In this Part 2 of our two-part series on pericarditis and myocarditis, Anton is again joined by Dr. Walter Himmel and Dr. Paul Dorian. They answer such questions as: Why does myocarditis often present a diagnostic challenge? What are the range of ECG findings in myocarditis? Does a negative high sensitivity troponin or CRP rule out myocarditis? What is the role of PoCUS in the diagnosis and prognosis of myocarditis? When should we consider myocarditis or pericarditis in patients with recent COVID-19 infection or COVID mRNA vaccination, and which of these patients require workups? and more…
Podcast production, sound design & editing by Anton Helman
Written Summary and blog post by Kate Dillon, edited by Anton Helman March, 2022
Cite this podcast as: Helman, A. Episode 168 Myocarditis – A Diagnostic Challenge. Emergency Medicine Cases. March, 2022. https://emergencymedicinecases.com/myocarditis. Accessed [date]
Why does myocarditis often present a diagnostic challenge?
The reason that myocarditis presents a diagnostic challenge is that clinical findings are nonspecific and the breadth of presentations is wide, ranging from subclinical disease to fulminant heart failure, a variety of dysrhythmias and cardiogenic shock. The definitive diagnosis is made by cardiac MRI. It is important to remember that myocarditis is just one of the many cardiomyopathies that include dilated, hypertrophic and restrictive cardiomyopathies.
The many presentations of acute myocarditis:
- ACS-like or pleuritic chest pain (from associated pericarditis)
- Unexplained new onset or worsening heart failure
- Unexplained dysrhythmia (palpitations, syncope)
- Unexplained cardiogenic shock
A European multicenter study found that the most common presenting symptoms of myocarditis were dyspnea (71.7%), non-specific chest pain (31.9%), dysrhythmic events (17.9%) and pericardial effusion or systolic separation of the pericardium (14.2%).
Consider myocarditis in:
- Patients presenting with signs or symptoms of viral illness or sepsis + cardiac symptoms
- Patients with new or worsening heart failure without risk factors for coronary artery disease
- Patients whose presentation is not quite fitting the typical presentations for dysrhythmias, heart failure, ACS or sepsis
Discriminating sepsis from early cardiogenic shock secondary to myocarditis is challenging during the early stages of workup and treatment, as myocarditis may present with features of both.
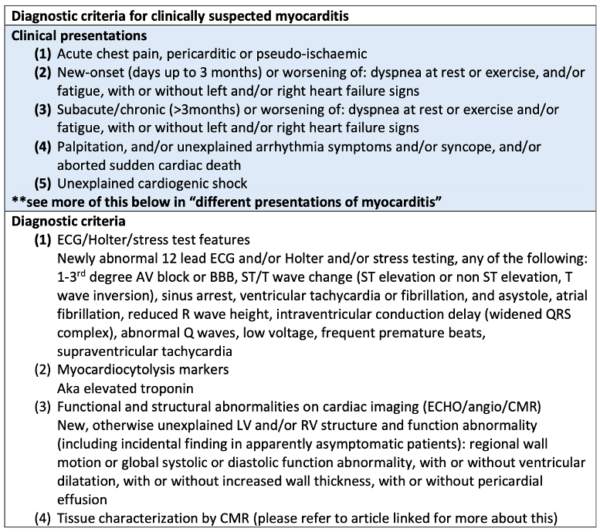
A preliminary diagnosis of myocarditis may be made if there is 1+ clinical presentation and 1+ diagnostic criteria from different categories (suspicion is higher with higher number of fulfilled criteria) in the absence of:
- Angiographically detectable CAD
- Known pre-existing cardiovascular disease or extra-cardiac causes that could explain the syndrome (valve disease, congenital heart disease, etc.).
Ancillary features supporting the diagnosis of myocarditis:
- Fever >38C at presentation or within the preceding 30 days with or without evidence of respiratory or GI infection
- Peripartum period
- Previous clinically suspected or definite myocarditis
- Personal or family history of allergic asthma, other types of allergies, or extracardiac autoimmune disease
- Family history of dilated cardiomyopathy (DCM) or myocarditis
In the subacute presentation of myocarditis patients may present with unexplained fatigue and dysrhythmias such as VPBs, non-sustained VT. Typically they are found to have mild LV dysfunction on cardiac ultrasound.
