In this EM Cases episode on Pediatric Asthma we discuss risk stratification (including the PASS and PRAM scores), indications for CXR, the value of blood gases, MDIs with spacer vs nebulizers for salbutamol and ipatropium bromide, the best way to give corticosteroids, the value of inhaled steroids, the importance of early administration of magnesium sulphate in the sickest kids, and the controversies around the use of ketamine, heliox, high flow nasal cannuala oxygen, NIPPV, epinephrine and IV salbutamol in severe asthma exacerbations. So, with the multinational and extensive experience of Dr. Dennis Scolnik, the clinical fellowship Program Director at The Hospital for Sick Children in Toronto and Dr. Sanjay Mehta, multiple award winning educator who you might remember from his fantastic work on our Pediatric Orthopedics episode, we’ll help you become more comfortable the next time you are faced with a child with asthma who is crashing in your ED…
Written Summary and blog post written by Anton Helman, April 2016
Cite this podcast as: Scolnik, D, Mehta, S, Helman, A. Management of Acute Pediatric Asthma Exacerbations. Emergency Medicine Cases. April, 2016. https://emergencymedicinecases.com/pediatric-asthma/. Accessed [date].
Pediatric Asthma Severity Indicators on History
- life-threatening exacerbations
- admissions to ICU
- intubation
- deterioration while already on systemic steroids
- using more than 2 canisters of short acting B-agonist per month
- cardiopulmonary and psychiatric comorbidities
Its important to realize that a lack of risk factors does not necessarily confer a lack of risk, so even if a patient has none of these risk factors, they can still be at risk for deterioration from their asthma.
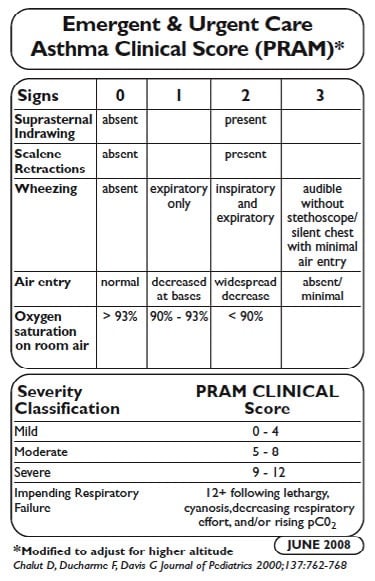
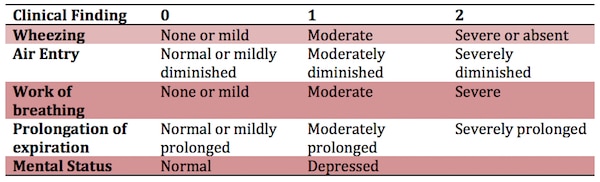
Reliable Validated Measures of Pediatric Asthma Severity
PASS Score for Pediatric Asthma Severity
VBG in Pediatric Asthma
A PaCO2 >42 is indicative but not diagnostic of a severe exacerbation
A PaCO2 >50 is a risk factor for impending respiratory failure
Metabolic Acidosis is an indicator of impending arrest!
A VBG is seldom indicated unless the child has no clinical improvement with maximal therapy. The timing of the VBG is important: It may be most useful as a baseline after ED treatment in a patient going to the ICU.
Don’t forget the classic teaching: A ‘normal’ Hg partial pressure of CO2 in a patient with extreme tachypnea and retractions could indicate impaired ventilation and impending respiratory failure.
Indications for CXR in presumed Pediatric Asthma
The rate of CXR use in kids with asthma increased significantly from the mid 90’s to around 2010. Although it’s not unreasonable for first time wheezers to get a baseline CXR, it’s important to realize that an unsuspected diagnosis made on the basis of a CXR in an acutely wheezing child is rare, even if the child has never wheezed before.
In fact there are no set of predictors in the literature that can accurately identify children likely to have abnormalities on CXR.
Nonetheless, some situations that might warrant a CXR in a child with a wheeze, are focal chest findings, fever, subcutaneous emphysema or a history of choking.
MDI vs Nebs vs IV B-agonists in Pediatric Asthma
Compared with nebulized treatments, metered-dose inhaler (MDI) with a spacer use has been shown to be equally effective for children of all ages with a wide range of illness severity and by multiple outcome measures. Among children 1 to 4 years old, using a MDI with a spacer was associated with a greater reduction in wheezing and a lower hospitalization rate in one study.
