Are we all rowing in the same direction for optimal patient flow?
“We have met the enemy and he is us.”—Pogo
It is both an evidence-based truth and almost a mantra of ED providers and leaders that the major cause of ED overcrowding is boarded patients. Yet in Ontario, based on the provincial government’s Pay for Results Program that was designed to reduce ED wait times, we have 10 years of experience from more than 70 EDs that demonstrated impressive flow gains can be achieved despite a poor flow of admitted patients out of the ED. While I have always been and continue to be an advocate for improved admission processes and better ED resources, these issues should never excuse us from exploring our own role in improving flow in our departments. Fostering a culture in which all staff are committed to improving care through better flow will trump petty concerns about hierarchies and role descriptions—and it will improve morale.
In this guest post, Crystal McLeod, a registered nurse who is completing her master’s degree in nursing in Ontario, Canada, describes seven strategies that staff nurses can implement to help improve flow in EDs. In addition to the strategies she presents, the call for action that permeates this post truly resonates with me; when the ED is backed up and patients are suffering, we all need to do something to improve flow!
—Dr. Howard Ovens, December 2017
Improving Patient Flow in the ED: Seven Strategies for Nurses
Over the course of my career as an ED staff nurse I have enjoyed providing excellent care and making a meaningful difference in another person’s life. Yet I have also witnessed critically ill patients experiencing delays in care, patients leaving the ED without being seen after hours of waiting, and parents going home with their discharged child without receiving important counselling due to a lack of time. A serious source of these problems is poor patient flow in the ED.
Improving patient flow in the ED is a worthwhile pursuit for staff nurses, but with limited leadership opportunities and financial resources this may seem to be a daunting challenge. In this blog post I offer seven strategies designed specifically to help ED staff nurses improve patient flow. There is no guide on this subject and limited evidence, but these strategies reflect what I have learned in practice: Staff nurses can improve patient flow through changes that promote efficiency and resource optimization. [3, 6, 9-12] Here are my seven strategies.
#1 Diminish bed holds
ED staff nurses often like to keep a bed or two open at all times for emergencies, a practice we call “bed holding.” [13-14] Bed holding can be practical, but it can also be harmful by causing more patients to leave the ED without being seen, longer delays in care, and poorer patient flow. [4-5] Even a delay of several minutes when placing each patient in an ED bed can translate into hours of additional time in the waiting room over the course of a day.
For ED staff nurses, reducing the length of time ED beds are held and improving the overall flow of patients into the department can occur through small changes in how ED beds are filled. These changes include:
- Filling beds despite physician wait times
Though the patient may not be seen right away, the patient will be accessible immediately once the physician is ready. As well, placing the patient directly in an ED bed allows staff to monitor them more closely and provides time to prepare them for assessment, such as having the patient change into a gown. [7]
- Asking housekeeping for assistance in cleaning beds
If you are busy with nursing tasks and have a full waiting room, get help from housekeeping to clean dirty beds to have the beds ready sooner and diminish the time they are empty.
- Filling rooms before taking a break
Leaving empty beds in your area when going on break may seem like less work for the staff nurse covering your assignment, but could create unintended delays. Instead, try to fill empty rooms before you go on break to ensure your lunch is not a barrier to patients being seen.
- Moving supplies based on patient need
ED beds are sometimes left empty because staff nurses wait to match the patient with the correctly themed room for their presenting injury. For example, ED staff nurses may avoid placing a patient with an eye injury in the casting room. In these scenarios you can increase your flexibility by moving the needed supplies into whatever room is available.
#2 Assist patients being discharged
When patients are being discharged, ED team members may inadvertently cause delays in emptying ED beds due to poor communication in signalling the end of a visit and in answering questions. Both can result in the awkward moment where a patient doesn’t know when to leave. To avoid this confusion, ED nurses can simply step into a patient’s room and ask if they need anything before they go. Since patients like to ask questions during this last check in, I have developed the habit of bringing educational materials with me so I can provide efficient and timely discharge teaching. [13-15]
If a patient requires assistance dressing, needs a mobility aide, or requires access to a phone before discharge, having staff nurses step up to complete these tasks can dramatically improve patient flow, too. [13-14]
#3 Assess flow culture in your ED
The nursing staff in every ED have a collective way of understanding their role, carrying out tasks, and managing team dynamics in the workplace. [13] As flow culture differs from one ED to another, there is value in having staff nurses assess how the manner in which their work is organized can affect patient flow and potentially create delays in patient care. [13] This way, any future changes in the ED can take into consideration the local style of nursing.
