Topics in this EM Quick Hits podcast
Justin Morgenstern on watchful waiting for large spontaneous pneumothoraces (0:44)
Michelle Klaiman on mirco-dosing buprenorphine for opiate use disorder (5:17)
Arun Sayal on the practical application of CRITOE in pediatric elbow fractures (10:45)
Jeff Perry on The Canadian TIA Score (19:37)
Sarah Reid on updated pediatric surviving sepsis guidelines (25:59)
Salim Rezaie (Best of REBELEM) on safety of vasopressor administration through peripheral IVs (33:40)
Podcast production, editing and sound design by Anton Helman
Podcast content, written summary & blog post by Michelle Klaiman and Anton Helman
Cite this podcast as: Helman, A. Morgenstern, J. Klaiman, M. Sayal, A. Perry, J, Reid, S. Rezaie, S. EM Quick Hits 18 – Conservative Management Pneumothorax, Microdosing Buprenorphine, Practical Use of CRITOE, Canadian TIA Score, Pediatric Surviving Sepsis Guidelines, Safety of Peripheral Vasopressors. Emergency Medicine Cases. May, 2020. https://emergencymedicinecases.com/em-quick-hits-may-2020/. Accessed [date].
Watchful waiting of large spontaneous pneumothorax
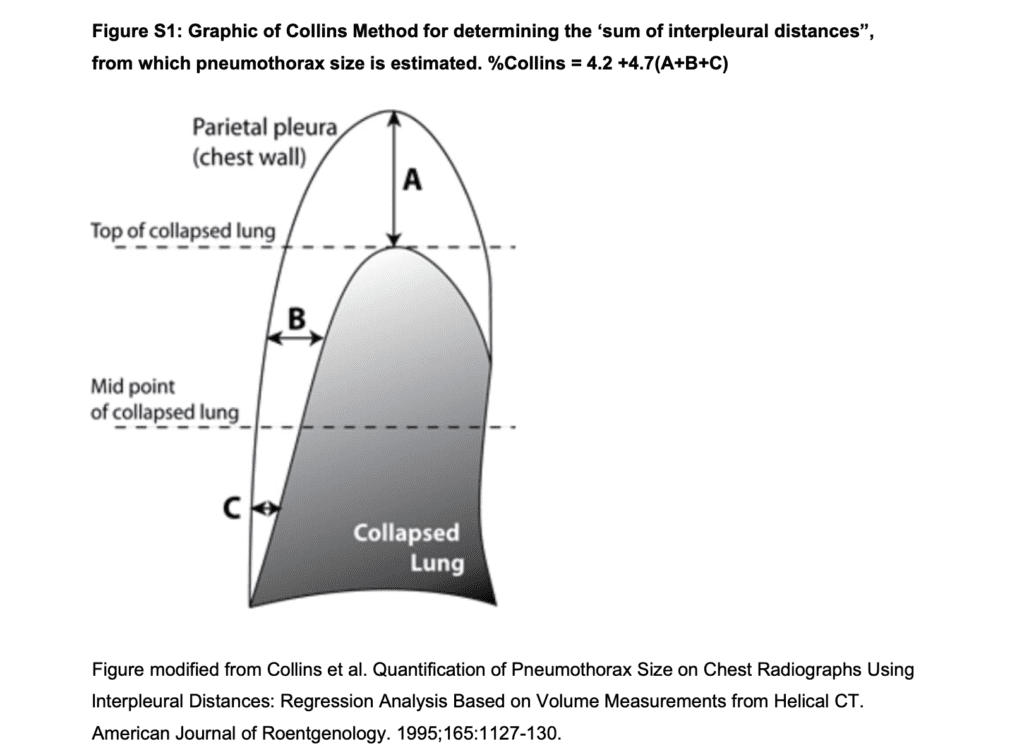
- This multicenter, open label, non-inferiority trial of 316 patients compared small bore chest tube treatment for primary spontaneous pneumothorax >32% (using Collins method – see below) to conservative management (observation for 4 hours followed by repeat chest x-ray and discharge from the ED if walking comfortably and vital signs were stable)
- The primary outcome of complete radiologic resolution of the pneumothorax occurred in 98.5% of the intervention group at 8 weeks and 94.4% of the conservative management group, a “non-inferior” difference and complete resolution of symptoms at 8 weeks was similar ( 93.4% vs 94.6%)
- Secondary outcomes show that pneumothoraces took about 2 weeks longer to resolve in the conservative group, however they had shorter hospital stays, less time of work, less CT scans, less recurrence and less serious adverse events
- Consider including conservative management of spontaneous pneumothorax in shared decision making
The Collins method estimates the size of pneumothorax using a calculation based on measuring the interpleural distance at the apex (A) and the midpoints of the upper (B) and lower (C) halves of the collapsed lung to the hemithorax on a PA chest x-ray.