Furthermore, a recent cost analysis determined that the use of MDIs to treat children with mild to moderate asthma exacerbations in the ED could yield significant cost savings compared with nebulized treatments. MDIs with a spacer should not be used in patients with impending respiratory failure and it can be difficult to coordinate breathing with administration of the inhaler for patients less than 1 year old.
IV beta-agonists have not been shown to be superior to inhaled beta-agonists. IV beta-agonists should be considered in those who are unable to tolerate nebulized or MDI treatments.
For < 15 kg: Salbutamol MDI 4 puffs or 2.5mg nebulized in 2-3ml NS x3 back to back (continuously) For > 15kg: Salbutamol MDI 8 puffs or 5mg nebulized in 2-3ml NS x3 back to back (continuously)
A Cochrane review found that those treated with continuously nebulized bronchodilators had lower rates of hospitalization, greater improvements in pulmonary function test results, and similar rates of adverse events compared with those treated intermittently. Continuous treatment allows greater compliance with the goal of delivering the equivalent of three intermittent bronchodilator treatments in the first hour of care. In addition, this method will result in less respiratory therapy time and costs; it has been shown to be safe, and it may benefit the sickest patients the most.
In children receiving multiple beta-agonist treatments, watch for hypokalemia, especially if the patient has diarrhea, or is on diuretic medications.
B-agonists with Ipatropium Bromide are more effective than B-agonists alone in Pediatric Asthma
In a systematic review and meta-analysis comparing the use of beta-agonists plus anticholinergics with beta-agonists alone, combination therapy was associated with significantly lower hospitalization rates and improvements in asthma scores and pulmonary function test results.
So multiple doses of ipatropium bromide added to beta-agonists are indicated for kids with moderate to severe asthma exacerbations. However, there are no clinical trials supporting ipratropium use beyond the first hour or first 3 doses in children.
Ipatromium Bromide dosing: MDI 4 puffs (80mcg) or 250mcg nebulized
Single dose Dexamethasone is the preferred oral corticosteroid for Pediatric Asthma
A study out of the Annals of EM entitled “A Randomized Trial of Single-Dose Oral Dexamethasone Versus Multidose Prednisolone for Acute Exacerbations of Asthma in Children Who Attend the Emergency Department”, showed that a single dose of dexamethasone dosed at 0.3mg/kg orally compared to prednisolone dosed at 1mg/kg for 3 days in 245 children with known asthma had equivalent PRAM scores at day 4. This is consistent with 3 previous RCTs, the largest of which dosed dexamethasone at 0.6mg/kg po.
So, it is reasonable to give one dose of dexamethasone at 0.3-0.6mg/kg po just prior to starting bronchodilators to all but the sickest of kids who present to the ED with an asthma exacerbation, obviating the need for an outpatient prescription.
It’s also worth noting that dexamethasone is associated with less vomiting compared to prednisolone as well.
Update 2022: A prospective, randomized, single center randomized clinical trial of 318 patients 2 to 20 years of age presenting to a pediatric ED with mild to moderate asthma exacerbation found no difference in the rate of return visits for continued or worsened symptoms, days to symptom resolution, missed school days, or vomiting between patient randomized to 1 or 2 doses of dexamethasone. Abstract
Inhaled corticosteroids
While there’s no evidence that the use of inhaled steroids in the ED are beneficial there is evidence that they decrease relapse rates in the outpatient setting.
The maximum dose of inhaled steroid is the equivalent of Fluticasone (Flovent in Canada) of 100 micrograms 2 puffs twice daily for a maximum of 200 micrograms per day. There is evidence based on observational data from the Canadian Paediatric Surveillance Program that higher doses may lead to adrenal suppression and in some cases adrenal shock.
Discharge Criteria for Pediatric Asthma
Discharge criteria from the ED include:
- Needing beta-agonists less often than q4 h after 4 to 8 h of conventional treatment
- A reading of SpO2 94% on room air
- Minimal or no signs of respiratory distress
- Improved air entry
Discharge Instructions for Pediatric Asthma
- Prepare a written asthma action plan with medications and signs to look out for that would necessitate a return to the ED
- Continue to use a short-acting beta-agonists such as salbutamol until exacerbation resolves and then as needed, with directions to see a health care professional if therapy is needed more often than every 4h.
- For all but the mildest of asthma patients seen in the ED, a prescription for 3 weeks of inhaled streroid such as fluticasone 50 micrograms, 2 puffs twice daily.
- Review techniques for using inhaled asthma medications as well as for cleaning/maintaining the inhaler device. Parents must understand that they need to use the MDI spacer and that the mask fits properly, to use the B-agonist BEFORE the inhanled steroid and to wash the mouth out after the steroid inhaler to prevent thrush.
