In this ECG Cases blog we look at 10 cases of T-wave inversion, with an approach and mnemonic to determine the underlying cause.
Written by Jesse McLaren; Peer Reviewed and edited by Anton Helman. June 2021
10 patients presented with T-wave inversion. What was the cause?
Case 1: 50yo with 5 days of intermittent chest pain. Normal vitals.
Case 2: 70yo with one day of chest pain. Normal vitals. Old then new ECG
Case 3: 65yo with shoulder pain. Normal vitals. Old then new ECG
Case 4: 90yo with 2 days epigastric pain and nausea. HR 50 BP 120
Case 5: 85yo prior cardiac disease with one day of shortness of breath and indigestion. Borderline tachy, other vitals normal. Old the new ECG
Case 6: 85yo with one week of shortness of breath and cough. Normal vitals
Case 7: 25yo with three weeks progressive shortness of breath. Normal vitals
Case 8: 40yo with 2 hours of ongoing chest pain. Borderline tachy, other vitals normal.
Case 9: 75yo with one month of shortness of breath on exertion. Currently asymptomatic with normal vitals.
Case 10: 60yo with 2 weeks exertional chest pain. Painfree at rest, normal vitals. Old then new ECG:
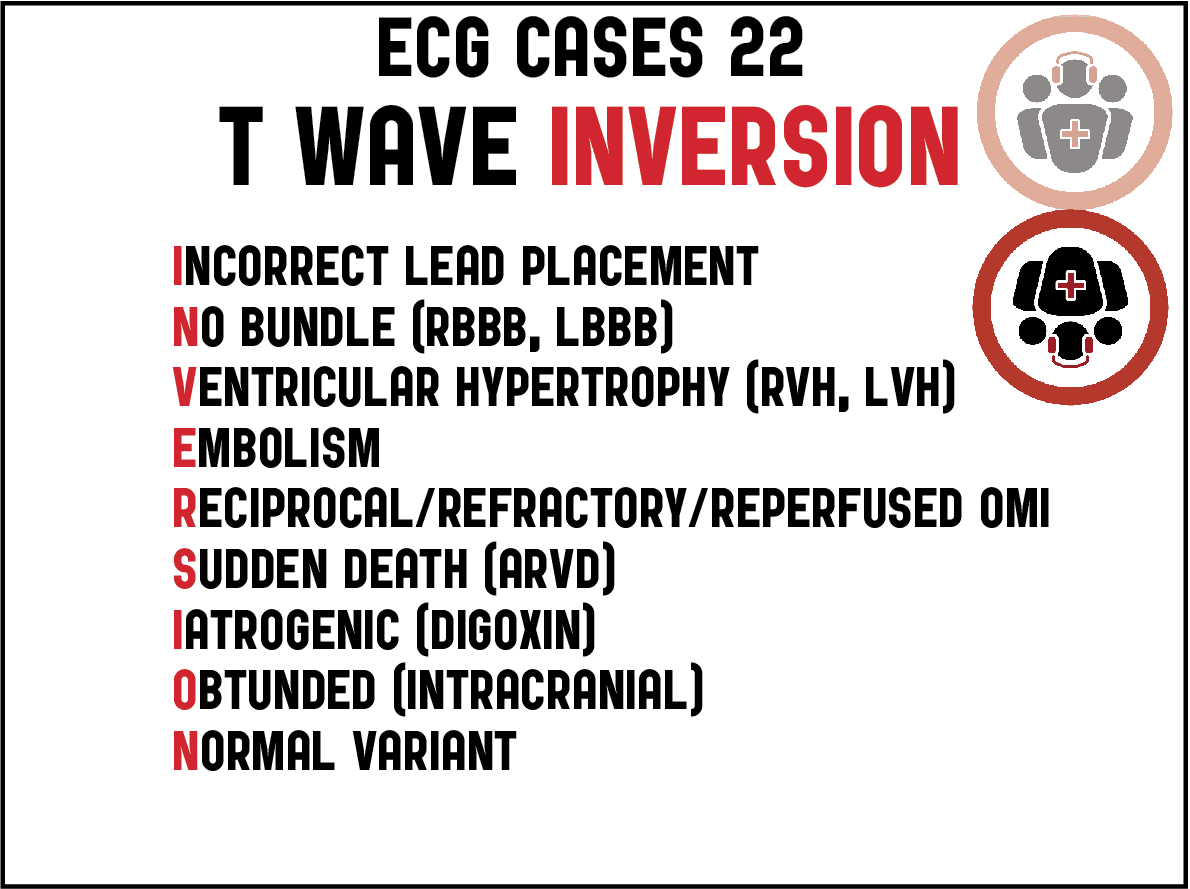
T-wave INVERSION
T-waves represent ventricular repolarization, and are normally inverted in leads aVR, V1 and sometimes III. In other leads, T-wave inversion (TWI) has a wide differential, as a review summarized: “Electrocardiographic TWIs may be related to a number of clinical syndromes, ranging from life-threatening events such as acute coronary ischemia, pulmonary embolism, and CNS injury to entirely benign presentations such as persistent juvenile T-wave pattern and the digitalis effect.”[1] The approach and differential to T-wave inversion can be remembered by the mnemonic “INVERSION”:
- Error
- Incorrect lead placement
- Secondary
- No bundle: LBBB, RBBB
- Ventricular hypertrophy: RVH, LVH
- Primary cardiovascular
- Embolism
- Reciprocal/reperfused/refractory Occlusion MI
- Miscellanneous
- Sudden death: ARVD
- Iatrogenic: digoxin
- Obtunded: ICP
- Benign
- Normal variant: persistent juvenile T-wave pattern
The first consideration is incorrect lead placement. Reversing limb leads can result in abnormal axis and inverted P-QRS-T-waves[1]. Precordial lead misplacement, with V1-2 placed too high, can also result in TWI. As a review summarized, “these features may falsely suggest acute or old cardiac ischemia, pulmonary embolism, or a type-2 Brugada pattern. Upwards misplacement of the lead may be strongly suspected with the P wave in V2 is biphasic, and presumed when the P wave is fully negative.”[2]
The next consideration is whether the TWI is secondary to abnormal depolarization. LBBB and LVH produce discordant ST depression and TWI in the left-sided leads, while RBBB and RVH produce discordant ST depression and TWI in right-sided leads. If there is superimposed ischemia, this can produce concordant ST elevation and upright T-waves, or disproportionate ST depression and deeper TWI.
