In this CritCases blog – a collaboration between STARS Air Ambulance Service, Mike Betzner and EM Cases – we discuss a challenging case of pulmonary hypertension where a fine balance in volume resuscitation, oxygenation and ventilation is critical.
Written by Michael Misch; Edited by James Brokenshire & Anton Helman; Expert Peer Review by Susan Wilcox (EM, Critical Care and Pulmonary physician at Medical University of South Carolina, Medical Director for MEDUCARE Ground Transport Service and the Medical Director for Emergency Teams, the inpatient emergency response service.) March, 2017
The Case
A 67-year old female with pulmonary hypertension secondary to scleroderma, on 8L of home oxygen at baseline, presents to a community hospital complaining of a 12-hour history of increasing shortness of breath. There is 
Ground EMS finds the patient to have severe shortness of breath with peripheral cyanosis and an oxygen saturation of 75%, respiratory rate of 30 on her 8 L oxygen via nasal prongs. When switched to a non-rebreather, her saturation increases to 88%. She is afebrile, heart rate of 88 bpm and blood pressure of 91/51.
The patient is brought to a community hospital where the local physician orders preliminary investigations and calls for transfer to a tertiary center. Flight time 35 is minutes. You prepare your transport crew.
What initial advice would you give to the community physician while you are en route for this patient with pulmonary hypertension?
First – Call pulmonary service ASAP. People do entire fellowships in the management of pulmonary hypertension.
Second – volume status is very hard to assess in these patients – I would advise a small bolus of fluid 250 cc. No more.
Third – hypoxia, hypercarbia and acidosis kills these patients. So reverse what you can as gently as possible. O2 – maximize non-invasive. Small settings as too much afterload/preload reduction and this patient is dead.
-Andrew Fagan, MD FRCPC
You absolutely need to involve the patient’s specialist in their care early and arrange transfer as soon as possible. Until the patient reaches a tertiary care center, you should consider doing fewer interventions rather than more. Large fluid boluses and attempts at intubation will likely kill the patient. Give 15 L oxygen via a non-rebreather and consider adding 15 L oxygen by nasal cannulae to increase Fi02. If you are going to give IV fluids, bolus only 250 cc at a time with prompt reassessment.
It is crucial to identify the underlying cause for decompensation in this patient. This would include electrolytes, blood cultures, lactate, ECG/troponin and portable CXR.
Case continued…
The community physician orders the following investigations and places the patient on a non-rebreather.
| Na | 132 | Hb | 91 | pH | 7.36 |
| K | 5.4 | Lk | 113 | pCO2 | 33 |
| Cl | 101 | Plt | 350 | HCO3 | 19 |
| HCO3 | 19 | pO2 | 24 | ||
| Cr | 142 (101 baseline) | Lactate | 5.0 | ||
| Glc | 6.0 | ||||
| Urea | 12.1 | ||||
| Troponin | 0.02 | ||||
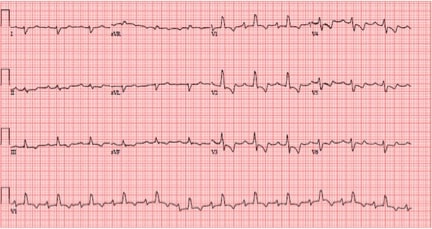
ECG
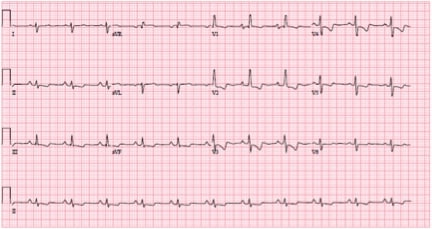
Old ECG
ECG interpretation: RBB, RAD, anterior and inferior T-wave inversions, all typical right of right heart strain. Little acute change from baseline.
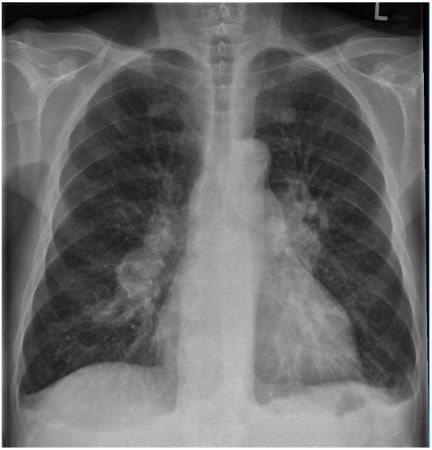
Portable CXR
CXR from 3 months prior
CXR interpretation: Suspect right middle/lower lobe infiltrate.