- Encourage follow-up with the patient’s primary care physician or a local asthma clinic to review asthma control, environmental history and symptom recognition.
Peak expiratory flow should NOT be relied upon solely as a measure of severity or as a sole determinate for discharge.
IV Magnesium Sulphate in Pediatric Asthma
A meta-analyses suggests that use of magnesium sulphate results in improved outcomes for both adults and children, improving respiratory function and decreasing hospital admissions. IV magnesium sulphate may be considered in cases of moderate and severe asthma with incomplete response to conventional.
IV magmesium sulphate 40mg/kg should be given EARLY to patients with severe asthma who do not substantially improve after the first 6o minutes of bronchodilator and steroid therapy.
The most common adverse effect is hypotension; this may be avoided by infusion of the dose over 20 minutes and giving a fluid bolus prior to or during the magnesium infusion.
If there is a delay in obtaining an IV, magnesium sulphate can be given IO or inhaled via nebulizer.
What about Nebulized Magnesium Sulphate?
The RCT entitled MAGNETIC trial in 2013 of about 500 children showed that MgSO4 2.5mL of 250mmol/L solution q20mins x 3 added to the salbutamol and ipratropium bromide nebulizer in the first hour for kids with acute severe asthma, significantly improved asthma severity scores without any increase in adverse events.
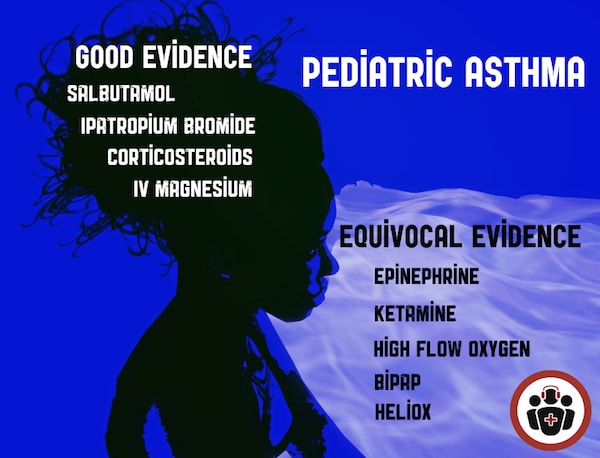
Pediatric Asthma Therapy with Equivocal or Mixed Evidence that may be indicated when all else has failed
Up to 26% of children intubated due to asthma suffer complications including pneumothorax, impaired venous return, and cardiovascular collapse because of increased intrathoracic pressure. Mechanical ventilation during an asthma exacerbation is associated with an increased risk of death and should be considered as a last resort and in conjunction with the support of a paediatric ICU specialist.
IM Epinephrine – time tested but no good evidence
IM epinephrine at the same doses used in anaphylaxis (0.01mg/kg of 1:1000, max 0.3mg given in the anterolateral thigh) has been used for decades in children with severe asthma, however there have been no robust RCTs to support it’s use.
Heliox – reserve for the ICU
According to the Canadian Pediatric Society Guidelines for Managing the Patient with Acute Asthma Exacerbation, using a helium-oxygen gas mixture should be reserved for children in the ICU setting with severe asthma exacerbation who have failed to improve despite maximized therapy.
Ketamine to avoid intubation – 3 Mixed Studies
A limited case series has reported the effectiveness of a bolus (2 mg/kg) followed by a continuous infusion (2 to 3 mg/kg/h) of ketamine in children with severe asthma who were approaching respiratory failure. In this study, the use of ketamine resulted in prompt improvement and avoided the need for endotracheal intubation. This is an appealing use of ketamine, because it may allow one to avoid the hazards of endotracheal intubation and mechanical ventilation in the patient with asthma.
A randomized control trial showed no improvement in pulmonary index scores with the administration of ketamine to patients with moderate to severe asthma. Patients were randomized to 0.2mg/kg ketamine bolus followed by 0.5mg/kg/h for 2 hours vs placebo.Pulmonary index scores were measured throughout the 2 hours and no difference was found.
In a 2001 prospective, observational, single-arm pilot study in two pediatric EDs over three months, the effect of IV ketamine added to standard therapy in status asthmaticus wasevaluated. Initiation of ketamine in patients with severe asthma was associated with clinical improvement. Side effects were easily managed with treatment or discontinuation of ketamine.
The take home message is that more convincing evidence is required before ketamine can be recommended for routine treatment of severe pediatric asthma to avoid intubation.
Ketamine, however, is safe at dissociative dosages, and is a reasonable option when all others measures have failed.
