Pain leads to suffering. Opioid misuse leads to suffering.
We strive to avoid both for our patients.
On the one hand, treating pain is one of the most important things we do in emergency medicine to help our patients and we need to be aggressive in getting our patients’ pain under control in a timely, effective, sustained and safe fashion. This was the emphasis 10-20 years ago after studies showed that we were poor at managing pain and our patients were suffering. On the other hand, opioid dependence, addiction, abuse and misuse are an enormous public health issue. Opioid misuse in Emergency Medicine has become a major problem in North America over the past 10 years at least partly as a reaction to the years that we were being told that we were failing at pain management. As Dr. Reuben Strayer said in his SMACC talk on the topic:
“Opioid misuse explodes in our face on nearly every shift, splattering the entire department with pain and suffering, and addiction and malingering and cursing and threats and hospital security, and miosis and apnea and naloxone and cardiac arrest.”
So how do we strike a balance between managing pain effectively and providing the seed for perpetuating a drug addiction or feeding a pre-existing drug addiction? How do we best take care of our patients who you suspect might have an opiod misuse problem? To help us sort through this difficult conundrum we have Dr. David Juurlink, a toxicologist and Dr. Reuben Strayer an EM physician, who both a special interest in opioid misuse.
Written Summary & blog post prepared by Keerat Grewal, edited by Anton Helman, December 2015
Cite this podcast as: Juurlink, D, Strayer, R, Helman, A. Opioid Misuse in Emergency Medicine. Emergency Medicine Cases. December, 2015. https://emergencymedicinecases.com/opioid-misuse-emergency-medicine/. Accessed [date].
Here are some numbers that may surprise you:
In a recent ED study on opioid prescribing patterns in Annals of EM, 17% of patients in the US were prescribed opioids on discharge from EDs. In Ontario, about 10 people die accidentally from prescription opioids every week. Between 1990 and 2010, drug overdose deaths in the US increased by almost four fold, eclipsing the rate of death from