If conduction is normal, then TWI is a primary abnormality. The most important consideration is Occlusion MI, which can manifest TWI as reciprocal changes, refractory ischemia, or reperfusion (spontaneous or after treatment). Wellens syndrome represents anterior TWI from spontaneously reperfused LAD occlusion at risk of re-occlusion (i.e. a patient with resolved symptoms, no Q waves, and TWI that progress from biphasic to symmetrically inverted), but this phenomenon can occur with any coronary artery. Refractory ischemia, on the other hand, presents with ongoing symptoms, Q waves and TWI. As an article explained, “TWI before reperfusion therapy must be interpreted in the context of time from onset of symptoms. Early TWI may suggest spontaneous reperfusion while evolution of ECG changes and late TWI signify more advanced stages of infarction.”[3] Anterior TWI can also be from pulmonary embolism, with concomitant inferior TWI which distinguishes it from cardiac ischemia. [4]
The differential for TWI also includes miscellaneous rarer causes—including arrhythmogenic right ventricular dysplasia (anterior TWI and epsilon waves), digoxin effect (diffuse sagging ST depression with flat or inverted T-waves), or intracranial emergencies (eg SAH, with deep TWI and prolonged QT). A final consideration for anterior TWI is the normal variant of “persisting juvenile T-wave pattern,” with shallow and asymmetric anterior TWI in young healthy adults (similar to the pattern seen in children). But this should be a diagnosis of exclusion, as a review summarized, “A diagnosis of PJTWP should be made only after consideration of more dangerous causes of anterior TWI, because such changes could reflect severe chronic obstructive pulmonary disease, pulmonary embolism(PE), acute myocardial infarction, or pulmonary hypertension. In particular, especially in the context of syncope, the clinician should consider the possibility of dysrhythmogenic right ventricular cardiomyopathy, as it may often present with TWI in V1–V3 in patients > 14 years old.”[5]
Back to the cases
Case 1: V2 TWI from lead misplacement
- Heart rate/rhythm: normal sinus
- Electrical conduction: normal
- Axis: normal
- R-wave: normal progression
- Tension: no hypertrophy
- ST/T: V2 TWI concordant with inverted P/QRS from high lead placement
Impression: lead misplacement. Normal ECG after V1-2 correctly placed (below) and patient had negative workup.
Case 2: inferior TWI from lead misplacement
- H: inverted P wave in II
- E: normal conduction
- A: extreme axis deviation
- R: old Q in V2 and small R in V3, pseudoQ wave inferiorly
- T: no hypertrophy
- S: inferior TWI concordant with inverted P/QRS
Impression: limb lead reversal. Patient had cath lab activated (with no culprit lesions) because of apparent inferior Q, convex ST segment and TWI, but this was from lead misplacement. Repeat ECG was back to baseline after correct placement:
Case 3: lateral TWI secondary to LBBB
- H: borderline sinus tach
- E: LBBB
- A: left axis
- R: poor R wave progression from LBBB
- T: can’t assess LVH
- S: lateral discordant TWI, no concordant or excessively discordant ST changes
Impression: LBBB without Sgarbossa/Smith criteria in hemodynamically stable patient. Unnecessary cath lab activation, negative workup.