- Brown SGA, Ball EL, Perrin K, et al. Conservative versus Interventional Treatment for Spontaneous Pneumothorax. The New England journal of medicine. 2020; 382(5):405-415
- First10EM: Conservative treatment for pneumothorax
- St Emlyn’s JC: Conservative management of pneumothoraces.
- REBEL EM: Spontaneous Pneumothorax: Stand There and Do Nothing?
ED buprenorphine initiation and microdosing
- ED initiation of buprenorphine/naloxone is standard of care for opioid withdrawal
- Opioid agonist therapy, including buprenorphine/naloxone, is the only evidence-based treatment for opioid use disorder to reduce opioid overdose death and ED visits
- Buprenorphine/naloxone is a safe medication with a ceiling effect for respiratory depression, although this is attenuated by concurrent sedating agents such as alcohol or benzodiazepines.
- If given too early, buprenorphine/naloxone can precipitate withdrawal as it displaces full agonists and downregulates mu opioid receptors.
- If a patient is not yet in withdrawal, consider a home initiation with 6 X 2mg tablets or a microdosing protocol.
Buprenorpine microdosing protocols
- Hammig R, Kemter A, Strasser J, von Bardeleben U, Gugger B, Walter M, et al. Use of microdoses for induction of buprenorphine treatment with overlapping full opioid agonist use: the Bernese method. Substance abuse and rehabilitation. 2016;7:99-105.
- Hu, Tina; Snider-Adler, Melissa; Nijmeh, Larry; Pyle, Adam. Buprenorphine/naloxone induction in a Canadian emergency department with rapid access to community-based addictions providers. CJEM ; 21(4): 492-498, 2019 Jul.
- Klaire S, Zivanovic R, Barbic SP, Sandhu R, Mathew N, Azar P. Rapid micro-induction of buprenorphine/naloxone for opioid use disorder in an inpatient setting: A case series. The American journal on addictions. 2019.
Using CRITOE sensibly for pediatric elbow fractures: Lateral condyle and medial epicondyle fractures
- Lateral condyle fractures comprise 15% of pediatric elbow fractures, are commonly missed in the ED and may require surgery; they are typically seen in children 3-8 years of age.
- A subtle lucency proximal to the capitellum on the elbow x-ray is either the ossification center “E” of CRITOE which closes at 10 years of age or in the 3-8 year old may represent a lateral condyle fracture, which if 1-2mm displaced, is often operative
- Medial epicondyle fractures comprise 10% of pediatric elbow fractures and are commonly missed in the ED; the mechanism is usually a valgus strain, typically in a 12-16 year old child; up to 5-10mm displacement is acceptable
- If the “I” of “CRITOE” is is difficult to identify, but “TOE” are present, suspect a medial epicondyle fracture that has migrated into the elbow joint
- When in doubt order a contralateral elbow x-ray for comparison
Medial epicondyle fracture. Case courtesy of Dr Andrew Dixon, Radiopaedia.org, rID: 9450
Marx, John A., and Peter Rosen. Rosen’s Emergency Medicine: Concepts and Clinical Practice. 8th ed. Philadelphia, PA: Elsevier/Saunders, 2014.
The Canadian TIA Score

A risk stratification tool that estimates of the risk that a patient presenting to the ED with TIA will suffer a stroke within 7 days. -3 to 3 points = low risk, 4-8 points = medium risk, ≥9 points = high risk.
- The Canadian TIA Score stratifies risk of subsequent stroke into low, moderate and high risk.
- Prompt emergency carotid endarterectomy (CEA) to prevent stroke has a NNT = 3 in high risk patients.
- Primary outcome was the composite of subsequent stroke or CEA ≤7 days.
