Pain is the most common reason for seeking health care. It accounts for 80% of ED visits. The WHO has declared that “optimal pain treatment is a human right”. As has been shown in multiple ED-based Pediatric pain management studies, Pediatric pain is all too often under-estimated and under-treated. Why does this matter? Under-estimating and under-treating pediatric pain may have not only short term detrimental effects but life-long detrimental effects as well; not to mention, screaming miserable children disturbing other patients in your ED and complaints to the hospital from parents. Whether it’s venipuncture, laceration repair, belly pain or reduction of a fracture we need to have the skills and knowledge to optimize efficient and effective pain management in all the kids we see in the ED. What are the indications for intranasal fentanyl? intranasal ketamine? Why should codeine be contra-indicated in children? How do triage-initaited pain protocols improve pediatric pain management? Which are most effective skin analgesics for venipuncture? To help you make these important pediatric pain management decisions, in this podcast we have one of the most prominent North American researchers and experts in Emergency Pediatric pain management, Dr. Samina Ali and not only the chief of McMaster Children’s ED but also the head of the division of Pediatric EM at McMaster University, Dr. Anthony Crocco.
Written Summary and blog post prepared and written by Dr. Anton Helman, July 2015
Cite this podcast as: Helman, A, Ali, S, Crocco, A. Pediatric Pain Management. Emergency Medicine Cases. July, 2015. https://emergencymedicinecases.com/pediatric-pain-management/. Accessed [date].
Why is Pediatric Pain Management Important?
Short-term detrimental effects of painful procedures
- Extended procedure duration and length of stay
- Slower surgical healing
- Emotional trauma and suffering
Long-term detrimental effects of painful procedures
- Infant pain may actually change pain processing
- Avoidance/heightened sensitivity to medical care
- Fear/increased pain experienced healthcare evaluation
Pediatric Pain Assessment Tools
A) Infants
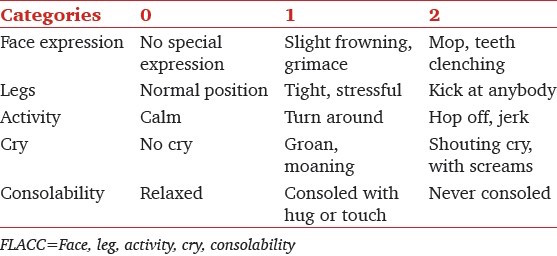
FLACC Scale (out of a total score of 10)
B) 4-8 years old
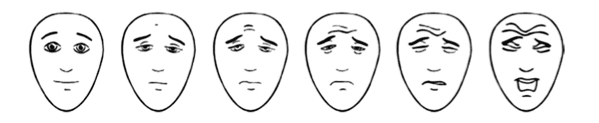
Faces Pain Scale Revised (child points to face that best describes their pain)
C) 8-15 years old
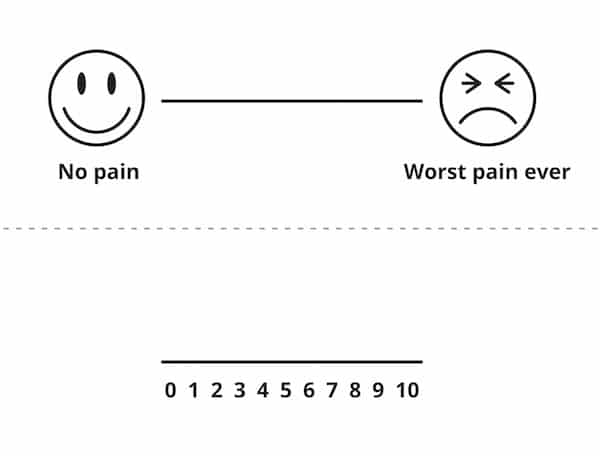
Visual Analog Scale
Do vital signs help in Pediatric Pain Assessment?
There is no correlation between improvement in pain scores and changes in heart rate, respiratory rate or blood pressure. Using vital signs to assess pain in children may be misleading.