Case 4: anterior TWI from RBBB + refractory Occlusion MI
- H: junctional bradycardia
- E: RBBB + LAFB
- A: left axis from LAFB
- R: early R wave from RBBB + anterior Q
- T: no hypertrophy
- S: mild concordant anterior STE with deep TWI
Impression: junctional bradycardia, bifasicular block and anterior Q+STE+TWI from refractory LAD occlusion. Initially interpreted as simply RBBB until trop I came back at 50,000, then cardiology consulted. Cath: 100% mid LAD occlusion, developed complete heart block requiring pacemaker.
Case 5: lateral TWI from LVH + reciprocal to Occlusion MI
- H: sinus tach
- E: normal intervals
- A: normal axis
- R: loss of anterior R waves
- T: LVH
- S: lateral TWI are deeper and more symmetric than baseline
Impression: LVH with loss of anterior R wave and reciprocal lateral TWI. Cath lab activated: 95% mid LAD occlusion, trop I rise from 1500 to 9000. Discharge ECG had anterior reperfusion TWI and return to baseline lateral TWI
Case 6: anterior TWI secondary to RVH
- H: sinus arrhythmia
- E: normal intervals
- A: right axis
- R: early R wave
- T: RVH (early R wave + right axis)
- S: anterior TWI discordant to abnormally tall T-wave
Impression: anterior TWI secondary to RVH, in patient with pulmonary hypertension who presented with respiratory infection.
Case 7: anterior/inferior TWI from pulmonary embolism
- H: normal sinus
- E: normal conduction
- A: normal axis
- R: normal R wave
- T: no hypertrophy
- S: TWI anterior + III
Impression: anterior and inferior TWI with progressive shortness of breath, consistent with PE. Trop I was 800 and CT revealed bilateral PE with RV strain.
Case 8: lateral TWI reciprocal to inferior Occlusion MI
- H: sinus tach
- E: normal intervals
- A: normal axis
- R: normal R wave progression, inferior Q
- T: no hypertrophy
- S: concave STE in III only, but reciprocal STD/TWI in I/aVL and STD in V2
Impression: infero-posterior Occlusion MI. Cath lab activated: 100% RCA occlusion, first trop I was 100 and peak 15,000. Discharge ECG had inferior Q with reperfusion TWI, and normalization of reciprocal TWI and anterior STD:
Case 9: anterolateral TWI from reperfused LAD occlusion
- H: sinus
- E: LAFB
- A: left axis from LAFB
- R: normal R waves, no Q waves
- T: no hypertrophy
- S: anterolateral TWI
Impression: resolved exertional symptoms with reperfusion TWI in LAD territory (Wellens syndrome). Trop neg but treated as acute coronary syndrome and admitted for angiogram: 85% proximal LAD occlusion. Discharge ECG had progression of anterolateral reperfusion TWI, then follow up ECG had TWI resolution:
Case 10: inferior TWI from reperfused RCA occlusion
- H: normal sinus
- E: normal conduction
- A: physiological left axis
- R: new tall R wave in V2
- T: no hypertrophy
- S: TWI in III/aVF
Impression: reperfused infero-posterior Occlusion MI. First trop I was 115 and admitted as “NSTEMI”. Cath few days later: 95% RCA occlusion. Discharge ECG same inferior TWI and tall anterior R wave:
Take home points for T-wave INVERSION mnemonic
- The differential for T-wave INVERSION includes: Incorrect lead placement, No bundle (RBBB, LBBB), Ventricular hypertrophy (LVH, RVH), Embolism, Reciprocal/refractory/reperfused occlusion MI, Sudden death (ARVD), Iatrogenic (digoxin), Obtunded (eg SAH), and Normal variant
- Acute cardiovascular TWI include reciprocal changes, reperfused occlusion (resolved symptoms), refractory ischemia (prolonged symptoms + Q waves), secondary + primary TWI (eg RBBB or LVH with disproportionate TWI), and PE (anterior + inferior TWI)
References for ECG Cases 22: T-wave INVERSION mnemonic
- Mond HG, Garcia J, Visagathilagar. Twisted leads: the footprints of malpositioned electrocardiographic leads. Heart Lung and Circ 2016 Jan;25(1):61-7
- Walsh B. Misplacing V1 and V2 can have clinical consequences. Am J of Emerg Med 2018 May;36(5):865-870
- Hira et al. T-wave inversions in leads with ST elevations in patients with acute anterior st elevation myocardial infarction is associated with patency of the infarct related artery. J Electrocardio Jul-Aug 2014;47(4):472-7
- Kosuge M, Kimura K, Ishikawa T, et al. Electrocardiographic Differentiation Between Acute Pulmonary Embolism and Acute Coronary Syndromes on the Basis of Negative T-Waves. Am J Cardiol 2007 Mar 15;99(6):817-21
- Walsh B, Smith SW. ‘Persistent juvenile’ T-wave pattern may not be persistent: case series and literature review. J Emerg Med 2015 Dec;49(6):e165-72

























Leave A Comment