- Prospectively enrolled 7,569 patients of whom 107 (1.4%) had a subsequent stroke and 74 (1.0%) CEA ≤7 days
- The Canadian TIA Score stratified the stroke/CEA ≤7days risk as: Low probability <0.2%, moderate probability 1.3%, high probability 2.6%.
- Inclusion Criteria
-
- Age > 18
- Diagnosed with a TIA in the ED by either the ED physician or neurologist
- Exclusion Criteria
-
- Patients who were diagnosed with a confirmed stroke (neurological deficit present >24 hours)
- Decreased LOC (GCS <15)
- Documented other cause for deficit which was not a TIA
- Presented >7 days following onset of most recent TIA and treated with TPA for an acute stroke.
- The Canadian TIA Score seems to accurately identify TIA patients risk for stroke/CEA ≤7 days.
- Suggested care recommendations based on Canadian TIA Score (-3 to 3 points = low risk, 4-8 points = medium risk, ≥9 points = high risk)
- Low risk – safely discharge following a careful ED assessment with elective follow-up
- Moderate risk – undergo additional testing in the ED, have antithrombotic therapy optimized, and be offered early stroke specialist follow-up
- High risk – fully investigate and manage ideally in consultation with a stroke specialist during their index ED visit
Ottawa Rules app on Google Play
Perry, J. et al. A prospective cohort study of patients with transient ischemic attack to identify high-risk clinical characteristics. Stroke. 2014 Jan;45(1):92-100. doi: 10.1161/STROKEAHA.113.003085. Epub 2013 Nov 21.
Perry, J. et al. PL01: Prospective multicenter validation of the Canadian TIA Score for predicting subsequent stroke within seven days. CJEM, 21(S1), S5-S5. 2019. doi:10.1017/cem.2019.40
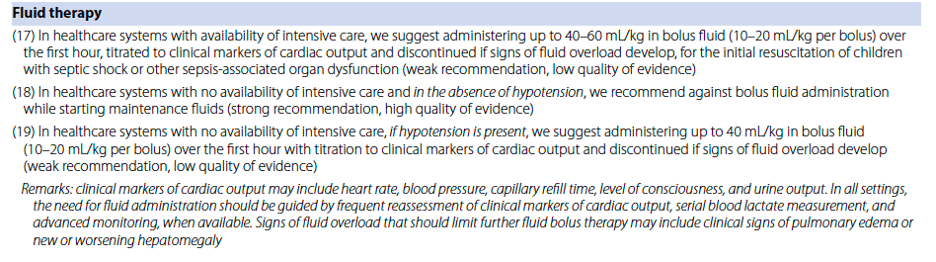
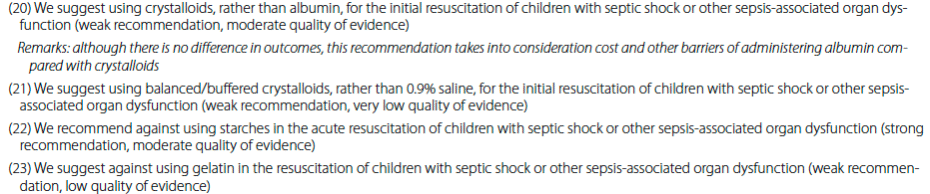
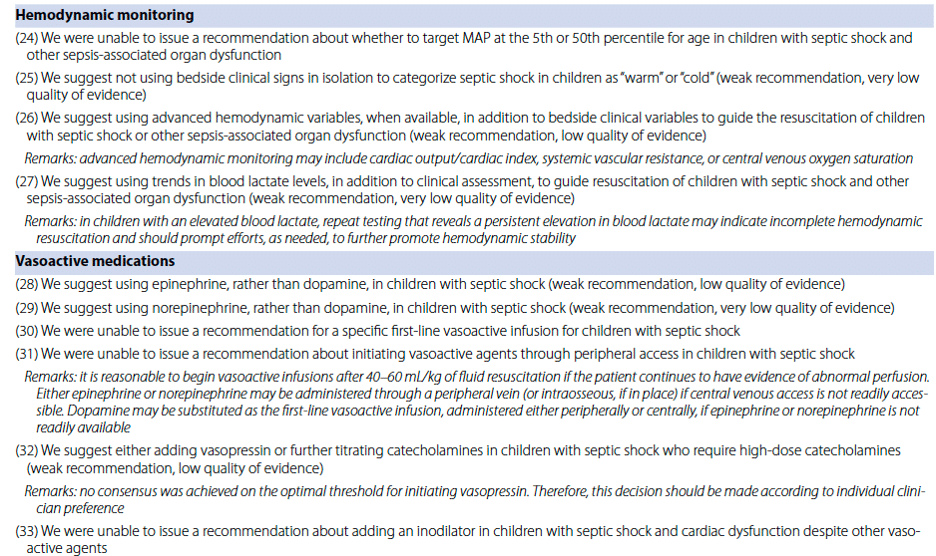
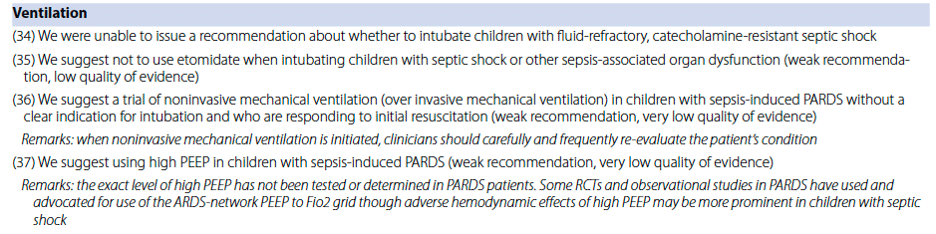
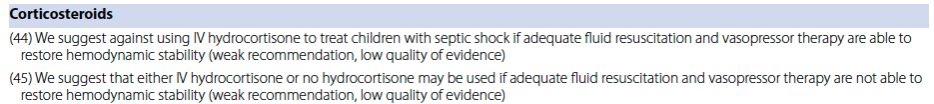
Pediatric sepsis updated guidelines 2020 bottom line recomendations
Episode 50 Recognition and Management of Pediatric Sepsis and Septic Shock
Weiss SL, Peters MJ, Alhazzani W, et al. Surviving Sepsis Campaign International Guidelines for the Management of Septic Shock and Sepsis-Associated Organ Dysfunction in Children. Pediatr Crit Care Med. 2020;21(2):e52-e106.
Safety of peripheral IV vasopressors and managing their complications (Best of REBEL EM)