Triage-Initiated Pain Protocols
A nurse-driven protocol at triage has been shown to improve time-to-analgesia. Many Canadian hospitals employ oral acetaminophen or ibuprophen triage-initiated pain protocols, and some in Canada and Australia employ intranasal fentanyl and oral opiods.
Low Resource Utilization Distraction Techniques
Infants
- Breastfeeding or breast milk has been shown to temper pain but has not been established for repeated painful procedures
- Oral Sucrose (2mL) reduces signs of distress in infants when given 2 minutes before the procedure and the analgesic effect can be augmented with non-nutritive sucking via a pacifier. If oral sucrose is not available, D25W 2mL is a reasonable replacement.
- An infant warmer or warm blanket
Toddlers and Older Children
- Music has been shown to minimize the pain and anxiety associated with painful procedures in children. Simply using a parents smartphone or tablet device to play a child’s favorite music is a low-cost simple distraction technique.
- Guided Visual Imagery may be of particular benefit to children as they are generally accepting of the idea of fantasy and suggestion. The dissociative effects of Ketamine in particular make it an ideal agent for the adjunctive use of guided imagery.
Topical Analgesic Options For Venipuncture
1. EMLA has an analgesic onset of 60 minutes after application and so is not recommended for wide use in the ED where a shorter onset is usually required.
2. Amethocaine 4% gel (Ametop) has been shown to be superior to EMLA for reducing overall needle insertion pain with less needle attempts required and the onset is faster (30 mins) than EMLA.
3. Liposomal Lidocaine 4% (LMX-4, Maxilene, ELA-Max) also has an onset of 30 mins and has been shown to be effective in pediatric patients for LP in particular.
4. Vapocolant spray has the advantange of immediate analgesic onset, however it is only suitable for procedures that are anticipated to require brief analgesia.
5. J-tip with buffered lidocaine (Zingo) is a needle-free injector with analgesic effect in 1-3mins. The J-tip eliminates the ‘second poke’ for venipuncture, decreases the risk of needle stick injury, and decreases the risk of infection transmission, however the evidence is weak (one study compared J-tip with buffered lidocaine to sham only and another compared it to an EMLA group, many of whom did not have the full 60 minutes of topical application)
Graded Analgesic Options for Pain Anticipated to Last Hours to Days
Mild-Moderate Pain:
Ibuprophen (10mg/kg q6h) has been shown in several studies to be superior to Acetaminophen (15mg/kg q4h) for mild-moderate musculo-skeletal pain in children. While the combination of Ibuprophen and Acetominophen has been shown in adult studies to be superior to either one alone, this has not been adequately studied in children. Nonetheless, our experts do recommend using the combination of ibuprophen and acetaminophen in the ED. While outpatient use of the this combination may lead to dosing errors and inadvertent overdose, it may be considered for children with reliable parents who have been counseled appropriately.
Moderate-Severe Pain:
Oral morphine suspension at 0.2-0.5mg/kg (max 15mg) with or without ibuprophen
Intravenous morphine is recommended by our experts for children with severe pain in whom you expect a prolonged period of pain of hours-days (eg: suspected appendicitis) at a dose of 0.1mg/kg IV push with frequent reassessments and titration to adequate pain control every 10 minutes. An oxygen saturation monitor is recommended for children receiving multiple doses of morphine.
Step-Wise Ladder Approach to Outpatient Pain Management
Low-Moderate: acetominophen or ibuprophen or both
Modrate-Severe: oral morphine or oxycodone-acetominophen – Roxacet suspension (available in United States)
|
Pain Severity |
Agents of Choice |
|
Mild pain |
ibuprophen +/- acetominophen |
|
Moderate pain |
ibuprophen +/- acetaminophen + morphine |
|
Severe pain |
ibuprophen +/- acetaminophen + morphine or oxycodone |
Codeine Should Almost Never be Given to Children or Breastfeeding Mothers
Codeine has a very wide bioavailability depending on the individual’s metabolism. Some individuals are slow metabolizers, while others are rapid metabolizers, and so the effects of codeine are unpredictable. There have been numerous case reports of pediatric deaths related to the use of ‘therapeutic’ doses of codeine.
