Most Recent
WTBS 9 – EM Quality Assurance Part One: Improving Follow up from the ED
This is Waiting to Be Seen 9 on EM Cases - Improving Follow up From the ED, Quality Assurance Part 1. We all face the challenge of how to manage final reports that arrive after the patient has been admitted or discharged, but some EDs are more organized and diligent than others in systematically addressing their obligations in this area. In this two-part guest blog, Dr. Lucas Chartier, an emergency physician in Toronto, will discuss best practices in departmental organization in part one and the obligations of the individual physician in part two. No ED will ever be perfect, but there are some positive lessons to share and we likely all can do better in reducing risks related to test result follow-up.
BEEM Cases 3 – Acute Respiratory Failure: NIPPV & POCUS
Shortness of breath is a very common chief complaint in the emergency department, but despite our familiarity with this symptom, management is not always straightforward. The differential diagnosis is extensive, including the common cardiorespiratory conditions, but extending to toxicologic, hematologic, neuromuscular, metabolic, and psychiatric causes. Over the past decade, we have seen the widespread adoption of new technologies to help us manage these patients. This post will look at some new evidence on two of those technologies: noninvasive positive pressure ventilation (NIPPV) and ultrasound (POCUS). We will answer 3 questions based on 3 systematic reviews using the BEEM critical appraisal framework...
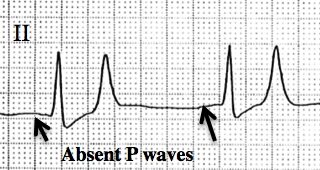
Best Case Ever 49 – Post-Arrest Hyperkalemia
Melanie Baimel's Best Case Ever on Post-Arrest Hyperkalemia on EM Cases. Post arrest patients can sometimes be challenging. We need to think of a variety of underlying causes of the arrest, antiarrhythmics, possible cath lab activation, targeted temperature management, sedation and more. To add to this, many post arrest patients do not have ideal vital signs that require attention. In this Best Case Ever, in anticipation of our upcoming episode on A Rational Approach to Hyperkalemia Dr. Melanie Baimel describes a post arrest patient who remains bradycardic and hypotensive despite multiple pressors....
Episode 85 – Medical Clearance of the Psychiatric Patient
Psychiatric chief complaints comprise about 6 or 7% of all ED visits, with the numbers of psychiatric patients we see increasing every year. The ED serves as both the lifeline and the gateway to psychiatric care for millions of patients suffering from acute behavioural or psychiatric emergencies. As ED docs, besides assessing the risk of suicide and homicide, one of the most important jobs we have is to determine whether the patient’s psychiatric or behavioral emergency is the result of an organic disease process, as opposed to a psychological one. There is no standard process for this. With the main objective in mind of picking up and appropriately managing organic disease while improving flow, decreasing cost and maintaining good relationships with our psychiatry colleagues, we have Dr. Howard Ovens, Dr. Brian Steinhart and Dr. Ian Dawe discuss this controversial topic...
CritCases 4 – Uterine Inversion and Postpartum Hemorrhage
In this CritCases blog - a collaboration between STARS Air Ambulance Service, Mike Betzner and EM Cases, Dr. James Brokenshire presents a case of acute unstable Uterine Inversion and discusses key therapeutic maneuvers including the Johnson Maneuver, tocolytics and resuscitation of postpartum hemorrhage.
Episode 84 – Congenital Heart Disease Emergencies
Congenital Heart Disease Emergencies on EM cases with Gary Joubert and Ashley Strobel. You might be surprised to learn that the prevalence of critical cardiac disease in infants is almost as high as the prevalence of infant sepsis. And if you’re like me, you don’t feel quite as confident managing sick infants with critical heart disease as you do managing sepsis. Critical congenital heart defects are often missed in the ED. For a variety of reasons, there are currently more children with congenital heart disease presenting to the ED than ever before and these numbers will continue to grow in the future. When I was in medical school I vaguely remember learning the complex physiology and long lists of congenital heart diseases, which I’ve now all but forgotten. What we really need to know about congenital heart disease emergencies is what actions to take in the ED when we have a cyanotic or shocky baby in front of us in the resuscitation room. So with the goal of learning a practical approach to congenital heart disease emergencies using the child’s age, colour and few simple tests, Dr. Strobel and Dr. Joubert will discuss some key actions, pearls and pitfalls so that the next time you’re faced with that crashing baby in the resuscitation room, you’ll know exactly what to do.