imaging of the C-Spine.
Sensitivity for clinically important C-Spine injury: 100%
Specificity for clinically important C-Spine injury: 42.5%
Inclusion Criteria:
- Adult patient
- Acute blunt trauma to the head or neck
- Alert (GCS 15)
- Stable (normal vital signs with SBP>90 mmHg and RR 10-24/min)
- Neck pain
- If no neck then all the following:
- Visible injury above clavicle
- Had not been ambulatory
- Dangerous mechanism of injury
Exclusion Criteria
- Age <16
- GCS < 15
- Isolated minor injuries (laceration)
- Grossly abnormal vital signs
- Injury > 48hr ago
- Penetrating trauma
- Presenting with acute paralysis
- Known vertebral disease
- Return for reassessment of same injury
- Pregnant
http://boringem.org/2014/09/11/boring-question-which-low-risk-c-spine-rule-best/
Great Mnemonic and easy algorithm by Teresa Chan on Boring EM Here
Canadian CT Head Rule
Application: A two- way rule to help physicians determine whether a patient presenting with a minor head injury requires CT imaging of the head.
Sensitivity: The five high risk factors have 100% sensitivity for predicting neurological intervention. All seven factors in the rule have a sensitivity of 98.4% for predicting clinically important brain injury.
Specificity: The high risk factors have 68.7% specificity for predicting neurological intervention All seven factors in the rule have a specificity of 49.6% for predicting clinically important brain injury.
Inclusion Criteria:
- Blunt trauma to the head resulting in witnessed loss of consciousness, definite amnesia or witnessed disorientation
- Initial ED GCS ≥13
- Injury occurred within 24 hours
Exclusion Criteria:
- Age
- Minimal head injury (no LOC, amnesia or disorientation)
- No clear history of trauma as primary event
- Obvious penetrating skull injury or depressed skull fracture
- Acute focal neurological deficit
- Unstable vital signs associated with major trauma
- Seizure before assessment in ED
- Bleeding disorder or use of oral anticoagulants
- Return for assessment of same head injury
- Pregnant
An analysis of Dr. Stiell’s paper comparing the Ottawa CT Head rule with the New Orleans rule here
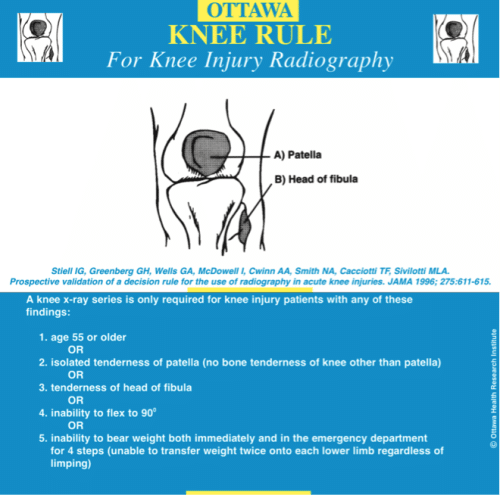
The Ottawa Knee Rule
Application: A two- way rule to help physicians determine whether a patient presenting with an acute knee injury requires radiography.
Sensitivity for knee fractures: 100%
Specificity for knee fractures: 54%
Inclusion Criteria:
- Adult patients
- Blunt knee injury of any mechanism
- Knee defined as: patella, head and neck of the fibula, proximal 8cm of the tibia and distal 8cm of the femur
Exclusion Criteria:
- Age < 18
- Pregnant
- Isolated injury of the skin without underlying soft-tissue or bone involvement
- Referred with radiographs
- Sustained injury > 7 days ago
- Returned for reassessment of the same injury
- ALOC
- Paraplegic
- Multiple trauma
For more on the Stiell Sessions on EM Cases:
Episode 56 The Stiell Sessions: Clinical Decision Rules and Risk Scales
References
Stiell, Ian G et al. “Implementation of the Ottawa ankle rules.” Jama 271.11 (1994): 827-832. Article
Anis, Aslam H et al. “Cost-effectiveness analysis of the Ottawa Ankle Rules.” Annals of emergency medicine 26.4 (1995): 422-428.Plint, Amy C et. Article
Bachmann, Lucas M et al. “Accuracy of Ottawa ankle rules to exclude fractures of the ankle and mid-foot: systematic review.” Bmj 326.7386 (2003): 417. Full pdf
Stiell, Ian G et al. “The Canadian C-spine rule for radiography in alert and stable trauma patients.” Jama 286.15 (2001): 1841-1848. Full pdf
Stiell, Ian G et al. “The Canadian C-spine rule versus the NEXUS low-risk criteria in patients with trauma.” New England Journal of Medicine 349.26 (2003): 2510-2518. Full pdf
Stiell, Ian G et al. “The Canadian CT Head Rule for patients with minor head injury.” The Lancet 357.9266 (2001): 1391-1396. Full text
Stiell, Ian G et al. “Derivation of a decision rule for the use of radiography in acute knee injuries.” Annals of emergency medicine 26.4 (1995): 405-413. Full pdf
Stiell, Ian G et al. “Implementation of the Ottawa Knee Rule for the use of radiography in acute knee injuries.” Jama 278.23 (1997): 2075-2079. Full pdf
Stiell, Ian G et al. “Clinical characteristics associated with adverse events in patients with exacerbation of chronic obstructive pulmonary disease: a prospective cohort study.” Canadian Medical Association Journal (2014): cmaj. 130968. Full pdf
Stiell, Ian G et al. “A risk scoring system to identify emergency department patients with heart failure at high risk for serious adverse events.” Academic Emergency Medicine 20.1 (2013): 17-26. Full pdf
Perry, Jeffrey J et al. “A Prospective Cohort Study of Patients with Transient Ischemic Attack to Identify High-Risk Clinical Characteristics.” Stroke; a journal of cerebral circulation 45.1 (2014): 92–100. Abstract
Dr. Helman and Dr. Stiell have no conflicts of interest to declare except that Dr. Stiell is funded by the Ottawa Research Institute for his research






[…] about checklists for these studies. If podcasts are more your bag there is a great interview here courtesy of Emergency Medicine cases. The authors do not mention these checklists but do comment on […]