BiPAP – the pediatric literature isn’t quite as impressive as the adult literature
A few case reports and observational studies of the use of BiPAP in pediatric asthma show some promise. The one RCT of only 20 patients does show a benefit in clinical asthma scores, respiratory rate, and supplemental oxygen need. While intuitively sensible, there is no evidence that NIPPV prevents the need for intubation in children with status asthmaticus.
Similar to other rescue measures, NIPPV can be considered when all others measures have failed in hopes of avoiding endotracheal intubation.
High Flow Nasal Cannula – gaining popularity
Another way of providing a bit of noninvasive positive pressure that seems to becoming popular among the pedatricians is high flow nasal cannula oxygen. The evidence is conflicting for this, and most studies were done in kids with bronchiolitis rather than asthma.
One study from Pediatric Emergency Care in 2012 showed that the use of high flow nasal oxygen reduced the need for intubation in pediatric acute respiratory failure, but there was no change in mortality or ICU length of stay.
However, a Cochrane review in 2014 based on 11 studies concluded that no evidence could be found to allow determination of the safety or effectiveness of HFNC therapy in children.
The latest study out of Emergency Medicine Journal concluded that HFNC may have a role, but about 1/3 of patients required BiPAP or intubation.
IV salbutamol – may improve recovery time and length of stay
Two RCTs showed a more rapid recovery time and earlier discharge from hospital when IV salbutamol was compared to nebulized ipratopium bromide in one of the studies, and compared to continuous salbutamol nebs in another. When using IV salbutamol, be on the lookout for excessive tachycardia, low DBP and rising lactate. Start at 1mcg/kg/min infusion and titrate to 5mcg/kg/min.
The decision to intubate should be based on clinical judgement as
opposed to any single vital sign or blood gas result. Some variables to consider for intubation are worsening hypercapnea, patient exhaustion and changes in mental status.
Putting it all together for Severe Pediatric Asthma Exacerbation: A Step-wise Approach
*note that the blue indicates evidence-based treatment while the red indicates therapies that are reasonable to try when all else has failed but do not have strong evidence for benefit
Put the child on the cardiac monitor
|
Obtain IV access and draw blood work including electrolytes and a VBG
(with particular attention to the K)
|
Call your RT and pediatric intensivist early
|
Continuous salbutamol nebulizers with the first 3 including ipratropium bromide
|
IV steroids: methylprednisolone 1mg/kg or hydrocortisone 5mg/kg
(if dexamethasone 0.3mg/kg, max 10mg was not given prior to starting nebs)
|
IV NS 20mL/kg bolus (preferably before the MgSO4)
|
IV Magnesium Sulphate 40mg/kg to a maximum of 2g over 20 mins
(in the first hour if possible)
|
Consider epinephrine 0.01mg/kg IM and nebulized MgSO4
(especially if you are having trouble obtaining IV access)
|
Consider BiPaP or high flow nasal oxygen
|
Consider IV salbutamol 1-5mcg/kg/min
(beware tachycardia, low DBP, rising lactate)
|
Consider subdissociative dose ketamine
|
Consider Heliox
Quote of the Month
“Knowledge is not only power; it is happiness,
and being taught is the intellectual analog of being loved.”
– Isaac Asimov
For more on Paediatric Emergencies download our free interactice eBook EM Cases Digest Vol. 2 Pediatric Emergencies
Dr. Helman, Dr. Mehta and Dr. Scolnik have no conflicts of interest to declare
Key References
Gorelick MH, Stevens MW, Schultz TR, Scribano PV. Performance of a novel clinical score, the
Pediatric Asthma Severity Score (PASS), in the evaluation of acute asthma. Acad Emerg Med
2004;11(1):10-8.
Belessis Y, Dixon S, Thomsen A, et al. Risk factors for an intensive care unit admission in children
with asthma. Pediatr Pulmonol 2004;37(3):201-9.
Chalut DS, Ducharme FM, Davis GM. The Preschool Respiratory Assessment Measure (PRAM): A
responsive index of acute asthma severity. J Pediatr 2000;137(6):762-8.
Birken CS, Parkin PC, Macarthur C. Asthma severity scores for preschoolers displayed weaknesses
in reliability, validity, and responsiveness. J Clin Epidemiol 2004;57(11):1177-81.
Gershel JC, et al: The usefulness of chest radiographs in first asthma attacks. Engl J Med 309: 336, 1983.
Castro-Rodriguez JA, Rodrigo GJ: Beta-agonists through metered-dose inhaler with valved holding chamber versus nebulizer for acute exacerbation of wheezing or asthma in children under 5 years of age: A systematic review with meta-analysis. J Pediatr 2004; 145:172.
