Most Recent
Funding FOAMed
Funding and freeing the future of learning that is FOAMed Longtime followers of EM Cases will have noticed a progressively prominent display on its website of the logo and inclusion of the name of [...]
Episode 64 Highlights from Whistler’s Update in EM Conference 2015 Part 2
In this Part 2 of EM Cases' Highlights from Whistler's Update in EM Conference 2015 Dr. David Carr gives you his top 5 pearls and pitfalls on ED antibiotic use including when patients with sinusitis really require antibiotics, when oral antibiotics can replace IV antibiotics, how we should be dosing Vancomycin in the ED, the newest antibiotic regimens for gonorrhea and the mortality benefit associated with antibiotic use in patients with upper GI bleeds. Dr. Chris Hicks gives you his take on immediate PCI in post-cardiac arrest patients with a presumed cardiac cause and The Modified HEART Score to safely discharge patients with low risk chest pain.
Episode 63 – Pediatric DKA
Pediatric DKA was identified as one of key diagnoses that we need to get better at managing in a massive national needs assessment conducted by the fine folks at TREKK – Translating Emergency Knowledge for Kids – one of EM Cases’ partners who’s mission is to improve the care of children in non-pediatric emergency departments across the country. You might be wondering - why was DKA singled out in this needs assessment? It turns out that kids who present to the ED in DKA without a known history of diabetes, can sometimes be tricky to diagnose, as they often present with vague symptoms. When a child does have a known history of diabetes, and the diagnosis of DKA is obvious, the challenge turns to managing severe, life-threatening DKA, so that we avoid the many potential complications of the DKA itself as well as the complications of treatment - cerebral edema being the big bad one. The approach to these patients has evolved over the years, even since I started practicing, from bolusing insulin and super aggressive fluid resuscitation to more gentle fluid management and delayed insulin drips, as examples. There are subtleties and controversies in the management of DKA when it comes to fluid management, correcting serum potassium and acidosis, preventing cerebral edema, as well as airway management for the really sick kids. In this episode we‘ll be asking our guest pediatric emergency medicine experts Dr. Sarah Reid, who you may remember from her powerhouse performance on our recent episodes on pediatric fever and sepsis, and Dr. Sarah Curtis, not only a pediatric emergency physician, but a prominent pediatric emergency researcher in Canada, about the key historical and examination pearls to help pick up this sometimes elusive diagnosis, what the value of serum ketones are in the diagnosis of DKA, how to assess the severity of DKA to guide management, how to avoid the dreaded cerebral edema that all too often complicates DKA, how to best adjust fluids and insulin during treatment, which kids can go home, which kids can go to the floor and which kids need to be transferred to a Pediatric ICU.
Why Recording Time to Initial Assessment is Worthwhile
As both an emergency director and a practising emergency physician, I believe it is the job of administrators to make the challenges of front line staff easier, not vice-versa. Clinicians are too busy taking care of patients to perform purely administrative chores. But one task that I would ask all emergency doctors to adopt is the step of recording the time of Physician Initial Assessment, or PIA times. The time from arrival until they first see a physician is what most patients consider their ED wait time, and it is an important metric to report. Yes, it means one more small box to fill out in your charting, but it can be of huge benefit to doctors. Allow me to explain why....
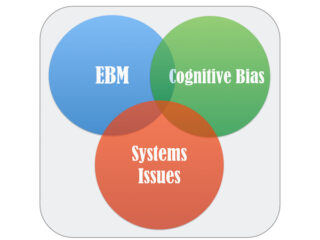
Episode 62 Diagnostic Decision Making in Emergency Medicine
This is Part 1 of EM Cases' series on Diagnostic Decision Making with Walter Himmel, Chris Hicks and David Dushenski discussing the intersection of evidence-based medicine, cognitive bias and systems issues to effect our diagnostic decision making in Emergency Medicine. In this episode we first discuss 5 strategies to help you master evidence-based diagnostic decision making to minimize diagnostic error, avoid over-testing and improve patient care including: 1. The incorporation of patients' values and clinical expertise into evidence-based decisions 2. Critically appraising diagnostic studies 3. Understanding that diagnostic tests are not perfect 4. Using the concept of test threshold to guide work-ups 5. Understanding that the predictive value of a test depends on the prevalence of disease We then go on to review some of the factors that play into the clinician’s and patient’s risk tolerance in a given clinical encounter, how this plays into shared decision making and the need to adjust our risk tolerance in critical situations. Finally, we present some strategies to prevent over-testing while improving patient care, patient flow and ethical practice.
Best Case Ever 35: Taking Action in Emergency Medicine
In anticipation of our series of podcasts on Diagnostic Decision Making with Dr. Walter Himmel, Dr. Chris Hicks and Dr. David Dushenski we have Dr. Hicks presenting his Best Case Ever. Taking action in Emergency Medicine requires not only careful consideration of the best evidence, the experience of the clinician, the patient's values and the system that you work in, but also the will to act. Dr. Hicks describes a case of a patient who suffers a cardiac arrest, where the diagnosis is quite obvious to everyone in the room (and the required action is as well), yet a delay in treatment occurs nonetheless.