Though the assessment of nursing work and flow culture may sound complicated, it can be done quickly by just asking fellow colleagues, “What part of your work slows you down in terms of seeing patients?” [7,13] With the permission of management, I have posed this question in workplace satisfaction surveys so colleagues can answer anonymously and without fear of reprimand. If your department is open to sharing ideas and comfortable with being honest, an ED staff meeting may also provide a conducive platform for assessing nurses’ thoughts on flow culture. On the other hand, if you feel inefficiencies in your flow culture have been accepted as the norm in your ED, asking someone outside of the department for their assessment may be beneficial. [3, 7,13, 16]
#4 Balance admissions
Most EDs operate on the principle that equal patient occupancy, often determined by the number and acuity of patients, satisfies the requirement of sharing work fairly among nurses. [1] In some circumstances this can be true, but when the task of handling admitted patients repeatedly falls to the same nurses their workload increases substantially and can cause delays in their area of the ED. [1, 17] Their workload is relatively heavy as tasks such as handling paperwork, reconciling medications, starting new medications, and performing procedures are all heightened in the first day of admission. [1]
To get around heavy patient workloads and keep patients flowing through all areas of the ED, I recommend having nursing staff share responsibility for admissions. By sharing I mean reassessing which nurse will care for admitted patients as physicians identify these patients. Often, triage nurses cannot determine who will be admitted and who will not, so nurses working in the main department should be able to offload admitted patients to colleagues to ensure equal completion of admissions. [1, 5, 19] Ideally, this strategy would be implemented through charge staff, who could reassign admitted patients from a staff nurse who has multiple patients to a nurse who has none. [5, 19] A staff nurse experiencing a lighter workload could also take the initiative by assisting a colleague with multiple admissions or, conversely, ask for help from a colleague when having to coordinate multiple admissions.
#5 Stay in the loop on ED changes
Changes occur all the time in the ED that affect the work of nurses and, in turn, patient flow. [20] In the past, physicians and nurse managers have not always effectively predicted how changes will affect nursing or known how to advocate for improvements in patient flow from the perspective of staff nurses. [11, 20] Therefore, I recommend steering committees charged with facilitating any ED change should include nursing staff, and nursing staff should jump at the chance to sit on these committees. [7, 14, 20]
Once they join a steering committee, ED staff nurses have the opportunity to share concerns and educate others about how nursing affects patient flow for the entire ED. [7, 21] If a staff nurse on a steering committee foresees a change being unpopular among ED nurses, then this nurse should put forward ideas for improving implementation success. [2, 7] These ideas may include seeking assistance from a trusted nursing organization or selecting respected staff nurses to pilot the change. [20-22]
#6 Implement a patient communication system
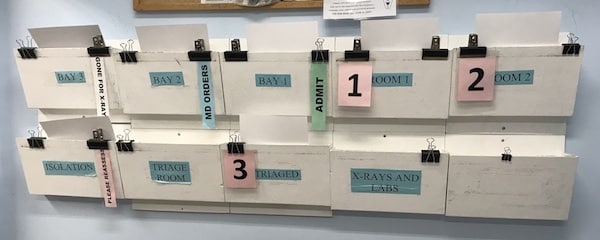
A patient communication system is any method that conveys the status of ED patients clearly and simultaneously to all team members. I have seen a variety of these systems, ranging from electronic white boards that update with changes in patient status to colour-coded clipboards that denote the patient’s triage acuity. Patient communication systems do not have to be elaborate but should help ED staff regularly account for patients, communicate outstanding tasks, and minimize disruptions to individual team members’ work flows. [23] In the ED where I work, staff simply swap out laminated paper cards (attached to charts with clips) as change occurs with the patient. Cards labelled 1, 2, 3 (etc.) and “Reassess” indicate which patients are waiting to be seen, while other cards stating “MD Orders,” “Transfer,” and “Admit” direct staff nurses.