Etiologies of myocarditis – more than just viral etiologies
- Bacterial
- Toxic/Drugs:
- Amphetamines (especially cocaine)
- Ethanol
- Scorpion, snake, and spider bites
- Medications including checkpoint inhibitors, lithium, cyclophosphamide
Pearl: in patients with unexplained new onset third-degree heart block, Lyme carditis and sarcoidosis should be considered; an extreme first-degree heart block in a patient with recent tick exposure and/or unusual rash should be considered Lyme carditis until proven otherwise, and consideration should be given for admission on telemetry as many patients progress to third-degree heart block
Lyme carditis as a result of disseminated Lyme Disease from EMU 2017 with Leeor Sommer
There are a wide range of ECG findings in patients with myocarditis from normal to MI mimics to ventricular dysrhythmias
- ECG sensitivity for myocarditis is only 47%
- The presence of abnormal QRS complexes and new LBBB are findings that are associated with higher rates of death and heart transplant
Common ECG Findings of Myocarditis:
- Non-specific ST-segment or T-wave changes (most common finding)
- Sinus tachycardia
- Conduction abnormalities (prolonged/wide QRS)
- Atrial or ventricular tachy- brady-dysrhythmias (supraventricular or ventricular arrythmias occur in up to 55% of patients, often non-sustained and not causing hemodynamic compromise)
- Ventricular premature beats
- Overt ischemic changes (T-wave inversion, ST segment change, pathologic Q-waves, PR depression), can be seen in focal myocarditis which can mimic MI
- Diffuse PR depression with ST elevation (if pericardium is involved)
- Low voltages and/or electrical alternans (if pericardial effusion is present)
When to consider myocarditis or pericarditis in patients with recent COVID-19 infection or COVID mRNA vaccination
- The baseline prevalence of myocarditis in the general population in North America is approximately 200 cases/million people/year
- The prevalence of myocardial damage in patients hospitalized with COVID-19 is approximately 5-25%
- The risk of myocarditis from an mRNA COVID vaccine is approximately 2 cases/million vaccinations in all comers
- The peak incidence is ~5-15 days following vaccine
- If ECG and troponin are normal and the patient is minimally symptomatic, safe discharge from the ED should be considered
- The vast majority of these patients recover within a few days and require only symptomatic treatment
- A minority of these patients require longer hospital stays and/or supportive therapy
- In a very small number of cases worldwide patients required cardiac mechanical support
- The risk of vaccine induced myocarditis is higher in males 15-40 years old (50 cases/million vaccinations)
- The mortality rate in these cases is very low and recovery rate is high
- These cases are typically associated with mRNA vaccines and are more common after the second or third dose compared to the first dose
Bottom Line
-
- The COVID-19 mRNA vaccines portend a degree of protection against myocardial damage related to COVID-19 infection
- The risk benefit ratio is not as clear for young, healthy males 15-40 years, but our experts’ opinion is that the risk of long-term sequelae of long-COVID is much higher than the risk of long-term sequelae with vaccine associated myopericarditis
- One is more likely to sustain an injury from a lightning strike (1 in 211,166 in Canada) than to have major complications from COVID-19 mRNA vaccine related myocarditis
FOAMcast deep dive into data on myocarditis and COVID-19 vaccination
PoCUS helps determine severity and extent of disease in myocarditis but is seldom helpful in the diagnosis
- There are two key PoCUS findings to look for patients with myocarditis:
- Pericardial effusion (present in 25% of patients)
- Poor global LV function
- A normal PoCUS does not rule out myocarditis
- Abnormalities on PoCUS may help determine severity of cardiac dysfunction and extent of disease
Can a negative troponin rule out myocarditis? The role of bloodwork in the diagnosis of myocarditis
With almost everyone presenting to EDs either having contracted COVID-19 and/or having received COVID-19 vaccination, we are often presented with the conundrum of which patients who present to the ED with any of the symptoms of myocarditis require a workup for myocarditis. Working up every patient with even the slightest chest pain or shortness of breath or palpitations or fever or any concern for myocarditis would not only lead to droves of false positives and downstream harms but also grind the EDs to a halt and bankrupt the health care system! For patients with a low pretest probability a “watch and wait” approach is reasonable. For patients with a moderate pretest probability based on history, physical, ECG and PoCUS, is there a set of blood work that could rule out myocarditis? Unfortunately, there is not enough data to guide us here. The overall sensitivity of troponin for myocarditis is about 80%, however this includes subclinical myocarditis. CRP is usually elevated in myocarditis and correlates with the extent of myocardial damage as quantified by cardiac MR, however the sensitivity is poor. BNP levels are increased in some patients with acute perimyocarditis regardless of whether or not they have heart failure. If troponin, CRP and BNP are all negative it is very unlikely that clinically significant myocarditis is present but this cannot rule out the diagnosis. Clinical judgment should dictate which patients to work up for myocarditis.