In the latest systematic review on this topic the extravasation rate was about 3%, and the rate of limb ischemia and compartment syndrome was 0%.
If you are faced with an extravasation event:
- Leave the catheter in place
- Slowly aspirate as much of the drug as possible
- Administer phentolamine 0.1-0.2mg/kg (max 10mg) through the IV plus 5mg/ml mixed in 9mL NS subcutaneous AND a 1 inch strip of topical nitroglycerine 2% to the site of ischemia
- Remove catheter
- Elevate the affected limb to minimize swelling
- Apply warm compressess for 20 mins q6-8h for at least 24-48hrs
In patients who are critically ill and requiring vasopressor treatment, the use of peripheral IVs are relatively safe with several caveats:
- Use an antecubital fossa or more proximal IV (These are generally larger veins which allow for larger IVs (i.e. 18g)
- Do not run the infusion for >2 – 4hrs
- Use as dilute a concentration as possible
- Use as small a volume as possible
- Have an IV observation protocol
- Have an extravasation protocol
REBEL Cast Ep73 – Are Peripheral Vasopressors Safe?
- Tian DH et al. Safety of Peripheral Administration of Vasopressor Medications: A Systematic Review. EMA 2019.
- Pancaro C et al. Risk of Major Complications After Perioperative Norepinephrine Infusion Through Peripheral Intravenous Lines in a Multicenter Study. Anesth Analg 2019.
None of the authors have any conflicts of interest to declare




Great post as always Anton and all the wonderful contributors!
It’s great to know that peripheral vasopressors can be run safely in the ED. My one argument for putting in the central line in the ED is that if we never end up doing the procedure or do so infrequently, we will become deskilled and inefficient at it. I know with IOs around, central lines are rarely needed in the initial resuscitation but it’s a great skill to have in the back of your pocket and one we leave residency being comfortable with. I think if you have the extra 10-15 minutes, and the patient is going to ultimately need the central line, it’s always nice to put in the line yourself and refresh that skill :)
Hey Anton
What scores on the TIA score puts a patient in low, medium or High. Thanks!
Just updated the post to include low/medium/high risk categories, taken from the the Ottawa Rules App itself. I suggest downloading the app – makes it nice and easy on shift.