The story of Tariq & Rani Jamieson: Tariq was a breastfed healthy term infant who was born in Toronto in 2005. Rani, his mother, was prescribed Tylenol #3 for episiotomy pain, which was taken at ‘therapeutic’ doses. On Day 7 of life, Rani noticed that Tariq was lethargic and on Day 11 was seen by his primary care physician for poor feeding. Rani had decreased her Tylenol #3 dose to 1 tablet twice daily. Nonetheless on Day 13 Tariq was found motionless and breathless in the family kitchen, and despite EMS attempts at resuscitation, was pronounced dead. The post-mortem examination discovered that Tariq had 7 times the acceptable morphine concentration (metabolite of Codeine) in his blood. Rani was phenotyped as an ultra-rapid metabolizer of Codeine, and the cause of death was determined to be Codeine overdose.
Analgesic Options for Pain Anticipated to Last Minutes or as A Bridge to Intravenous Analgesics
Nitrous Oxide
Nitrous Oxide is a relatively weak dissociative anesthetic gas with mild-moderate anxiolytic, analgesic and amnesic properties. It has a rapid onset of 5 minutes and recovery of 5-15 minutes. The rate of adverse events (vomiting, dizziness, euphoria/dysphoria) is low (0.03%) and most hospital protocols do not require fasting for it’s use.
Intranasal Analgesics & Anxiolytics
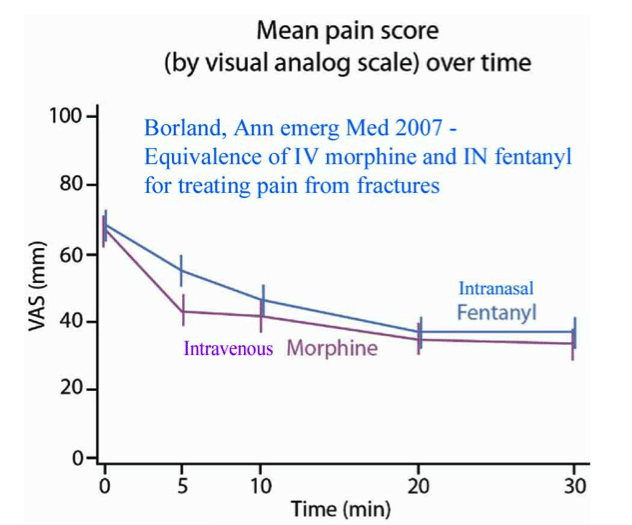
Intranasal Fentanyl (1-1.5mcg/kg IN) has comparable effects to IV Morphine (see graph), with a rapid onset and high bioavailability.
A general rule of thumb for dosing intranasal medication is to use twice the IV dose. Administer IN fentanyl using an atomizer in the most concentrated available formulation, and if more than 0.3mL is required, consider splitting the dose and administering one half in one nare and the other half in the other nare so that the absorptive area is maximized. With appropriate doses, respiratory depression is rare and can be reversed with intranasal naloxone.
Intranasal Ketamine (1mg/kg IN) in children 3-13 years of age with isolated limb injury and moderate to severe pain was shown in the PITCHFORK study in 2015 to have similar pain reduction when compared to IN Fentanyl 1.5mcg/kg in a randomized controlled fashion. In this study 78% of children had minor adverse events with ketamine compared to 40% with fentanyl, however none suffered moderate or severe adverse events.
Intranasal Midazolam is an effective anxiolytic in children however a significant proportion of children will suffer from more anxiety after receiving midazolam; therefore our experts do not recommend it as a first line anxiolytic.
Do Children Receiving Skin Adhesive for Laceration Repair Require Analgesia?
Lidocaine Epinephrine Tetracaine (LET) gel has been shown to decrease pain in children with lacerations that are treated with skin adhesive in an RCT. Some pediatric emergency departments employ nurse-initiated LET application at triage for all children with lacerations, regardless of the method of laceration closure used.
Quote of the Month
Pain is inevitable. Suffering is optional.