Having worked in EDs with, without, and in the process of implementing a communication system, I feel confident in saying that once implemented successfully a communication system can greatly improve patient flow at low cost. All you really need are some paper and clips to get started. Implementation can be tedious as staff learn to use the system consistently, and time must be invested to educate the ED team on how to use the chosen communication system. Some staff will get discouraged and want to revert back to the old way, but persevere. Once the system is implemented, you’ll find you no longer have to interrupt colleagues or wait around to provide patient updates.
#7 Follow medical directives consistently
Medical directives, or pre-existing clinical guidelines, can be used to direct radiology, lab orders, medication administration, and nursing care in the ED and can speed up patient care. [4-5] However, medical directives arise from a physician’s scope of practice and cannot be created by an individual nurse. So, does this mean staff nurses have no influence over how medical directives affect patient flow? Absolutely not.
If you work in an ED with medical directives, ensure they are being used to their maximal potential by knowing them inside out. Even if you have only five, review them regularly and apply them to all eligible patients consistently. If you work in an ED without medical directives but think they would improve patient flow, consider approaching the ED medical staff. The Ontario Hospital Association offers an Emergency Department (ED) Medical Directives Implementation Kit that provides guidance to ED medical staff during the design, approval, and implementation of directives. [24] Reviewing this document before meeting with ED medical staff can be helpful when proposing and discussing new directive ideas.
What you do matters
Improving ED patient flow is a task that requires continuous effort from both departmental staff and hospital leadership. [7] However, the burden of this task can be alleviated by specifically calling on ED staff nurses to share in the governance, design, and implementation of changes to improve patient flow. [3] Even small changes in resource optimization from each individual nurse can cause dramatic improvements in ED patient flow. [3]
For staff nurses, strategies to improve patent flow in your ED are limited only by your creativity. [14] The seven strategies I have suggested in this post are meant to serve as jumping-off points and to start a conversation about what staff nurses in your ED could do to improve patient flow. Having a similar interest in improving patient flow, ED leaders may support your ideas with policy and turn your individual actions into a consistent practice among all ED staff. [1, 21] Ultimately, the potential to make individual changes and establish interest in patient flow projects rests with you.
—Crystal McLeod is in the final year of her master’s degree in nursing at Western University in London, Ontario. She has also worked for several years as a registered nurse in rural and remote emergency departments across Ontario.
Disclaimer: This blog post is the author’s own and does not represent the positions, strategies, or opinions of the author’s employer.
References
- Armony M, Israelit S, Mandelbaum A, Marmor YN, Tseytlin Y, Yom-Tov GB. On patient
flow in hospitals: A data-based queueing-science perspective. Stochastic Systems. 2015;5(1):
146-194. doi:10.1214/14-SSY153
- Carter EJ, Pouch SM, Larson EL. The relationship between emergency department crowding
and patient outcomes: A systematic review. J Nurs Scholarsh. 2014;46(2):
106-115. doi:10.1111/jnu.12055
- Sayah A, Lai-Becker M, Kingsley-Rocker L, Scott-Long T, O’Connor K, Lobon, LF.
Emergency department expansion versus patient flow improvement: Impact on patient
experience of care. J Emerg Med. 2016;50(2):339–348. doi:10.1016/j.jemermed.2015.06.068
- Van Der Linden MC, Khursheed M, Hooda K, Pines JM, Van Der Linden N. Two emergency
departments, 6000 km apart: Differences in patient flow and staff perceptions about crowding.
Int Emerg Nurs. 2017;In Press. doi: 10.1016/j.ienj.2017.06.002
- Alexander D, Abbott L, Zhou Q, Staff I. Can triage nurses accurately predict patient
dispositions in the emergency department? J Emerg Nurs. 2016;42(6):513-518.
doi:10.1016/j.jen.2016.05.008
- Fulbrook P, Jessup M, Kinnear F. Implementation and evaluation of a ‘Navigator’ role to
improve emergency department throughput. Australas Emerg Nurs J. 2017;20(3):114-121.
doi:10.1016/j.aenj.2017.05.004
- McHugh M, Van Dyke K, McClelland M, Moss D. Improving patient flow and reducing
emergency department crowding: A guide for hospitals. AHRQ Publication No. 11(12)-0094.