Camargo CA, Spooner CH, Rowe BH. Continuous versus intermittent beta-agonists in the treatment of acute asthma. Cochrane Database Syst Rev. 2003;(4):CD001115.
Randolph C. Dexamethasone for acute asthma exacerbations in children: a meta-analysis. Pediatrics. 2014;134 Suppl 3:S178-9.
Cronin JJ, Mccoy S, Kennedy U, et al. A Randomized Trial of Single-Dose Oral Dexamethasone Versus Multidose Prednisolone for Acute Exacerbations of Asthma in Children Who Attend the Emergency Department. Ann Emerg Med. 2015; 134:432.
Rodrigo GJ, Castro-Rodriguez JA: Anticholinergics in the treatment of children and adults with acute asthma: A systematic review with meta-analysis. Thorax 2005; 60:740.)
Goldbloom E, Ahmet A. Adrenal suppression: An under-recognized complication of a common therapy. Paediatr Child Health. 2010;15(7):411-2. Full PDF
Rowe BH, et al: Intravenous magnesium sulfate treatment for acute asthma in the emergency department: A systematic review of the literature. Ann Emerg Med 2000; 36:181. Full PDF
Cheuk DK, Chau TC, Lee SL: A meta-analysis on intravenous magnesium sulphate for treating acute asthma. Arch Dis Child 2005; 90:74.
Powell CV, Kolamunnage-dona R, Lowe J, et al. MAGNEsium Trial In Children (MAGNETIC): a randomised, placebo-controlled trial and economic evaluation of nebulised magnesium sulphate in acute severe asthma in children. Health Technol Assess. 2013;17(45):v-vi, 1-216.
O Ortiz-Alvarez, A Mikrogianakis; Managing the Patient with an acute asthma exacerbation. Canadian Paediatric Society,Paediatr Child Health 2012;17(5):251-5
Denmark TK, Crane HA, Brown L: Ketamine to avoid mechanical ventilation in severe pediatric asthma. J Emerg Med 30: 163, 2006.
Allen JY, Macia CG. The efficacy of ketamine in pediatric emergency department patients who present with acute severe asthma. Ann Emerg Med. 2005;46(1):43-50.
Petrillo TM, Fortenberry JD, Linzer JF, Simon HK. Emergency department use of ketamine in pediatric status asthmaticus. J Asthma. 2001; 38(8):657-664.
Basnet S, Mander G, Andoh J, Klaska H, Verhulst S, Koirala J. Safety, efficacy, and tolerability of early initiation of noninvasive positive pressure ventilation in pediatric patients admitted with status asthmaticus: a pilot study. Pediatr Crit Care Med. 2012;13(4):393-8.
Wing R, James C, Maranda LS, Armsby CC. Use of high-flow nasal cannula support in the emergency department reduces the need for intubation in pediatric acute respiratory insufficiency. Pediatr Emerg Care. 2012;28(11):1117-23.
Mayfield S, Jauncey-cooke J, Hough JL, Schibler A, Gibbons K, Bogossian F. High-flow nasal cannula therapy for respiratory support in children. Cochrane Database Syst Rev. 2014;3:CD009850.
Long E, Babl FE, Duke T. Is there a role for humidified heated high-flow nasal cannula therapy in paediatric emergency departments?. Emerg Med J. 2016.
Browne GJ, Trieu L, Van asperen P. Randomized, double-blind, placebo-controlled trial of intravenous salbutamol and nebulized ipratropium bromide in early management of severe acute asthma in children presenting to an emergency department. Crit Care Med. 2002;30(2):448-53.
Browne GJ, Penna AS, Phung X, Soo M. Randomised trial of intravenous salbutamol in early management of acute severe asthma in children. Lancet. 1997;349(9048):301-5.
Additional FOAMed Resources for Pediatric Asthma
Evidence-based slide set on ED pediatric asthma management from CAEP 2015 Conference
Mechanical Ventilation in Severe Asthma on Pediatric EM Morsels
Asthma and The Vent on PEM ED podcast
Best Bets review on Ketamine in Severe Asthma
St. Emlyns on Why don’t we just use dexamethasone?
Ryan Radecki on Early Administration of Steroids in Pediatric Asthma
For more EM Cases content on Pediatric Emergencies download our free eBook,
EM Cases Digest Vol. 2 Pediatric Emergencies here.




[…] Helman goes through an evidence based approach to management of asthma exacerbations in children. […]
Simple but covers all the basics, enjoyable read through
Thank you