What factors must be considered when treating this patient with shock and respiratory failure given their history of pulmonary hypertension and right heart failure?
The management of patients with pulmonary hypertension is highly specialized. The unique pathophysiology needs to be understood if the clinician is going to manage this patient safely until they reach their pulmonary hypertension specialist.
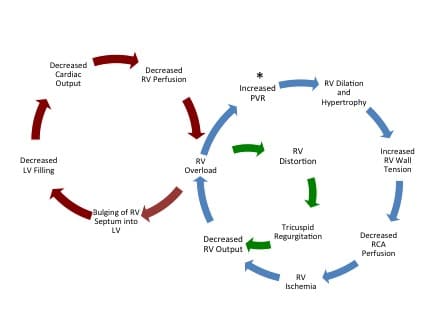
Pulmonary hypertension is most often encountered in the ED in patients with left heart failure or severe COPD. It is defined as an elevated pulmonary artery pressure > 25 mmHg. The pulmonary circulation is normally a low pressure, low resistance circuit. Elevated pulmonary artery pressure causes the right ventricle to dilate and eventually hypertrophy. Initially, via the Frank-Starling mechanism, the RV is able to increase stroke volume in response to increased pulmonary arterial pressure and maintain cardiac output. However, beyond a certain point, the right ventricle is no longer able to compensate, which causes elevated right ventricular filling pressures, decreased cardiac output and overt signs of right heart failure. The dilatation and hypertrophy of the right ventricle in attempt to compensate for elevated pulmonary pressure has two crucial implications that ultimately reduce cardiac output:
As the right ventricular dilates, it causes bowing into the left ventricle which decreases left ventricular filling and decreases cardiac output (termed interventricular dependence).
Progressive dilation of the right ventricle causes distortion of the tricuspid valve with causes regurgitation and further decreases right ventricular cardiac output.

From Wilcox et al. 2015
Finally, understanding right ventricular perfusion is necessary to appropriately manage these patients. Unlike the left ventricle which is perfused during diastole, the right ventricle is a lower pressure system and is normally perfused via the right coronary artery (RCA) during both systole and diastole. However, in pulmonary hypertension, RCA perfusion decreases proportionally to increases in right ventricular pressure. If pulmonary artery pressure surpasses systemic pressure, the right ventricle becomes ischemic, further decreasing RV contractility, increasing RV pressure and further limiting blood flow. This causes a spiral of depicted below.
PATIENTS WITH PULMONARY HYPERTENSION WALK A FINE LINE BETWEEN PULMONARY AND SYSTEMIC BLOOD PRESSURE. LARGE FLUID BOLUSES AND ATTEMPTS AT INTUBATION MAY CAUSE CARDIOVASCULAR COLLAPSE.
What are possible causes of this pulmonary hypertension patient’s decompensation?
Any condition that will cause a decrease in systemic blood pressure, increase in pulmonary arterial pressure or a combination thereof can cause an acute decompensation in these patients and initiate the death spiral of death.
| Increase in Pulmonary Artery Pressure | Decrease in Right Ventricular Perfusion/Oxygenation |
|---|---|
| Pulmonary embolus
COPD exacerbation Hypoxia (i.e. from pneumonia) Interruption of pulmonary vasodilator therapy |
Sepsis
Hypovolemia Anemia |
ALWAYS INSPECT THE PUMP AS ANY INTERRUPTION IN VASODILATOR THERAPY CAN BE LIFE-THREATENING
Patients with pulmonary arterial hypertension will often be taking multiple pulmonary vasodilator medications. There must never be an interruption in these treatments while under our care as they can cause a rebound elevation in pulmonary artery pressures. This patient is on an infusion of epoprostenol, prostacyclin analogue and pulmonary vasodilator. Pump malfunction can cause a rebound elevation in pulmonary artery pressures and must be immediately inspected. If there is any concern regarding a possible pump malfunction, an IV infusion at the same dose should be started immediately.
The CXR in this case suggests a possible right sided infiltrate. Pneumonia complicated by sepsis will have the following deleterious effects:
Hypoxia and hypercapnea cause pulmonary vasoconstriction, increasing right ventricular pressure
Systemic vasodilation from sepsis decrease right ventricular perfusion and further decrease right ventricular cardiac output
Give broad spectrum antibiotics. Pulmonary hypertension patients with sepsis often have a bowel source of bacteremia due compromised intestinal barrier function from poor cardiac output and high venous pressures.
Case continued…
Based on the initial investigations, the patient is treated for a presumed pneumonia with ceftriaxone, vancomycin, and azithromycin. A 250 cc normal saline bolus is given.
How will you optimize this patient’s oxygenation?
