This past May in Toronto, the largest and, in my opinion, best Canadian EM conference, North York General Hospital’s Emergency Medicine Update Conference, attracted ‘Captain Cortex’ himself, Stuart Swadron, a Toronto native to talk about his approach to vertigo, which highlights how not to miss a posterior circulation stroke. For the seventh year running the EMU conference was proud to have one of the worlds most well known EM educators, Amal Mattu who presented the most important Cardiology Literature from the past year. This podcast includes edited versions of their talks with commentary and summaries.
Blogpost & Summary Prepared by Dr. Keerat Grewal, June 2014
Cite this podcast as: Swadron, S, Mattu, A, Helman, A. NYGH EM Update Conference 2014. Emergency Medicine Cases. June, 2014. https://emergencymedicinecases.com/episode-45-swadron-vertigo-mattu-cardiology-literature-em-update-2014/. Accessed [date].
Chapter 1 – Dr. Stuart Swadron – An Approach to Vertigo
From North York General’s Emergency Medicine Update Conference, May 2014
VIDEO LINK for HINTS exam: http://emcrit.org/misc/posterior-stroke-video/
Go here to see a video Scott Weingart explaining how to use an iphone to help interpret the Head Impulse Test for your HINTS exam.
Paucis Verbis: Acute vestibular syndrome and HINTS exam. Academic Life in Emergency Medicine
An excellent review of the HINTS exam by Andrew Petrosoniak on Boring EM
GET STUART SWADRON’S BEST CASE EVER
Update 2015: Should HINTS be used on all patients with vertigo in the ED? Check out this critical appraisal of the HINTS exam on SOCMOB.
Update 2020: A prospective double-blind randomized trial involving 200 patients demonstrated that dimenhydrinate and metoclopramide are equally effective in treating nausea and vertigo symptoms in the emergency department. Abstract
Update 2022: A systematic review including 5 RCTs with 296 patients found that vestibular suppressant medications (including antihistamines, phenothiazines, anticholinergics, benzodiazepines) had no effect on symptom resolution after 14 to 31 days (difference -0.03, 95% CI -0.53 to 0.47), and uncertain effect on symptom resolution at 24 hours, patient satisfaction, quality of life, ED return visits or adverse events. This review did find that canalith repositioning maneuvers may improve symptom resolution at 14-31 days when compared to vestibular suppressants (RR 0.63, 95%CI 0.52 to 0.78). Abstract
Chapter 2 – Dr. Amal Mattu – Cardiology Literature
From North York General’s Emergency Medicine Update Conference, May 2014
Dr. Amal Mattu’s screencast on Sgarbossa Criteria at Emergency ECG Video of the Week: Episode 114
GET AMAL MATTU’S BEST CASE EVER
Summary of Full Episode
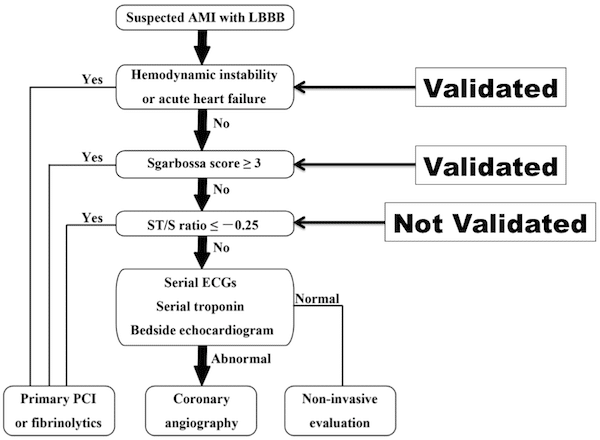
Fig 1: LBBB Algorithm (Cai et al., 2013) (4)
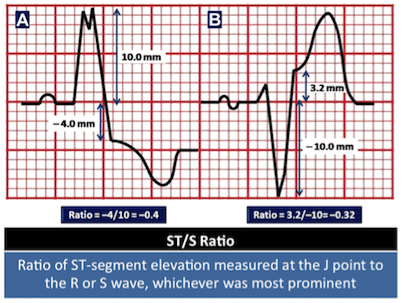
Fig 2: ST/S Ratio (Cai et al., 2014) (4)
Quote of the Month
“Everything should be made as simple as possible, but not simpler” – Albert Einstein
Dr. Helman, Dr. Mattu and Dr. Swadron have no conflicts of interest to declare.
KEY REFERENCES
1. Clinical practice guideline: Benign paroxysmal positional vertigo. Bhattacharyya, n et al. Otolaryngology-Head and Neck Surgery 2008; 139: 47-81. Abstract
2. Does my dizzy patient have a stroke? A systematic review of bedside diagnosis in acute vestibular syndrome. Tarnutzer, MD et al. CMAJ 2011; 183(9):571-592. Free Full Text
3. HINTS to diagnose stroke in the Acute Vestibular Syndrome: Three-step beside oculomotor examination more sensitive than early MRI diffusion-weighted imaging. Kattah, JC et al. Stroke 2009; 40: 3504-3510. Free Full Text
4. The left bundle-branch block puzzle in the 2013 ST-elevation myocardial infarction guideline: From falsely declaring emergency to denying reperfusion in a high risk population. Are the Sgarbossa Criteria ready for prime Time? Cai Q et al. American Heart Journal 2013; 166(3): 409-413. Free Full Text
5. 2013 ACCF/AHA Guideline for the management of ST-elevation myocardial infarction. O’Gara PT et al. Journal of the American College of Cardiology 2013; 61(4): 78-140. Free Full Text
6. Diagnostic time course, treatment, and in-hospital outcomes for patients with ST-segment elevation myocardial infarction presenting with nondiagnostic initial electrocardiogram. Riley RF et al. American Heart Journal 2013; 165(1): 50-56. Free Full Text
Click edit button to change this text.




Really great episode with two fantastic talks. I enjoyed hearing Stuart Swadron’s simplified approach to vertigo. One thing I wanted to point out, which may have been lost in the podcast (non-visual and edited) format, is that the HINTS battery of tests really must be applied to a specific patient population and only that population. The Acute Vestibular Syndrome is distinct from other vertigo, as described by Dr Newman-Toker in his CMAJ article in 2011:
“When dizziness de velops acutely, is accompanied by nausea or vomiting, unsteady gait, nystagmus and intolerance to head motion, and persists for a day or more, the clinical condition is known as acute vestibular syndrome.”
Thus the vertigo really must be persistent for several hours (and according to the above definition, > 24hr). Don’t apply HINTS to your brief vertiginous patients. Otherwise the tests don’t perform as they should, and for example, the ER doc may be over-calling the stroke due to the normal head thrust.
Great episode as usual.
Thanks Elisha for clarifying. BPPV is still the most common cause of vertigo that we see in the ED, and the HINTS exam does NOT apply to BPPV. It is specifically to help differentiate acute vestibular syndrome (which presents with constant vertigo for hours-days) vs stroke. If only the Dix-hallpike was as specific for BPPV as the HINTS is for stroke!
Great stuff