In Part 2 of this Episode on Emergency Ultrasound or Point of Care Ultrasound (POCUS) Dr. Fischer, Dr. Hannam, Dr. Chenkin & Dr. Hall, Canada’s EM ultrasound gurus discuss how POCUS can help our decision-making in the pediatric patient with a limp, in the patient with necrotizing fasciitis, in the pregnant patient with vaginal bleeding and in the common and challenging elderly patient with undifferentiated abdominal pain. They cover POCUS indications from urinary retention to appendicitis and debate the utility of these indications. This is followed by a debate on how best to educate ourselves and the EM community in POCUS and how best to designs quality assurance programs so that point of care ultrasound (POCUS) becomes an accepted tool across the entire medical community.
Our panel of POCUS experts answer questions such as: How does emergency ultrasound compare to X-ray to identify soft-tissue foreign bodies? How does the accuracy of emergency ultrasound compared to radiology department ultrasound for cholycystitis? Can emergency ultrasound help us in the the patient with suspected appendicitis? Can emergency ultrasound replace foley catheterization to assess for urinary retention in the patient with suspected cauda equina syndrome? What are the common pitfalls of the FAST exam and the AAA ultrasound exam? and many many more….
Cite this podcast as: Hall, G, Chenkin, J, Hannam, P, Fischer, J, Helman, A. Part 2: More Point of Care Ultrasound. Emergency Medicine Cases. November, 2011. https://emergencymedicinecases.com/episode-18-part-2-more-point-of-care-ultrasound/. Accessed [date].
POCUS for Soft Tissue Infection
Ultrasonographic appearance may help in diagnosis and treatment of diseases along a spectrum:
- Cellulitis: edematous tissues with cobblestone appearance (see image)
- Abscess: physicians have been shown in studies to be poor at identifying the presence of an abscess in patients with cellulitis clinically, leading to many unnecesarry I&Ds; on POCUS , abscess appears as a hypoechoic collection; POCUS may be used to define borders and depth (eg, peritonsillar abscess with carotid artery nearby), or post‐procedure to insure all septations have been broken and loculations drained
- Foreign bodies (FBs): POCUS better than XR for many FBs (plastic, wood); however, for very small FB, no better than XR; POCUS may help in localising FB, injecting lidocaine around it, and removing it in real‐time visualization
- Necrotizing fasciitis: fascial thickening, turbid fluid accumulation near fascial plane, and lots of soft tissue swelling; also edema out of proportion compared to what is seen clinically
- Periosteal abscess: fluid beneath bone cortex
POCUS for Vaginal Bleeding
In order to reasonably exclude ectopic pregnancy (in the absence of traditional risk factors):
- Need to visualize whole uterus, from cervix from fundus, with juxtaposition with the bladder and in two planes (transverse and longitudinal),
- Criteria for definite IUP (intra‐uterine pregnancy): gestational sac ≥25mm (pseudo‐gestational sac of ectopic pregnancy is usually smaller), surrounded by ≥5‐7mm of uterine tissue, with white ring within it (i.e. yolk sac); if you see fetus, look for heart beat (see image – note: no bladder seen)
- In all scans, Morrison’s pouch should be imaged to rule out free fluid – even when positive intra‐uterine pregnancy (patient may have heterotopic pregnancies, which might be as frequent as 1:6‐8,000 compared to the usually quoted 1:30,000), and even in β‐HCG level below usual cut off as it may be low secondary as the ectopic pregnancy dying, which can still rupture as a result of the inflammatory response
- Discriminatory thresholds of ultrasound for IUP: 5wks (usually β‐HCG of 1,500) – gestational sac; 5.5wks – gestational with yolk sac; 6wks – fetal pole; 6‐7wks – fetal heart
Pitfalls:
- (1) not full visualization of the uterus due to bowel gas
- (2) not asking questions about risk factors of ectopic pregnancy
- (3) not realizing that fertility treatments = heterotopic pregnancy more likely
- (4) indeterminate scan is still an ectopic pregnancy until proven otherwise, and should be treated as such with immediate confirmatory scan
- Importantly, bedside ultrasound cannot be used as a tool to confirm the well‐being of the fetus in the 2nd or 3rd trimester, given that conditions such as placenta previa and placenta abruptio may present with a normal POCUS
Check out the PV Card on ALiEM for a summary of how to do POCUS for 1st trimester vaginal bleeding.