Rockville, MD: Agency for Healthcare Research and Quality, 2011.
- Stang AS, Crotts J, Johnson DW, Hartling L, Guttmann A. Crowding measures associated
with the quality of emergency department care: A systematic review. Acad Emerg Med. 2015;22(6):643-656. doi:10.1111/acem.12682
- Leslie K. “Ontario nurses warn of increased risk of patients dying due to hospital cuts and
- Innes K, Jackson D, Plummer V, Elliott D. Emergency department waiting room nurse role:
A key informant perspective. Australas Emerg Nurs J. 2017;20(1):6–11.
doi:10.1016/j.aenj.2016.12.002
- Shindul-Rothschild J, Read CY, Stamp KD, Flanagan J. Nurse staffing and hospital
characteristics predictive of time to diagnostic evaluation for patients in the emergency
department. J Emerg Nurs. 2017;43(2):138-144. doi:10.1016/j.jen.2016.07.003
- Kirk JW. Implementing evidence-based practices in an emergency department:
Contradictions exposed when prioritising a flow culture. J Clin Nurs. 2016;
25(3):555-565. doi:10.1111/jocn.13092
- Christensen M, Rosenberg M, Mahon E, Pineda S, Rojas E, Soque V, et al. Pivot nursing: An
alternative to traditional ED triage. J Emerg Nurs. 2016;42(5):395-399.
doi:10.1016/j.jen.2015.07.014
- Wolters Kluwer Health. Lexicomp Online. 2017. http://www.wolterskluwercdi.com/lexicom
- Gipp NJ. Keeping the team happy protecting colleagues from a deluge of difficulties is not
the only job of a good manager. Emerg Nurse. 2016;24(5):15. doi:10.7748/en.24.5.15.s18
- Hamilton R. Nurses’ knowledge and skill retention following cardiopulmonary resuscitation
training: A review of the literature. J Adv Nurs. 2005;51(3):288-297.
doi:10.1111/j.1365-2648.2005.03491.x
- Feldman R, Warfield TA. Disagreement. Oxford, UK: Oxford University Press, 2010.
- Ming T, Lai A, Lau PM. Can team triage improve patient flow in the emergency department?
A systematic review and meta-analysis. Adv Emerg Nurs J. 2016;38(3):233-250. doi:10.1097/TME.0000000000000113
- Bonalumi NM, Bhattacharya A, Edwards C, Fasnacht A, Mazzone L, Stephens K, et al.
Impact of a planned workflow change: Super track improves quality and service for low-
acuity patients at an inner-city hospital. J Emerg Nurs. 2017;43(2):114-125.
doi:10.1016/j.jen.2016.03.029
- Rainford WC, Wood S, McMullen PC, Philipsen ND. The disruptive force of lateral violence
in the health care setting. J Nurse Pract. 2015;11(2):157-164.
doi:10.1016/j.nurpra.2014.10.010
- Van Donk P, Tanti ER, Porter JE. Triage and treat model of care: Effective
management of minor injuries in the emergency department. Collegian. 2017;24(4):325-330. doi:10.1016/j.colegn.2016.05.003
- Cheung DS, Kelly JJ, Beach C, Berkeley RP, Bitterman RA, Broida RI, et al. Improving
handoffs in the emergency department. Ann Emerg Med. 2010;55(2):171-180. doi:10.1016/j.annemergmed.2009.07.016
- Ovens H, Stevenson K, Cheung W, Dushenski D, Eisen J, Farquharson C, et al. Emergency
Department (ED) Medical Directives Implementation Kit. Ontario Hospital Association, 1-121. https://www.oha.com/Professional%20Issues1/ED%20Medical%20Directives%20Implementation%20Kit.pdf





We need more nurses to join the conversation on Access Block in the ED. Thank you for the ideas and keep the conversation flowing.
The process of bed holding is an interesting phenomenon. While I am in agreement with Crystal re avoiding “bed holding,” I am curious to see how it impacts key metrics, such as ALOS, time to physician, time to nurse, time to EKG, time from ED bed to inpatient space. Do you know if such data exists?