As mentioned, RV failure patients are very sensitive to hypoxia and hypercapnea due to associated pulmonary arterial vasoconstriction and resultant increase in RV pressure. Deliver high flow (15L) oxygen via a non-rebreather. High flow oxygen via nasal cannula concomitantly may further increase your Fi02 (see Critcases 6 on optimizing preoxygenation). If this is not sufficient, non-invasive positive pressure ventilation (NIPPV) may be an option. Because these patients are very sensitive to increase pulmonary artery pressures, you should start NIPPV at the lowest pressure possible and monitored closely for decompensation.
Does this patient need more IV fluids?
No. In a patient with hypotension and a normal RV, 1-2 L of NS bolus will often be adequately tolerated and will likely be beneficial. In a patient with acutely decompensated RV function, large fluid boluses will worsen RV dilatation, cause further compression of the left ventricle precipitating decreased cardiac output and cardiovascular collapse.
On physical exam, this patient has pitting edema and signs of volume overload. Bedside ultrasound is often an excellent tool to assess fluid tolerance in the shock patient, but in this case will likely not be helpful in assessment of volume status, as PAH patients will almost always have a dilated IVC due to elevated right ventricular pressures. Patients with right heart failure have a RV:LV > 1 (normal is < 0.6) and there will often be a thickened right ventricular wall secondary to chronic pulmonary hypertension.
Case continued…
You arrive at the community hospital. The patient has received a 250 cc normal saline bolus. Blood pressure is now 70/40, heart rate 100, oxygen saturation 86% on 15 L via a non-rebreather and 15 L via nasal cannula. This patient needs transfer to the tertiary centre but is decompensating hemodynamically.
What inotropic/vasopressor agent will you start prior to transport?
With a recent ECHO that shows an RVSP of 80 and a BP of 91/51 I can guarantee that the RV is essentially getting no perfusion and is severely ischemic (Aortic pressure – PA pressure = RV perfusion during systole and diastole). With that in mind it is essential that we give some norepinephrine peripherally to increase the SVR and allow for RV coronary perfusion.
-Dr. Marc N. Francis MD, FRCPC
The ideal hemodynamic agent would increase cardiac output, maintain SVR and decrease pulmonary vascular resistance (PVR). This agent does not exist. Most experts advocate starting with a vasopressor then adding an inotrope, given that most inotropes can cause decrease SVR (which will decrease right ventricular perfusion).
Vasopressors
Norepinephrine
As per previous Critcases, norepinephrine is becoming the universal first line agent for shock in the emergency department. It will increase systemic vascular resistance, which will increase right ventricular perfusion and has some Beta-1 effect that can provide some augmentation of inotropy. Unfortunately, it will also increase pulmonary vascular resistance. However, if there is any component of distributive shock, such as in this patient where sepsis is a consideration, norepinephrine would be a sound first line choice.
Vasopressin
Often used as an adjunct to increase SVR following norepinephrine, vasopressin could be used as a first line pressor in right heart failure patients as it will increase SVR but decrease pulmonary vascular resistance by a nitric oxide mechanism.
Phenylephrine
Essentially contra-indicated due its potent pulmonary vasoconstriction effects.
Inotropes
Dobutamine
While an excellent Beta-1 agonist that will increase cardiac output, dobutamine can cause tachycardia and systemic vasodilation. As such, it should not be started until a vasopressor is running.
Milrinone
A phosphodiesterase inhibitor, milrinone will increase contractility and peripheral arterial and venous vasodilation. As such, it has similar properties to dobutamine.
Epinephrine
Epinephrine’s strong Beta-1 stimulation will increase cardiac output and will not cause systemic vasodilation. However, it may be more likely to cause tachydysrythmias, which are poorly tolerated in right heart failure due to their effect on ventricular filling time.
Case continued…
The patient remains hypoxic at 88% on CPAP and now trending downward. The tertiary care center is awaiting transfer of the patient. You decide to intubate the patient prior to transfer.
How will proceed with intubation in this patient with pulmonary hypertension?
In pulmonary hypertension with RV failure, intubation must be seen as an absolute last resort.
This is because:
Sedatives used for RSI will cause hypotension which worsen RV ischemia
Transient hypoxia and hypercapnea will worsen pulmonary vasoconstriction, increase pulmonary artery pressure and RV ventricular pressures
Positive pressure ventilation will further increase pulmonary artery pressures and right ventricular pressure
The combination of the above factors can precipitate almost immediate decline in cardiac output and cardiac arrest.