Supportive therapies in the ED management of myocarditis
- ED management of myocarditis is supportive, including treatment of the complications of myocarditis (i.e. treat heart failure, shock, dysrhythmias as you normally would)
- Treatment is not with anti-inflammatories or colchicine as it is with pericarditis
- Patients with fulminant acute myocarditis require admission to an ICU and may require mechanical cardiac therapies such as ECMO
Episode 163: Acute Heart Failure ED Management: Part I
Episode 164: Cardiogenic Shock Simplified: Part II
Take home points on myocarditis
- Myocarditis presents a diagnostic challenge as clinical findings are nonspecific and the breadth of presentations is wide, ranging from subclinical disease to fulminant heart failure, a variety of dysrhythmias and cardiogenic shock
- Consider myocarditis in patients with atypical or unexplained cardiac and infectious symptoms, new or worsening heart failure or dysrhythmias without risk factors and in patients with unexplained cardiogenic shock
- Unexplained dysrhythmias and fatigue are a common presentation of patients who present in the subacute period
- There are a wide variety of ECG finding with myocarditis; a normal ECG does not rule out myocarditis and localized myocarditis can mimic MI
- The COVID-19 vaccines portent a degree of protection against myocardial damage as a complication of COVID-19 infection
- The risk of long term sequelae of COVID-19 are higher than the risk of long-term sequelae of vaccine associated myopericarditis
- In patients presenting 5-15 days after COVID-19 infection or COVID-19 vaccine, a normal ECG and troponin makes clinically relevant acute myocarditis unlikely and those patients can generally be discharged from the ED safely
- Troponin, BNP, and CRP should be considered in moderate pretest probability patients; if they are all negative the diagnosis of clinically significant acute myocarditis is very unlikely, but cannot be ruled out with certainty
- Treatment of myocarditis involves supportive management of the complications of myocarditis that may include heart failure, dysrhythmias and cardiogenic shock requiring ICU admission and cardiac mechanical therapy
References
- KociolRD, Cooper LT, Fang JC, et al; American Heart Association Heart Failure and Transplantation Committee of the Council on Clinical Cardiology. Recognition and Initial Management of Fulminant Myocarditis: A Scientific Statement from the American Heart Association. Circulation. 2020 Feb 11;141(6): e69-e92.
- Sharma AN, Stultz JR, Bellamkonda N, Amsterdam EA. Fulminant Myocarditis: Epidemiology, Pathogenesis, Diagnosis, and Management. Am J Cardiol. 2019;124(12):1954-1960.
- KindermannI, Barth C, Mahfoud F, et al. Update on myocarditis. J Am Coll Cardiol. 2012;59(9):779-792.
- Caforio AL, PankuweitS, Arbustini E, et al. Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J. 2013;34(33):2636-2648d.
- Ammirati E, Veronese G, Cipriani M, et al. Acute and Fulminant Myocarditis: A Pragmatic Clinical Approach to Diagnosis and Treatment. CurrCardiol Rep. 2018;20(11):114.
- Goitein, O., Sabag, A., Koperstein, R. et al. Role of C reactive protein in evaluating the extent of myocardial inflammation in acute myocarditis. J Cardiovasc Magn Reson 17, P291 (2015).
- Grabowski M, Karpiński G, J Filipiak K, Rdzanek A, Pietrasik A, Wretowski D, Rudowski R, Opolski G. Diagnostic value of BNP in suspected perimyocarditis–a preliminary report. Kardiol Pol. 2004 Nov;61(11):451-8; discussion 459-60.
- Cooper Jr, Leslie T. Myocarditis. N Engl J Med 2009; 360:1526–38.Hufnagel G, Pankuweit S, Richter A, Schönian U, Maisch B. The European Study of Epidemiology and Treatment of Cardiac Inflammatory Diseases (ESETCID). Herz. 2000;25(3):279-285.
- Blauwet LA, Cooper LT. Myocarditis. Progress in Cardiovascular Diseases. 2010;52(4):274-288.
- Riveros T. Myocarditis in Adults: ED Presentations, Evaluation, and Management. emDocs. Published October 2018. Accessed December 22, 2021.
- Handberg E, Apel G, Williamson K. Myocarditis in the ED. NUEM Blog, Peer-Reviewed. Published May 2016. Accessed December 22, 2021.
Drs. Helman, Dorian and Himmel have no conflicts of interest to declare
Now test your knowledge with a quiz.




Leave A Comment