motor vehicle collisions in 2009. This was driven by deaths related to prescription opioids, which now kill more people than heroin and cocaine combined. Opioids are the most prescribed class of medication in the US. In 2010, one out of every eight deaths among persons aged 25 to 34 years was opioid-related. Four out of 5 new heroin users report that their initial drug was a prescription opioid. In Ontario, three times the people died from opiate overdose than from HIV in 2011.
Fig 1: Opioid sales, admissions, and deaths in the U.S.
Who is at risk for Opioid Misuse in Emergency Medicine?
All ED patients are at risk for opiod misuse, regardless of their risk factors. Even opioid-naive patients with no risk factors for opioid misuse are at risk for developing opioid misuse problems.
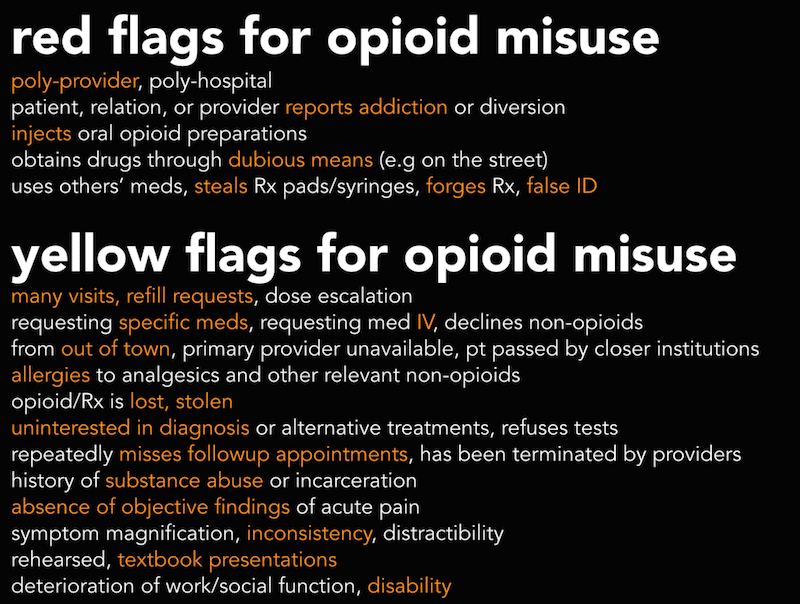
Nonetheless, their are particular risk factors, red and yellow flags that should raise your suspicion for pre-existing opioid misuse and help guide management. (see Figure 2 and 3)
Patients at particularly high risk for opioid misuse include:
- Young age (< 40 years old)
- Psychiatric history
- Substance abuse history
- Benzodiazepine use
Fig 2: Red & Yellow Flags for Opioid Misuse
(courtesy of Dr. R. Strayer)
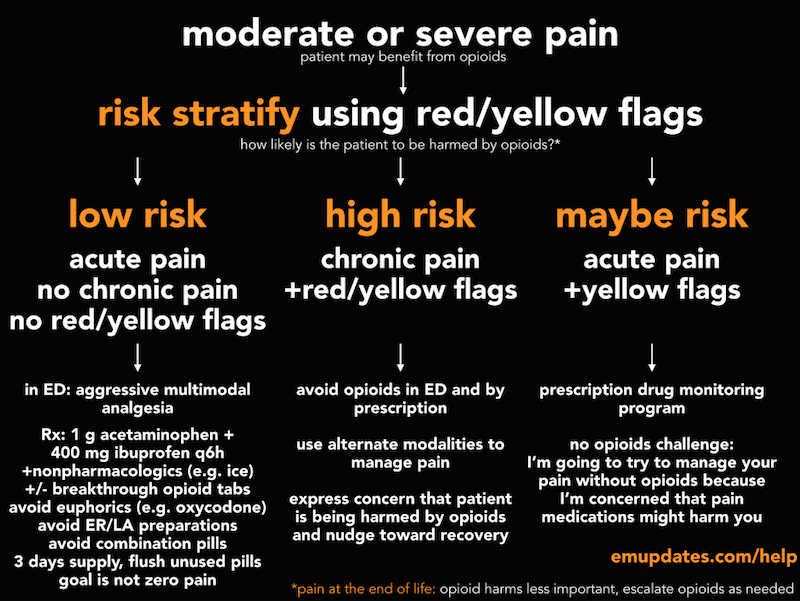
Fig 3: Risk Stratification for Opioid Misuse
(courtesy of Dr. R. Strayer)
Trajectories of Opioid Use in Emergency Medicine
There are various trajectories that patients who are prescribed opioids may follow (see Figure 4). We must consider the risks of prescribing opioids to opioid naive patients, and their risk of opioid misuse. As previously described, even among patients thought to be ‘low risk’ for opioid misuse, some of these patients will develop risky drug behaviours with opioids.
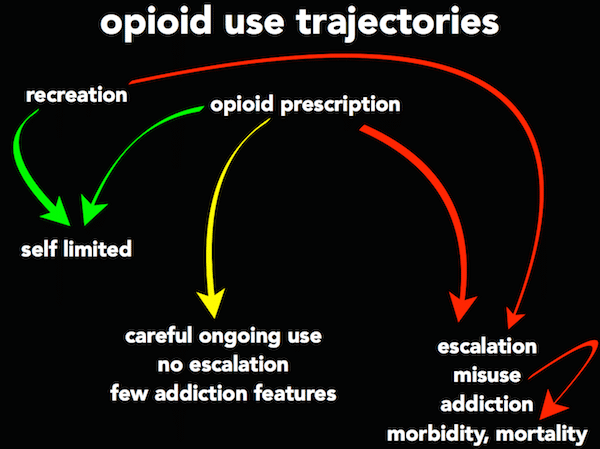
(courtesy of Dr. R. Strayer)
Opioid-Induced Hyperalgesia
Opioid-induced hyperalgesia is a phenomenon that develops in patients who are started on opioids for a condition such as back pain, arthritis, or fibromyalgia, and as the dose is increased, rather than their perceived pain decreasing as might be expected, patients develop marked hyperalgesia. The pathophysiology of this phenomenon is not well understood.