Some experts will advocate for an awake intubation to prevent the systemic hypotension from sedative medications as well as the hypercapnea that may result from the apneic period. Alternatively, ketamine can be considered without the use of a paralytic as it will maintain respiratory drive. If RSI is to be used, avoid propofol due to risk of hypotension and instead consider etomidate in addition to a paralytic agent.
What is your ventilation strategy in the patient with pulmonary hypertension?
Given the drawbacks of increased intrathoracic pressure, you should aim for low tidal volumes (6-8 ml/kg ideal body weight) and low plateau pressures (< 30 mmHg). Minimal PEEP should be used (< 12 cm H20). Unlike an ARDS protocol for ventilation, these patients cannot tolerate permissive hypercapnea and hypoxia due to pulmonary vasoconstriction.
Case continued…
While en route, the patient develops atrial fibrillation with rapid ventricular response at a rate of 140 bpm.
What is your immediate next step?
These patients tolerate tachycardia poorly due to decreased ventricular filling time and cardiac output. They rely on atrioventricular synchrony to maintain cardiac output. The patient needs an immediate rhythm control strategy. Provide minimal sedation and cardiovert immediately.
Case continued…
You arrive at the tertiary centre and the patient is transferred to the ICU under the care of their pulmonary hypertension specialist.
What are the implications if this pulmonary hypertension patient were to have a cardiac arrest?
Patients with pulmonary hypertension and right heart failure who suffer cardiac arrest have an extremely poor prognosis. CPR in the event of a cardiac arrest is essentially futile given the obstructive physiology of severe pulmonary hypertension. Of course, patient and family wishes need to be incorporated into decision making.
What other treatments are potentially available at a tertiary center for these pulmonary hypertension patients?
Failing inotropic and vasopressor support, these patients may require inhaled pulmonary vasodilator therapies, likely unavailable in a community hospital. Inhaled nitric oxide or inhaled epoprostenol provide pulmonary vasodilation while limiting systemic hypotension. Additionally, they may help to correct V/Q mismatch by preferentially vasodilating pulmonary arteries perfusing well ventilated lung. ECMO would remove deoxygenated blood from the venous system and restore oxygenated blood to the arterial system, which would benefit both right and left ventricular dysfunction as well as improve oxygenation.
Case Resolution
The patient receives maximal inotropic support, inhaled epoprostenol and aggressive treatment of sepsis secondary to presumed pneumonia. Unfortunately, the patient continues to deteriorate. Given the severity of the patient’s disease burden and the potential harm of more aggressive measures, the patient and family decide to pursue comfort measures and the patient expires.
Take Home Points for Pulmonary Hypertension
- Patients with severe pulmonary hypertension walk a fine line between pulmonary and systemic blood pressure. They require judicious fluid volume resuscitation. Avoid positive pressure ventilation if possible.
- Aggressively search for the underlying cause of decompensation, with a low threshold to start broad-spectrum antibiotics.
- Do not allow vasodilator therapy to be interrupted while the patient is under your care.
- Norepinephrine or vasopressin followed by an inotrope is reasonable to manage the patient’s hemodynamics.
- Tachycardia is poorly tolerated in pulmonary hypertension. Immediate cardioversion of tachydysrythmias is required.
- Intubating a patient with pulmonary hypertension is a last resort. Consider awake intubation. Avoid prolonged apnea or over sedation.
- Cardiac arrest in the context of pulmonary hypertension has a very poor prognosis. CPR is futile as the patient demonstrates obstructive physiology.
- Involve the patient’s pulmonary hypertension specialist and arrange transfer to a specialized center early in the care of these patients.
Expert Peer Review by Susan Wilcox
Resuscitation of the critically ill pulmonary hypertension patient is challenging not only because these patients have little physiologic reserve, but also because the standard principles of critical care do not apply. The foundational aspects of resuscitation, including early intubation, positive pressure ventilation, and aggressive fluid resuscitation, can 
Optimizing RV preload
In considering the preload, these patients are far more likely to be volume overloaded than dry. Unless there is compelling evidence that the patient is volume depleted, avoiding IV fluids is advisable. If there is strong suspicion for a volume responsive state, boluses should be 250mLs followed by close reassessment. Bedside ultrasound is useful in confirming RV overload but is not often helpful in assessing volume responsiveness in patients with long-standing pulmonary hypertension in extremis. A patient in respiratory distress may generate substantial negative intrathoracic pressures, leading to variation in the IVC despite not being volume-responsive.
Pulmonary artery catheters are rarely used in critical care, however, following cardiac output in patients with pulmonary hypertension is one of the few indications for PA line placement. These patients often benefit from diuresis with a paradoxical increase in cardiac output after decreasing RV volume overload. Because giving diuretics in patients with preexisting hypotension can be daunting, PA line monitoring can provide reassurance that this is the correct intervention.