-Dalai Lama
For more on Paediatric Emergencies download our free interactice eBook EM Cases Digest Vol. 2 Pediatric Emergencies
Key References
Weisman S, Bernstein B, Schechter N. Consequences of inadequate analgesia during painful procedures in children. Arch Pediatr Adolesc Med. 1998;152:147-149. Abstract
Poonai N, et al. Opioid analgesia for acute abdominal pain in children: A systematic review and meta-analysis. Acad Emerg Med. 2014 Nov;21(11):1183-92. doi: 10.1111/acem.12509. Review. Abstract
Zier JL, Liu M. Safety of High-Concentration Nitrous Oxide by Nasal Mask for Pediatric Procedural Sedation. Pediatr Emerg Care 2011; 27: 1107-1112. Abstract
Poonai N et al. Oral administration of morphine versus ibuprofen to manage postfracture pain in children: a randomized trial. CMAJ. 2014 Dec 9;186(18):1358-63. Abstract
William T. Zempsky. Pharmacologic Approaches for Reducing Venous Access Pain in Children. Pediatrics 2008;122;S140. Abstract
Harman, S. Efficacy and pain control with topical lidocaine-epinephrine-tetracaine during laceration repair with tissue adhesive in children: a randomized controlled trial. CMAJ. 2013 Sep 17;185(13):E629-34. Abstract
Curtis SJ et al. A randomized controlled trial of sucrose and/or pacifier as analgesia for infants receiving venipuncture in a pediatric emergency department. BMC Pediatr. 2007 Jul 18;7:27. Abstract
Graudins A et al. The PICHFORK (Pain in Children Fentanyl or Ketamine) trial: a randomized controlled trial comparing intranasal ketamine and fentanyl for the relief of moderate to severe pain in children with limb injuries. Ann Emerg Med. 2015 Mar;65(3):248-254.e1. Abstract
Dr. Helman, Dr. Ali & Dr. Crocco have no conflicts of interest to declare

For more EM Cases content on Pediatric Emergencies check out our free interactive eBook,
EM Cases Digest Vol. 2 Pediatric Emergencies here.
Now test your knowledge with a quiz.





Im a Intensive Care Paramedic and previous Extended Paramedic. I only just started listening to these pod casts, quite enjoying the discussion. I find in the pre hospital area that Fentanyl IN works really well with kids (and adults), particularly with burns. For that easy and rapid pain relief. As I dont see the very little ones in a rural setting frequently enough to be proficient with IV access, this IN route is a great back up route. We use to use nitrous oxide but that has been removed sometime ago. It was very handy to have at times. I have seen it used to allow facial suturing to occur in a little 6 year old female, with great success. Australia pre hospital services use Penthrox (Methoxyflurane) as an inhalation analgesic. This also is a easy to use (for compliant kids) and works quite well and gives you time to not only relieve pain but get an IV in that they tend not to remember. To finish off pharmacological wise my ambulance pain arsenal is Penthrox, morphine, fentanyl and ketamine (not for under 14 yo). Kind regards Mick
Thanks for the tip on Methoxyflurane Mick. Not sure if it’s used in Canada much. I wonder about it’s effectiveness compared to NO and it’s safety profile. I’ll ask our local experts. Cheers. Anton
Vapocoolant sprays must never be used near heat or ignition sources as they are flammable and bad accidents can and have occurred ..
Home availability is particularly dangerous .
Great review, I just want to make a comment on subcutaneous Morphine since you havent mention it. In in our hospital in spain we use it when we dont have an IV placed and when we suspect of a pain that will last longer for example burns… with a rapid onset compared with IV and longer lasting time than Fentanyl. For Fractures IN fentanyl or Ketamine is our best option. What are your commments about it? Thanks.
Leave some reference about this:
Penson RT, Joel SP, Roberts M, Gloyne A, Beckwith S, Slevin ML. The bioavailability and pharmacokinetics of subcutaneous, nebulized and oral morphine-6-glucuronide. Br J Clin Pharmacol. 2002;53(4):347–354. doi:10.1046/j.1365-2125.2002.01554.x
Rural GP here. Love these podcasts, and this episode on pain management just helped us manage a 4 yr old with a burn today. Thanks for this high quality information.