Opioid Misuse Harm Reduction Strategies in the ED
Categories of harm reduction:
- Prevent opioid misuse and dependency in opioid naïve patients
- Reduce the number of opioid pills in the community that are available for misuse and abuse
- Reduce harm and move towards recovery in patients who have evidence of opioid misuse
Key harm reduction techniques:
- Avoid prescribing extended release, long acting preparations of opioids. These types of opioids have been shown to have double the potential for overdose (1).
- Avoid prescribing opioids to patients who are already taking sedatives, particularly benzodiazepines (2).
- Avoid prescribing opioids to patients with alcohol dependency, or patients who are regular benzodiazepine or sedative users, especially if they have a known substance abuse history or history of mental illness.
- Avoid oxycodone (i.e. percocet or percodan). Oxycodone tends to have a side effect of euphoria, therefore, it is more habit forming than oral morphine (3).
- If prescribing opioids, prescribe a small number of pills to last the patient 2-3 days. Opioid dependence can develop within 5 days, and will usually develop within 14 days (4).
- If you know the patient is an IV drug user, do not give them oral opioids. There is a risk that these patients will crush the tablets and use them intravenously, which can result in infectious and thrombotic complications (5).
- Tell patients to discard unused pills immediately, especially if they have adolescents living with them. Many people start their drug addiction in adolescence by experimenting with parent’s opioid prescription pills. Non-medical use of opioids in Ontario is ranked as the 3rd drug of choice for students, and 67% of adolescents report getting these pills from home.
Communication Strategies to Use in Patients with Opioid Misuse in Emergency Medicine
First, Gather Data: Before seeing the patient, gather as much information as possible regarding the patient, including: previous ED visits, pharmacy refills, ‘double-doctoring’, etc.
Set Expectations: Talk to patients about statistics, risks and benefits of opioids.
“My job is to manage your pain, at the same time, I manage the potential for some pain medications to harm you”
Transfer the Blame: Do not blame the patient for opioid misuse.
“Prescription pain medications, even when used as directed, can cause patients to become dependent, and I’m concerned that the pills we prescribed for you in the past, even though you were using them appropriately, you many now be dependent on them.”
“We can help you break free of that dependence”
Ensure patients know that their medical concerns are taken seriously:
“I want to make sure that there is nothing dangerous causing your pain, because that is our main responsibility in the emergency room. I want to relieve your symptoms and make you as comfortable as I can.”
“I will not use opioids to control your pain, because I think opioids will make your condition worse, even if it makes you feel better in the short term.”
“I think using opioids will be harmful to you, so if you want treatment for your pain I am going to try to treat your pain with other types of medicines”
Alternatives to Opioids in Patients who Present to the ED with Acute on Chronic Pain
- Nerve blocks
- NSAIDs
- Ketamine: 0.3mg/kg, 20-30mg for most adults, as an IV drip over 10-20 minutes.
- Droperidol: available in the U.S. In Canada, other antipsychotics, such as haloperidol, may be helpful.
- Intravenous lidocaine: 1-3 mg/kg bolus followed by 1-3 mg/kg/h.
- Gabapentin: for neuropathic pain.
For a discussion on the literature on the opioid-sparing effects of Ketamine go to Journal Jam 4
Pain Management Strategies for Specific Conditions
Consider alternatives to opioids for common presenting complaints. Some treatment strategies our experts suggest for common complaints are listed below.
Mechanical Back Pain: Local anesthetics (i.e. bupivacaine 0.5%, 10cc IM injected directly into the point of maximal pain).
Migraines: Opioids are known not to be useful for improving the pain associated with migraine headaches, and are not routinely recommended. Medications options include: metoclopramide, prochlorperazine, NSAIDs, ergot, tryptans and high flow oxygen (8). Low dose propofol for refractory headaches has been reported to be effective in reducing the pain associated migraine headaches in case series (9).
Dental Pain: Dental block.
Fracture Pain: Combination of acetaminophen and ibuprofen.
Sickle Cell Patients: Pain management in Sickle Cell patients is often challenging. Consider low dose IV ketamine for those patients in whom you suspect opiod misuse.