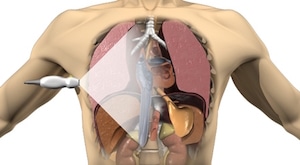
FAST exam
- Part of primary survey for multi‐trauma patient: RUQ or Morrison’s pouch – most dependent portion of abdomen and therefore most likely to collect blood, LUQ – both splenorenal and subdiaphragmatic space (the latter is more dependent), pelvis – retrovesicular space in men or Douglas space in women, and pericardial space; extended FAST (eFAST) is part of secondary survey: scan thorax for pneumo/hemothoraces
- Algorithm
- Unstable patient and positive FAST – straight to OR
- Hemodynamically stable patient with positive FAST – likely to CT scan to further delineate injuries
- Negative FAST – CT scan if mechanism of injury is severe, but may elect observation with serial clinical and FAST exams
- Limitations: FAST is operator‐dependent, and it cannot differentiate between acute blood from chronic ascites, the location of the bleeding, or injuries to solid organs; will miss hollow viscus injuries, or retroperitoneal injuries
- Pitfalls of FAST
- (1) performing FAST when patient needs laparotomy regardless of results
- (2) not repeating examination in negative study as the 250‐500cc of fluid necessary for positive result may take time to develop
- (3) believing a negative study in patients with prior laparotomy and loculations (fluid accumulates in non‐traditional locations), or
- (4) in patients with non‐acute injury (few hours later), due to clotted blood appearing as solid organ
POCUS for Abdominal Aortic Aneurysm
- Consider it in every patient >50yo with abdominal, flank or back pain, especially if history of HTN or smoking, and in patients with syncope
- Technique: transverse position starting at xyphoid and looking at the aorta subdiaphragmatically just anterior to the spine, which is thick‐walled and non‐compressible with no respiratory variability; go down until the bifurcation of the iliac vessels (see image – positive AAA scan with intraluminal clot)
- Aorta >3cm means aortic aneurysm, but gives no information re: rupture (which may be retroperitonally and without free fluid in abdomen), which should be a clinical diagnosis
- Bowel gas: press hard and hold the probe for up to 30sec until the gas moves and the aorta appears
Point of Care Ultrasound for Cholecystitis
- Sonographic Murphy’s sign: after visualizing the GB, press on it with the probe, positive test with pain maximal at this location (in the setting of stone) – highly specific for acute cholecystitis
- Other signs: distended GB, thickened GB wall (proximal wall in transverse view), pericholecystic fluid – none of these are perfect, but EPs shown to be as good as radiologists for diagnosing acute cholecystitis in studies
- See image for distended gallbladder, thickened wall and pericholecystic fluid
Urinary retention & Post-void Residual
- Bladder is elastic and assumes different shapes, so measurement of urine post‐void residual can be off by as much as 20%, so consider using Foley (the gold standard) instead for accurate measurement (eg, in the case of rule out cauda equina a post‐void residual of
- Ultrasound may be sufficient to determine post‐void residual if the urine volume seen is extreme (very large or the bladder is empty or near‐empty), and therefore may obviate the need for a foley.
Point of Care Ultrasound for Emergency Procedures
- Ultrasound‐guided central line vascular access has been shown to be safer, identify anatomical variations (eg, 5% of internal jugular veins are medial to carotid artery), to decrease complications, to reduce the number of attempts and the number of failed attempts, and to decrease the time for procedure
- US can be used in static or dynamic (better) technique, or alone or 2‐operator technique; can also help in rotating the patient’s neck just the right amount to separate the internal jugular as much as possible from the carotid artery; can also be used to confirm position of central line after insertion
- Especially helpful with trainees and education, to demonstrate exactly what is happening and give real‐time feedback
- Consider utrasound‐guided supra‐clavicular approach as an alternative to subclavian approach (which needs to be blind given that bone obscures view, and traditionally has had the lowest complication rate of all blind central line locations)
Point of Care Ultrasound for Nerve blocks
- High‐doses narcotics can cause complications (respiratory failure, delirium) especially in elderly, which can often be avoided easily by nerve blocks
- 3‐in‐1 nerve block for hip fractures: femoral, lateral femoral cutaneous, and obturator nerves are blocked; faster relief of pain for patient and lower dose of anesthetic used (20cc vs. 30cc) when POCUS is used (compared to blind technique), and lower use of opiods for same pain relief
Education, certification and quality assurance
- The EM Cases experts agree that POCUS needs to be part of the core curriculum for the training of new emergency physicians, who then might not require formal certification given that POCUS is a skill on the same level as ECG‐reading or intubation; however, it is not clear how the evaluation of the skill should proceed, i.e. competency assessment vs. a set number of procedures done
- However, for the emergency physicians in practice, there needs to be a mechanism to bring them up to speed and insure that quality of care and patient safety is not compromised, either through continuing medical education or certification (similar to when laparoscopic surgeries started and surgeons needed re‐training)
More Point of Care Ultrasound Pearls
- For pediatric head injury where you are debating whether or not to do a CT scan of the brain, consider assessing for skull fracture with ultrasound, because intracranial bleeding is much more likely in the setting of skull fracture, and if found would then necessitate a CT scan (see EMC episode 3 for details on pediatric head injuries)
- Emergency US for appendicitis is only part of the diagnostic puzzle, but given that high specificity demonstrated in studies (which is what surgeons care about to decrease ‘white laparotomies’), it is a useful skill
For more on Point of Care Ultrasound on EM Cases:
Episode 18 Part 1: Point of Care Ultrasound Pearls, Pitfalls and Controversies
Best Case Ever 6 Can Point of Care Ultrasound Save Lives?
POCUS Cases videos




Very nice introduction to arrays of POCUS application.