Maximizing contractility
Systemic hypotension is detrimental in pulmonary hypertension because the RV relies upon a strong gradient between the pressure in the right coronary artery and the RV transmural pressure to maintain perfusion. With hypotension, the RV can become ischemic, leading to poor contractility, worsening volume overload, and decreased LV filling. Therefore, maximizing contractility means adding vasopressors to maintain RV perfusion as well as subsequent addition of inotropes. While norepinephrine is a first line agent, vasopressin is an excellent alternative or adjunct to maintain systemic vascular resistance without increasing pulmonary vascular resistance or tachycardia. Once the SVR is maintained, an inotrope of milrinone or dobutamine should be added.
Minimizing RV afterload
To minimize the RV’s afterload, hypoxia and hypercarbia must be avoided, and high flow oxygen, if available, is an excellent therapy to that end. A non-rebreather mask can provide about 15L/min of flow, but high flow oxygen can provide up to 60L/min, an important distinction for patients with high minute ventilation. If intubation is unavoidable, empirically starting norepinephrine to maintain SVR and provide a modicum of ionotropic support prior to intubation is advisable. Push-dose phenylephrine, sometimes used in emergency intubations, should be avoided in favor of other vasopressors and inotropes.
Initiation or titration of intravenous pulmonary vasodilators like epoprostenol should only be done by a pulmonary hypertension specialist in a closely monitored setting. Inhaled pulmonary vasodilators are more forgiving, with less risk of systemic hypotension and hypoxemia, but also are less potent in their effects on the PVR.
Patients in the ED often miss medications, but patients should never miss their pulmonary vasodilators. If the patient is on oral medications and must be NPO, the patient’s pulmonary hypertension specialist should be contacted immediately to discuss an alternative plan. Calling the pulmonary hypertension specialist as soon as the patient presents to the ED is always appropriate. If the patient’s doctor cannot be reached, speaking with a Pulmonologist or Medical Intensivist at a tertiary care center is the next best option.
References
Buckley MS, Feldman JP. Inhaled epoprostenol for the treatment of pulmonary arterial hypertension in critically ill adults. Pharmacotherapy. 2010;30(7):728-40.
Hoeper MM, Galié N, Murali S, et al. Outcome after cardiopulmonary resuscitation in patients with pulmonary arterial hypertension. Am J Respir Crit Care Med. 2002;165(3):341-4.
Hoeper MM, Granton J. Intensive care unit management of patients with severe pulmonary hypertension and right heart failure. Am J Respir Crit Care Med. 2011;184(10):1114-24.
Green EM, Givertz MM. Management of acute right ventricular failure in the intensive care unit. Curr Heart Fail Rep. 2012;9(3):228-35.
Price LC, Wort SJ, Finney SJ, Marino PS, Brett SJ. Pulmonary vascular and right ventricular dysfunction in adult critical care: current and emerging options for management: a systematic literature review. Crit Care. 2010;14(5):R169.
Tongers J, Schwerdtfeger B, Klein G, et al. Incidence and clinical relevance of supraventricular tachyarrhythmias in pulmonary hypertension. Am Heart J. 2007;153(1):127-32.
Ventetuolo CE, Klinger JR. Management of acute right ventricular failure in the intensive care unit. Ann Am Thorac Soc. 2014;11(5):811-22.
Wilcox SR, Kabrhel C, Channick RN. Pulmonary Hypertension and Right Ventricular Failure in Emergency Medicine. Ann Emerg Med. 2015;66(6):619-28.





simply fantastic post – so vital to know how to manage sick patients with Sev Pulm HTN coming to ED, not very common, need a totally different approach to usual, can easily be harmed by lack of proper understanding of this patho- physiology.
Not as uncommon as we think. Once you start echoing patients in ED you will realise soon how frequently it is encountered. Early echo in all hypotensive patients is critical. If there is suggestion of pulmonary hypertension you have the clinical paradigm of “hypertensive hypotension”.
In Moderate to severe pulmonary hypertension septic shock has near 70-80% mortality and Goals of care should be considered immediately.
Fabulous article and I feel we ought to identifying these early in ED much before RV failure is imminent. We will continue to see a rise of Type II and type III pulmonary hypertension.
Hello! Thank you so much for this information and spreading awareness of these very fragile pulmonary hypertension patients.
The case study says patient is on Remodulin which is treprostinil (not epoprostenol). Could help to distinguish the significant half-life differences between these 2 drugs (4 hrs for treprostinil vs less than 6 minutes for epoprostenol).
Thanks again! Great guide for emergency management!