For an in-depth discussion on managment of Sicle Cell Anemia in the ED go to Episode 68: Management of Sickle Cell Disease in Emergency Medicine
Chronic Abdominal Pain: Haldol, ketamine.
NOTE: These strategies do not apply to palliative and end of life care.
See Episode 70 for a discussion of opioid use in palliative care and end of life care.
Precautions for Prescribing Opioids in Chronic Non-Cancer Pain in the Acute Setting
Adapted from Canadian guideline for safe and effective use of opioids for chronic noncancer pain, 2011 (10)
In general prescribing opioids for chronic pain in the ED should be avoided when possible. If you do prescribe opioids to these patients, consider the following actions:
- Contact the patient’s pharmacy: if you are unable to obtain pharmacy records, or if the patient’s history is inconsistent with information from the pharmacy, do not prescribe opioids.
- Inform the patient that this is a one-time only prescription, and document this in the chart.
- Prescribe a reasonable daily dose that you are comfortable with, even if this is lower than the family physician’s usual prescription.
- Prescribe only enough medication to last until the next working day.
- Send a record of the visit to the patient’s regular doctor.
For more on opioid misuse on EM Cases:
Episode 27: Drugs of Abuse – Stimulants and Opiates
Ep 116 Emergency Management of Opioid Misuse, Overdose and Withdrawal
Best Case Ever 41 Opiate Misuse and Physician Compassion
BCE 76 Opioid Withdrawal
Key References
- Miller M, Barber CW, Leatherman S, et al. 2015. Prescription opioid duration of action and the risk of unintentional overdose among patients receiving opioid therapy. JAMA Intern Med;175(4): 608-15. Full Article
- Morbidity and Mortality Weekly Report. Apr 17, 2015. Poisoning deaths involving opioid analgesics. Centers for Disease Control. Full Article
- Wightman R, Perrone J, Portelli I, Nelson L. 2012. Likeability and abuse liability of commonly prescribed opioids. J Med Toxicol; 8(4):335-40. Full PDF
- Galinkin J, Koh JL. 2014. Recognition and management of iatrogenically induced opioid dependence and withdrawl in children. Pediatrics;133(1): 152-5. Full Article
- Galante JM, Ahmad S, Albers EA, Sena MJ. 2012. Trauma and substance abuse: Deadly consequences of intravenous Percocet tablets. J Emerg Med;43(3):167-9. Abstract
- Gomes T, Juurlink DN, Yao Z. 2014. Impact of legislation and a prescription monitoring program on the prevalence of potentially inappropriate prescriptions for monitored drugs in Ontario: A time series analysis. CMAJ Open;2(4):256-61. Full PDF
- Dormuth CR, Miller TA, Juang A, Mamdani MM, Juurlink DN. 2012. Effect of a centralized prescription network on inappropriate prescriptions for opioid analgesics benzodiazepines. CMAJ;184(16):852-6. Full PDF
- Ozkurt B, Cinar O, Cevik E, et al. Efficacy of high-flow oxygen therapy in all types of headache: a prospective, randomized, placebo-controlled trial. Am J Emerg Med. 2012;30(9):1760-4. Abstract
- Soleimanpour H, Taheraghdam A, Ghafouri RR, Taghizadieh A, Marjany K, Soleimanpour M. Improvement of refractory migraine headache by propofol: case series. Int J Emerg Med. 2012;5(1):19. Full PDF
- Kahan M, Wilson L, Mailis-gagnon A, Srivastava A. Canadian guideline for safe and effective use of opioids for chronic noncancer pain: clinical summary for family physicians. Part 2: special populations. Can Fam Physician. 2011;57(11):1269-76, e419-28. Full PDF
Dr. Helman, Dr. Juurlink & Dr. Strayer have no conflicts of interest to declare
Additional FOAMed Resources on Opioid Misuse
Emergency Medicine Updates: Opioid Misuse
http://emupdates.com/helpcard-and-opioid-misuse/
Academic Life in Emergency Medicine: Initial pain medication options in the emergency department
http://www.aliem.com/pv-card-initial-pain-medication-options/
Mike Evans: Best advice for people considering or taking opioid pain medications
http://knowledgex.camh.net/videos/Pages/best_advice_opioids_evans.aspx
The Skeptics’ Guide to EM: Chase the Dragon and Naloxone
http://thesgem.com/2017/05/sgem179-chase-the-dragon-and-naloxone/
https://www.youtube.com/watch?v=7Na2m7lx-hU
Now test your knowledge with a quiz.






