Episode 75 Decision Making in EM – Cognitive Debiasing, Situational Awareness & Preferred Error
While knowledge acquisition is vital to developing your clinical skills as an EM provider, using that knowledge effectively for decision making in EM requires a whole other set of skills. In this EM Cases episode on Decision Making in EM Part 2 - Cognitive Debiasing, Situational Awareness & Preferred Error, we explore some of the concepts introduced in Episode 11 on Cognitive Decision Making like cognitive debiasing strategies, and some of the concepts introduced in Episode 62 Diagnostic Decision Making Part 1 like risk tolerance, with the goal of helping you gain insight into how we think and when to take action so you can ultimately take better care of your patients. Walter Himmel, Chris Hicks and David Dushenski answer questions such as: How do expert clinicians blend Type 1 and Type 2 thinking to make decisions? How do expert clinicians use their mistakes and reflect on their experience to improve their decision making skills? How can we mitigate the detrimental effects of affective bias, high decision density and decision fatigue that are so abundant in the ED? How can we use mental rehearsal to not only improve our procedural skills but also our team-based resuscitation skills? How can we improve our situational awareness to make our clinical assessments more robust? How can anticipatory guidance improve the care of your non-critical patients as well as the flow of a resuscitation? How can understanding the concept of preferred error help us make critical time-sensitive decisions? and many more important decision making in EM nuggets...
Episode 74 Opioid Misuse in Emergency Medicine
Pain leads to suffering. Opioid misuse leads to suffering. We strive to avoid both for our patients. On the one hand, treating pain is one of the most important things we do in emergency medicine [...]
Episode 73 Emergency Management of Pediatric Seizures
Pediatric seizures are common. So common that about 5% of all children will have a seizure by the time they’re 16 years old. If any of you have been parents of a child who suddenly starts seizing, you’ll know intimately how terrifying it can be. While most of the kids who present to the ED with a seizure will end up being diagnosed with a benign simple febrile seizure, some kids will suffer from complex febrile seizures, requiring some more thought, work-up and management, while others will have afebrile seizures which are a whole other kettle of fish. We need to know how to differentiate these entities, how to work-them up and how to manage them in the ED. At the other end of the spectrum of disease there is status epilepticus – a true emergency with a scary mortality rate - where you need to act fast and know your algorithms like the back of your hand. This topic was chosen based on a nation-wide needs assessment study conducted by TREKK (Translating Emergency Knowledge for Kids), a collaborator with EM Cases. With the help of two of Canada’s Pediatric Emergency Medicine seizure experts hand picked by TREKK, Dr. Lawrence Richer and Dr. Angelo Mikrogianakis, we’ll give you the all the tools you need to approach the child who presents to the ED with seizure with the utmost confidence.
Episode 72 ACLS Guidelines 2015 Post Arrest Care
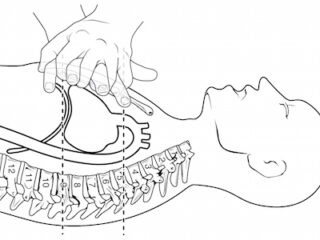
Once we've achieved ROSC our job is not over. Good post-arrest care involves maintaining blood pressure and cerebral perfusion, adequate sedation, cooling and preventing hyperthermia, considering antiarrhythmic medications, optimization of tissue oxygen delivery while avoiding hyperoxia, getting patients to PCI who need it, and looking for and treating the underlying cause. Dr. Lin and Dr. Morrison offer us their opinion on the new simplified approach to diagnosing the underlying cause of PEA arrests. We'll also discuss when it's time to terminate resuscitation or 'call the code' as well as some fascinating research on gender differences in cardiac arrest care. These co-authors of the guidelines will give us their vision of the future of cardiac arrest care and we'll wrap up the episode with a third opinion, so to speak: Dr. Weingart's take on the whole thing....
Episode 71 ACLS Guidelines 2015 – Cardiac Arrest Controversies Part 1
A lot has changed over the years when it comes to managing the adult in cardiac arrest. As a result, survival rates after cardiac arrest have risen steadily over the last decade. With the release of the 2015 American Heart Association ACLS Guidelines 2015 online on Oct 16th, while there aren’t a lot a big changes, there are many small but important changes we need to be aware of, and there still remains a lot of controversy. In light of knowing how to provide optimal cardio-cerebral resuscitation and improving patient outcomes, in this episode we’ll ask two Canadian co-authors of The Guidelines, Dr. Laurie Morrison and Dr. Steve Lin some of the most practice-changing and controversial questions.
Episode 70 End of Life Care in Emergency Medicine
Most of us in North America live in cultures that almost never talk about death and dying. And medical progress has led the way to a shift in the culture of dying, in which death has been medicalized. While most people wish to die at home, every decade has seen an increase in the proportion of deaths that occur in hospital. Death is often seen as a failure to keep people alive rather than a natural dignified end to life. This is at odds with what a lot of people actually want at the end of their lives: 70% of hospitalized Canadian elderly say they prefer comfort measures as apposed to life-prolonging treatment, yet as many as ⅔ of these patients are admitted to ICUs. Quality End of Life Care in Emergency Medicine is not widely taught. Most of us are not well prepared for death in our EDs – and we should be. There’s no second chance when it comes to a bad death like there is if you screw up a central line placement, so you need the skills to do it right the first time. To recognize when comfort measures and compassion are what will be best for our patients, is just as important as knowing when to intervene and treat aggressively in a resuscitation. Emergency physicians should be able to recognize not only the symptoms and patterns that are common in the last hours to days of life, but also understand the various trajectories over months or years toward death, if they’re going to provide the high quality end of life care that patients deserve. So, with the help of Dr. Howard Ovens, a veteran emergency physician with over 25 years of experience who speaks at national conferences on End of Life Care in Emergency Medicine, Dr. Paul Miller, an emergency physician who also runs a palliative care unit at McMaster University and Dr. Shona MacLachlan who led the palliative care stream at the CAEP conference in Edmonton this past June, we'll help you learn the skills you need to assess dying patients appropriately, communicate with their families effectively, manage end of life symptoms with confidence and much more...