[…] Medicine Cases takes on opioid misuse in the emergency department. […]
Working as an ED nurse I don’t hold the prescribing pen, but I thoroughly enjoyed this episode and was happy to be educated on the issue- as a patient advocate I want to make sure my patients are getting the best medication/treatment. Now as I move forward with this new information I find myself trying to discuss this topic further in my workplace and explore what role we have in preventing opioid misuse and abuse. Though one major one issue I have run up against where I work is the use of long-acting narcotics for acute pain, in patients who have never taken before a long acting agent and don’t have chronic pain. From this episode I realize that long acting oral agents can be harmful due to their high risk for overdose, yet my fellow colleagues assure me that the risk for abuse/misuse is higher with short acting oral opioid preparations, like statex or oral morphine, and therefore they should be avoided. I have looked around for research to help decide on this issue, but am coming up with little. Any suggestions? Will misuse potential develop faster in patients taking short acting or long acting preparations? How does this factor weigh on the risk for overdose? I just feel odd about giving hydromorph contin or M-elson to patients with pain that is episodic without knowing all the risks. Thanks! Crystal
Thanks for your comments Crystal. The most important step to take to reduce opioid misuse cause by/perpetuated by acute care providers is to prescribe opioids to fewer opioid naive patients, and in opioid naive patients in whom you think prescription opioids are indicated, prescribe fewer opioids.
The literature suggests that immediate release oxycodone and hydrocodone are more abuse-prone than alternative immediate release preparations. The literature also demonstrates that extended release preparations are powerfully associated with overdose mortality; of course controlled-release oxycodone (Oxycontin) is the patriarch of prescription opioid misuse.
There are some who feel that immediate release opioids are more likely to foster addiction than extended release preparations, because IR pharmacokinetics provide a “spike” in opioid levels where ER pills deliver their components more slowly. I do not think that there is literature to guide us on this specific question, in opioid-naive patients. The opioid spike theory makes some sense, but so does the idea that ER preparations saturate the opioid receptors continuously, causing a more powerful cellular/neurotransmitter adaptive response that is crucial to the pathophysiology of addiction. Bottom line is that I don’t think we know the answer to that question but we do know ER opioids are much more likely to kill people overall, so it makes sense to avoid them.
But again, much more important than choosing IR vs. ER or oxy vs. something else (avoid oxycodone) is to prescribe to fewer patients. The vast majority of patients currently discharged from american/canadian emergency departments with opioids would do very well with non-opioid analgesia, which confers no addiction risk.
Thanks so much, that all makes sense! I definitely agree this issue is a battle against two evils, both to be avoided as much as possible. Appreciate your time, Crystal
I found this episode fascinating. I’m not a medical professional, but I have a syndrome which causes chronic pain from frequent joint dislocations, diagnosed during childhood. At the time, my parents decided that I was not to take opioids, and I am very grateful. I imagine I would have been dependent by the time I was a teenager, as some other patients are. To laypeople, parents can seem abusive when denying these drugs and not wanting their children to develop dependence. Do you manage pediatric cases differently, and if so, how? I would be interested in a follow-up episode. Thanks for such an interesting podcast.
Thanks for sharing your personal experience Mila. This is exactly the kind of thing physicians need to hear. While there is some evidence that poor pain control in the Emergency Department for acutely painful conditions in children leads to heightened pain sensitivity as an adult, I am not aware of any literature for chronic pain outside the ED. We have done an episode on pediatirc pain management (https://emergencymedicinecases.com/pediatric-pain-management/), but did not address patients with chronic pain conditions specifically.
Hello. Can you suggest any scholarly articles on how medical decision making goes up when the patient is an infant or a child under the age of 8?